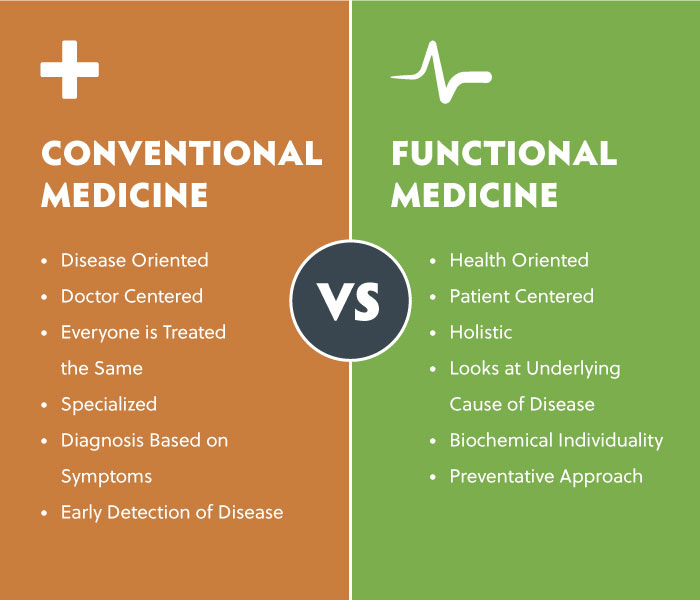
Conventional medicine can be thought of as a system in which medical doctors and other healthcare professionals treat symptoms and diseases using drugs, radiation, or surgery (National Cancer Institute, 2018). Functional medicine (FM) is an emerging model, which considers the underlying cause of disease and symptoms in its effort to restore an individual’s homeostasis (Kresser Institute, 2018). FM is grounded in evidence-based medicine yet considers the inexorable relationships between organs and the human body as a whole (Kresser Institute, 2018). As a means of appreciating the utility of FM, the following sections will consider the nature of Alzheimer’s disease (AD) and potential solutions to mitigate and manage said ailment.
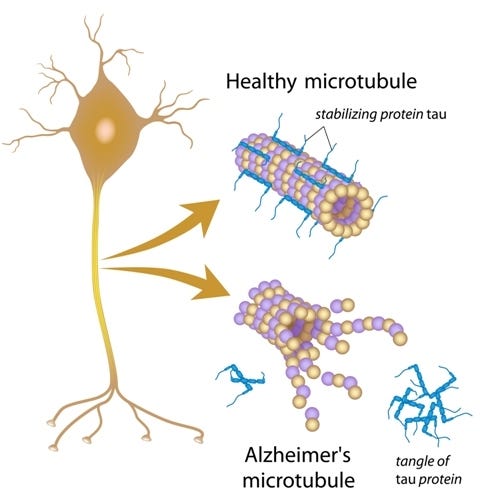
AD is the sixth leading cause of death in the Unites States, with 5.4 million Americans suffering from the disease (Kandimalla, Thirumala, & Reddy, 2017). AD is characterized by the development of two abnormal proteins in the brain known as β-amyloid and tau, which are toxic to nerve cells within the brain (Jin, 2015). The build-up of such proteins inexorably leads to neuron death, degraded brain function, and manifestations of dementia; a term, which describes a decline in mental abilities including language, memory, and logical thinking (Jin, 2015). The precise trigger for AD remains elusive yet it tends to run in families indicating a genetic driver. Jin (2015) indicated that there are 30 genes that might be involved in AD, three of which are passed down from parent to child. Half of the children of an affected parent are likely to develop AD (Jin, 2015).
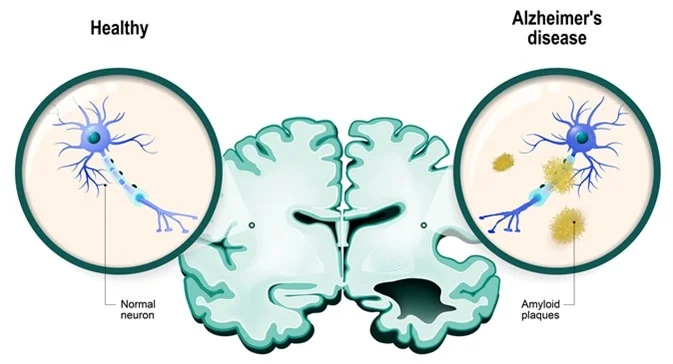
Symptoms of mild AD can include deficits with memory of more recent events, getting lost in a familiar place, misplacing items, trouble completing complex tasks, and mood and personality changes (Jin 2015). Symptoms of moderate AD include worsened memory loss and confusion, poorer mood and personality changes, which could include paranoia, hostility, inability to recognize family members and friends, and requiring help with activities such as getting dressed or going to the bathroom (Jin 2015). Symptoms of severe AD are marked by an inability to speak and complete dependence on others for all day-to-day activities (Jin, 2015). Jin (2015) indicated that conventional medicine currently treats AD symptoms with medications that can slow the advancement of the disease but cannot reverse it. At best, other medications are used to treat systemic problems from AD such as sleep, anxiety, or depression. Having considered the indicators of AD (both physiological and behavioral manifestations), the following will explore how FM can help manage/mitigate the root cause of AD.
