Ligament strength is essential to maintaining joint stability, and prevention of injury. Collagen, a structural protein constituting 65%-80% of the dry weight of ligaments and tendons, provides the majority of functional integrity and framework, as seen on the anterior cruciate ligament (ACL) (Marumo, Saito, Yamagishi, & Fujii, 2005). Thus, finding a suitable tissue replacement for the ACL, which satisfies the loading requirements within the knee joint, is paramount. As a means of appreciating the constituents of collagen, and its role in ligament strength, the following will consider 3 harvested tissues (i.e., patellar, semitendinosus, and gracilis tendon) used in ACL reconstruction. Finally, this author will consider the concept of “ligamentization” as proposed by Marumo et al. (2005), and its impact on the strength of the reconstructed ACL.
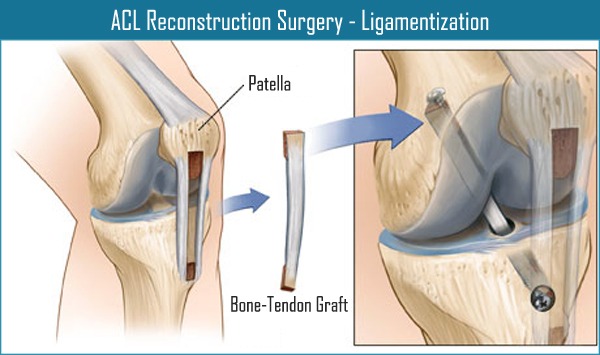
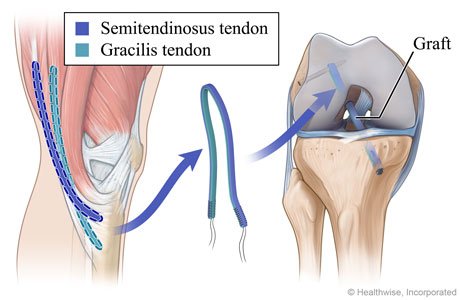
As mentioned in the aforementioned section, Marumo et al. (2005) considered the impact of different harvested tissues for ACL reconstruction. Throughout the structure of collagen, there exists a unique molecular coil with associated molecular crosslinks (Marumo et al., 2005). Such qualities allow collagen to exude tensile strength (i.e., resistance to elongation) and viscoelasticity (i.e., resistance to elongation with some extensibility, and a return to normal length after tensile loading) in tendons and ligaments (Delforge, 2002). The ACL requires high degrees of tensile strength. Thus it is relevant to consider differences between tendinous and ligamentous tissue; tendons have different collagen reducible crosslinks compared to ligaments, making them weaker (Marumo et al., 2005). However, bone-patellar tendon-bone (BPTB) and semitendinosus and gracilis (STG) autografts (i.e., tissue transplanted from one part of the body to another part in the same individual) tended to have enough similar morphologic, histologic, and biochemical similarities to make the harvested tissues viable options (Delforge, 2002; Marumo et al., 2005).
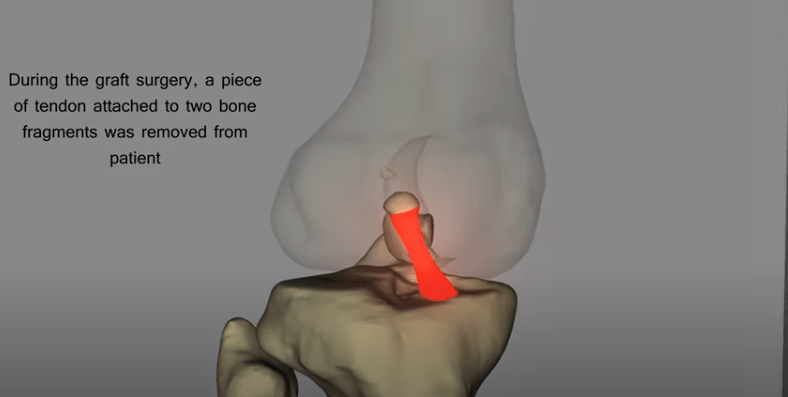
Marumo et al. (2005) noted that apparent differences between the morphology, histology, and biochemistry of a native ACL ligament and BPTB/STG became less clear as the autografts continued healing, up to a year post-surgery. The authors continued to explain that rabbit models implementing tendinous autografts underwent “ligamentization”; a process by, which biochemical and histological parameters change to reflect characteristics more akin to a ligament (Marumo, 2005). Having sampled 50 patients (30 patients in the BPTB group, and 20 patients in the STG group) who underwent ACL reconstructive surgery, findings indicated ligamentization within a year (Marumo, 2005). Results in both groups indicated collagen content increased within 1 year; STG collagen rose from 78.5% (measured 4-6 months post surgery) to as high as 92.2%, while the BPTG group was as high as 95.3%. It should be noted that collagen content in the BPTG group could not be assessed at the 4-6 month point post-surgery (Marumo, 2005).
