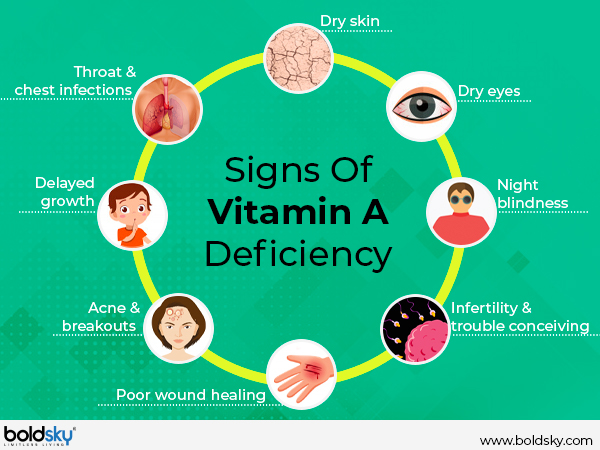
In less developed countries, vitamin A deficiency (in conjunction to protein, iron, and iodine deficiency) are the leading causes of child deaths worldwide (Vijayaraghavan, 2000). Early signs of said deficiency can express itself as xerophthalmia (dryness of eyes), nyctalopia (night blindness), and dry skin (Gropper, Smith, & Carr, 2018). Although such signs can prompt one to seek supplementation to mitigate further complications of deficiency, caution must be implemented when introducing vitamin A to avoid toxicity. As a means of appreciating the need to cautiously supplement, the following will explore the same.
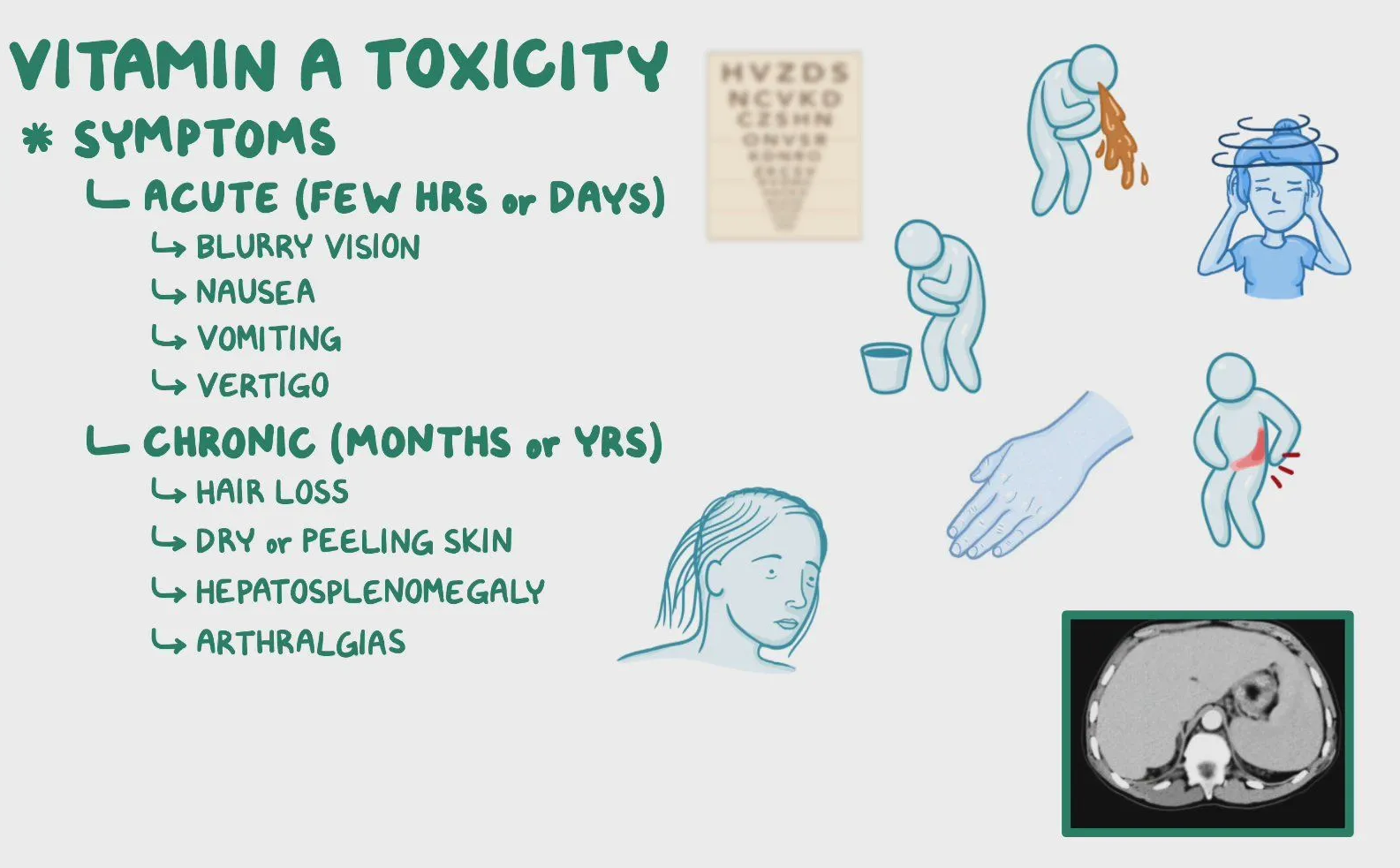
The tolerable upper intake level (UL) of vitamin A was stated by Gropper et al. (2018) as 10,000 IU/day, while 50,000 IU/day can induce a toxic state known as hypervitaminosis. Such symptoms of overconsumption of said vitamin can present as blurred vision, headache, nausea, vomiting, diarrhea, dizziness, muscle incoordination, and skin peeling (Allen & Haskell, 2002). Other conditions from overconsumption of vitamin A can include hair loss, while more severe side effects include decreased bone mineral density (BMD) (Gropper et al., 2018). BMD loss occurs from an early closure of epiphysial plates and excessive bone resorption (Gropper, et al, 2018). Such toxicity can also negatively affect other key systems, to include the liver.
The liver, according to Gropper et al. (2018), is the primary site of vitamin A storage. Normal concentrations of vitamin A within the liver is approximately 100 μg/g. However, plasma levels will rise when liver storage exceeds 300 μg/g; a level also thought to represent toxicity (Allen & Haskell, 2002).Excess vitamin A consumption has been reported to induce hyperplasia; a physiological state of excessive production of cells (Gropper et al., 2018). Vitamin A toxicity can also induce liver fibrogenesis (excessive formation of connective tissue), hypertrophy (growth of the liver), and sclerosis (stiffening) of veins (Allen & Haskell, 2002; Gropper et al., 2018). As such, it is crucial to consider appropriate and safe levels of vitamin A supplementation.
