
It is estimated that almost 8% of the US population has diabetes, with another 57 million having pre-diabetes (Hammaker, 2014). There is also a rise in Alzheimer’s disease (AD), and some researchers are exploring its possible relationship to the aforementioned metabolic disease. As a means of appreciating the pathogenesis of AD, the following will explore insulin resistance, diabetes, and it connection to memory loss and cognition.
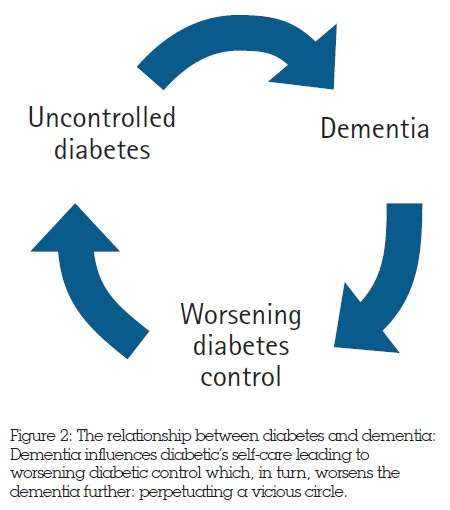
Hammaker (2014) noted studies among the elderly in which a pattern was uncovered; elderly subjects who developed AD also had type 2 diabetes (T2D), in addition to having twice the risk of developing dementia. Hammaker (2014) also cited a diabetes prevalence study, indicating that many elderly individuals exhibited a high rate of diabetes (33% of total subjects) while other subjects had impaired fasting glucose (75%). Finally, those individuals who took insulin had a higher risk of developing dementia (Hammaker, 2014). Such coexistence and high rates of insulin resistance, diabetes, and AD among the elderly is, at minimum, suspect.
Post-mortem tissue studies of individuals with AD uncovered an intriguing finding; patients with AD had 80% fewer insulin receptors than those individuals who did not have AD (Hammaker, 2014). Furthermore, there were certain areas of the brain that had higher concentrations of insulin receptors in non-AD individuals; the olfactory bulb, pre-frontal cerebral cortex, hypothalamus, cerebellum, and choroid plexus. Such findings may appear trivial, initially. However, said brain regions are associated with memory and logic (Hammaker, 2014). Such anatomical and physiological findings build a case for a strong relationship between insulin and cognitive processes. The following section will consider the same in greater detail.
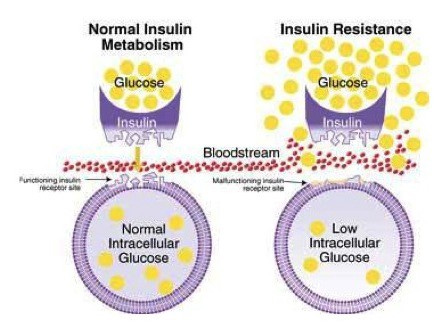
There exists a mechanistic relationship between insulin, brain tissue, and function. Studies have supported the role of insulin stimulating acetylcholine; a neurotransmitter responsible for cognition and the formation of memories (Hammaker, 2014). Individuals with brain-based insulin resistance tend to develop attentional processing dysregulation. Furthermore, since the brain is not absorbing glucose, hyperglycemia ensues; a process thought to increase oxidative stress (Hammaker, 2014). Such a process can also reduce acetylcholine production, causing aberrations in memory formation, in addition to forming beta-amyloid plaques (which kill neurons) within cerebral blood vessels (Hammaker, 2014). Interestingly, beta-amyloid plaques are also found in the pancreas of individuals with T2D; a characteristic shared by AD and T2D.

In conclusion, brain-based insulin resistance and hyperglycemia can occur in patients before AD progresses, allowing said symptoms to act as an early warning sign. Furthermore, such knowledge helps one appreciate the mechanistic roles of insulin resistance and hyperglycemia in the formation and progression of AD. Most importantly, since the risk of AD is higher in those with T2D, such facts should prompt medical professionals to take preventative measures before neurological symptoms worsen.
References
Hammaker, B. G. (2014). More than a coincidence: Could Alzheimer’s disease actually be a type 3 diabetes? Journal of Diabetes Science and Technology, 28(9), 16-18.
-Michael McIsaac