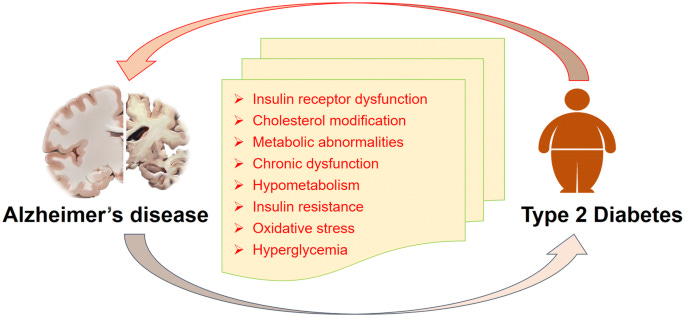
T2D is characterized by hyperglycaemia, insulin resistance, and hyperinsulinemia (Kandimalla et al., 2017). Such conditions arise due to a reduced sensitivity of muscle, liver and fat cells to insulin (also called insulin resistance). Kandimalla et al. (2017) noted that immediately after the meal the pancreas increases insulin production, which targets adipose tissue, skeletal muscle, liver, and fat (Kandimalla et al., 2017). Insulin triggers the uptake of glucose from the blood and promotes glycogenesis by inhibiting glucose production (Kandimalla et al., 2017). Substantial research, from epidemiological studies, has emerged indicating that type 2 diabetes mellitus (T2D) is strongly associated with cognitive impairment (Kandimalla et al., 2017). Such a physiological aberration is due to a failure of glucose to absorb into the neurons for energy production; another key tissue that insulin interacts with (Kandimalla et al., 2017). Thus, individuals with hyperglycemia and insulin resistance (IR) (characteristics of T2D) are likely to develop AD and can be considered a risk factor.
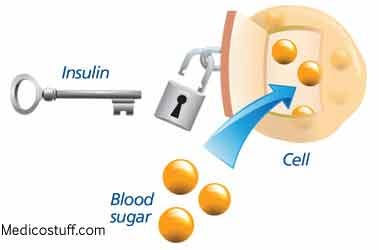
IR within the brain has been associated with an unfavorable cascade of biochemical and physiological events. Research has suggested that AD represents a metabolic disease and has indicated that deficits in utilization of glucose by the brain in the early course of disease eventually lead to the cognitive dysfunction (Kandimalla et al., 2017). Interestingly, patients with AD had 80% fewer insulin receptors compared to other individuals who did not have AD (Hammaker, 2014). Additionally, the pre-frontal cerebral cortex, choroid plexus, olfactory bulb, hypothalamus, and cerebellum had the greatest deficit of insulin receptors; regions responsible for memory and logic (Hammaker, 2014). Considering that IR, hyperglycaemia, and a lack of insulin receptors are hallmarks and drivers of AD (uncovering the source of the disease, which is a FM approach) the following will explore how a FM paradigm might help those afflicted with said metabolic disease.
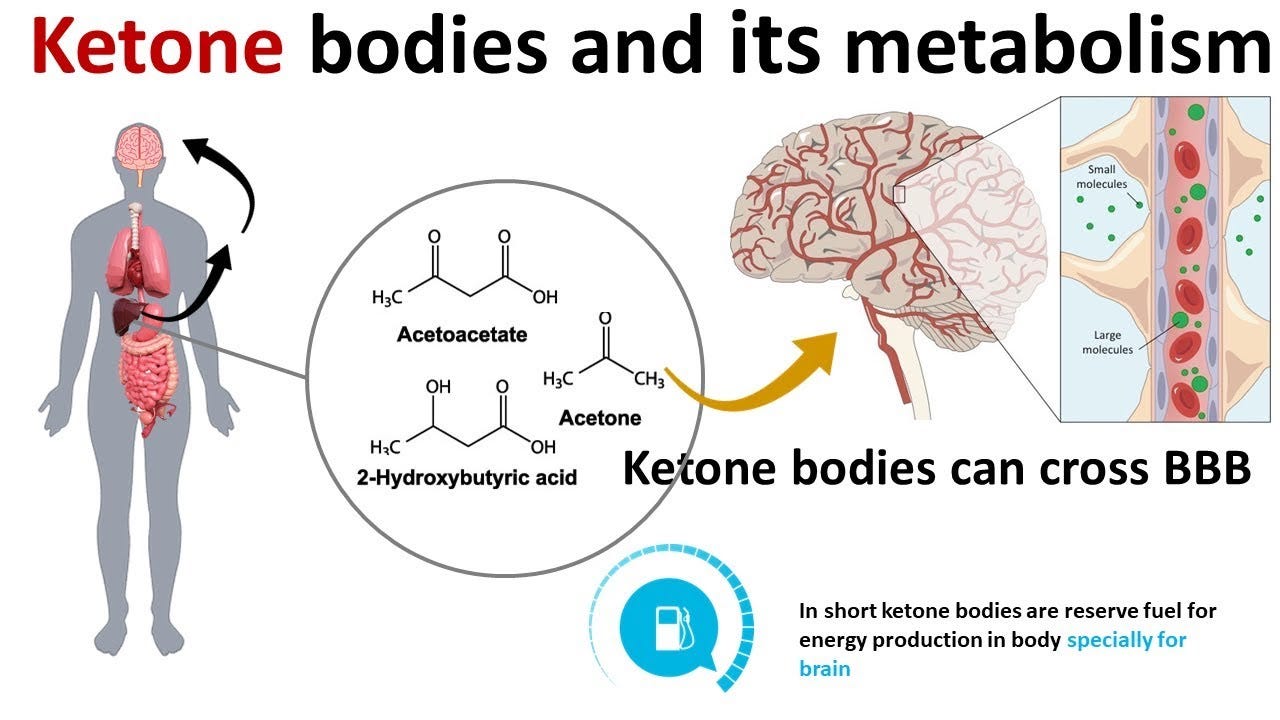
The adult brain requires a relatively large energy supply; the brain represents approximately 2% of total bodyweight while consuming approximately 20–23% of whole-body energy requirements, predominantly in the form of glucose (Cunnane et al., 2016). During starvation, fasting, or strenuous exercise, the brain is capable of utilizing an alternate energy source known as ketone bodies (KBs): acetone, acetoacetate (ACAC), and beta-hydroxybutyrate (BHB) (Cunnane et al., 2016). The most widely metabolized KBs of the three produced are ACAC and BHB, and said energy substrates are thought to circumvent aberrations in glucose metabolism (Cunnane et al., 2016). The following sections will explore how KBs can help mitigate the root cause of AD.