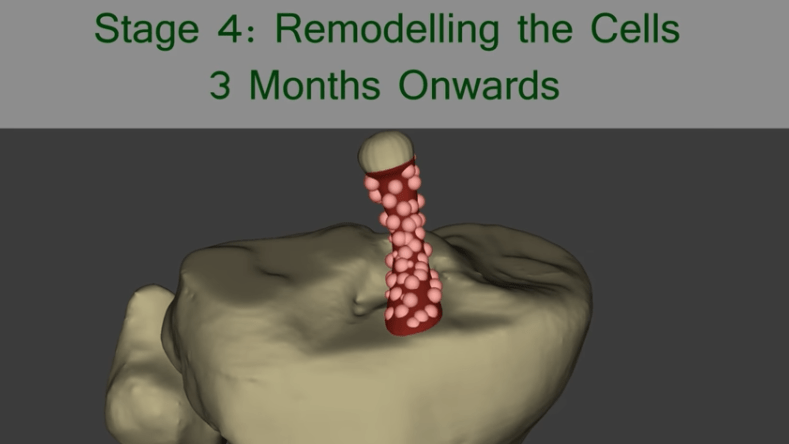
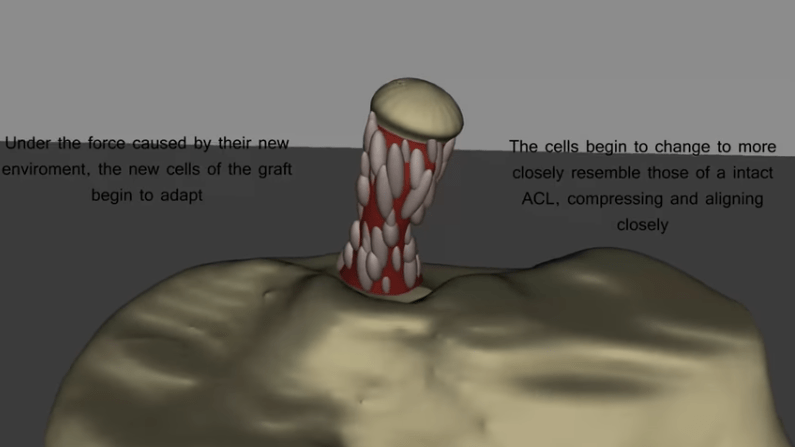
Knowledge of collagen, its constituents, and function has allowed this author to appreciate the vigilance required when choosing a tissue replacement for ligamentous reconstructive surgery. Additionally, awareness of the time required (i.e., up to a year) for an autograft to “ligamentize” also warrants caution regarding the time and place of exercise prescription, progressions, and return to play. Finally, such research reminds this author of the capacity of the human movement system to adapt, in the presence of change.
References
Delforge, G. (2002). Musculoskeletal trauma; Implications for sports injury management.Champaign, IL: Human Kinetics.
Marumo, K., Saito, M., Yamagishi, T., & Fujii, K. (2005). The “ligamentization” process in human anterior cruciate ligament reconstruction with autogenous patellar and hamstring tendons. A biochemical study. American Journal of Sports Medicine, 33(8), 1166-1173.
-Michael McIsaac