Vitamin A status can be measured in multiple fashions to include measuring plasma retinol (vitamin A). However, Gropper at al. (2018) indicated limitations in said protocol; plasma levels are a good indicator only if individuals have exhausted their stores (i.e., deficiency) or if liver stores are at capacity (i.e., toxicity). Such extremes exclude populations that often fall between such states. Another method thought to be more inclusive would be the relative dose response (RDR). Essentially, plasma levels of retinol are measured before and after an oral administration of vitamin A and placed in an equation thereafter. Said equation is 5-hour plasma retinol – initial plasma retinol divided by 5-hour plasma retinol concentration x 100 (Gropper et al., 2018). %RDR greater than or equal to 20% represents inadequate vitamin A liver stores (Groopper et al., 2018). Such a method would be useful in helping one avoid overconsumption of supplemental retinol.
In conclusion, vitamin A deficiency can occur in select populations leading to serious, and sometimes permanent, damage. However, it is imperative that when addressing said deficiency, caution is taken to avoid the extreme of supplementation; toxicity. Tests such as RDR could help in guiding individuals to appropriate levels of vitamin A consumption, thereby achieving optimal health and homeostasis in a safe and efficient manner.
References
Allen, L. A., & Haskell, M. (2002). Estimating the potential for vitamin A toxicity in women and young children. The Journal of Nutrition, 132(9), 2907-2919.
Gropper, S. S., Smith, J. L., & Carr, T. P. (2018). Advanced nutrition and human metabolism (7thed.). Boston, MA: Cengage Learning.
Penniston, K. L., & Tanumihardjo, S. A. (2003). Vitamin A in dietary supplements and fortified foods: Too much of a good thing? Journal of the American Dietetic Association, 103(9), 1185-1187.
Vijayaraghavan, K. (2000). Vitamin A deficiency. The Lancet Perspectives, 356, s41.
-Michael McIsaac