During ketosis (the process of producing KBs), Cunnane et al. (2016) stated that the body can produce KBs (in the liver) at a rate of 100-150g/day, a level considered sufficient to provide energy to the brain in place of glucose. Paoli, Rubini, Volek, and Grimaldi (2013) stated that approximately after 72-96 hours, cells move from using glucose as a primary substrate to triglycerides, which are biochemically converted into ketones (Paoli et al., 2013).
Paoli et al. (2013) also noted that ketosis is achieved through minimizing the ingestion of starchy carbohydrates to less than 50 grams/day in order to induce a change in substrate utilization by lowering insulin secretion and increasing lipolysis (triglyceride breakdown and release from adipose tissue).
Furthermore, supplementing the diet with additional fats also helps provide triglycerides for ketosis; medium chain triglycerides (MCT) from coconut oil have been particularly beneficial to individuals with AD as they are in a form that can enter the liver and convert to KBs in an expeditious fashion (Cunnane et al., 2016). Finally, Cunnane et al. (2013) stated that MCT doses of up to 1g/kg/day had a large safety record in all species, including humans.
By applying a FM model, identifying the mechanisms of T2D and AD, uncovering their relationships, and implementing a ketogenic diet, research has indicated that such an inclusive approach has shown to sustain normal brain function in those with poorly regulated blood glucose and early stages of AD (Cunnane et al., 2016). Although this author’s review of AD and ketosis is not extensive (i.e., physical activity has also been shown to help regulate mood and memory in those with AD), it does, however, demonstrate the relevance of identifying the genesis of symptoms as a starting point for treatment rather that treating the symptoms itself.
References
Cunnane, S., C., Courchesne-Loyer, A., St-Pierre, V., Vandenberghe, C., Pierrotti, T., Fortier, … Castellano, C. A. (2016). Can ketones compensate for deteriorating brain glucose uptake during aging? Implications for the risk and treatment of Alzheimer’s disease. Annals of the New York Academy of Sciences, 13671(1), 12-20.
Hammaker, B. G. (2014). More than a coincidence: Could Alzheimer’s disease actually be a type 3 diabetes? Journal of Diabetes Science and technology, 28(9), 16-18.
Jin, J. (2015). Alzheimer disease. JAMA, 313(14), 1488.
Kandimalla, R., Thirumala, V., & Reddy, P. H. (2017). Is Alzheimer’s disease a type 3 diabetes? Molecular Basis of Disease, 1863(5), 1078-1089.
Kresser Institute (2018). Functional medicine. Retrieved from https://kresserinstitute.com/category/functional-medicine/
National Cancer Institute (2018). Western medicine. Retrieved from https://www.cancer.gov/publications/dictionaries/cancer-terms/def/conventional-medicine
Paoli, A., Rubini, A., Volek, J. S., & Grimaldi, K. A. (2013). Beyond weight loss: A review of the therapeutic uses of very low-carbohydrate (ketogenic) diets. European Journal of Clinical Nutrition, 67, 789-796.
-Michael McIsaac
