As discussed in previous posts, the gastrointestinal tract (GIT) is an approximate 16-foot long organ system; a gateway facilitating immune function and entry of key macronutrients and micronutrients into the inner systems of the human body.1Approximately 30% of total daily caloric intake is devoted to the GIT in addition to a unique and independently working lymphatic and nervous system.1(416)As Bralley and Lord1(416) stated, such a devotion of resources implies the relevance and importance of the GIT in maintaining homeostasis. As a means of appreciating gut function and health, the following will explore proactive methods of assessing maldigestion, malabsorption, food allergies, and sensitivities.
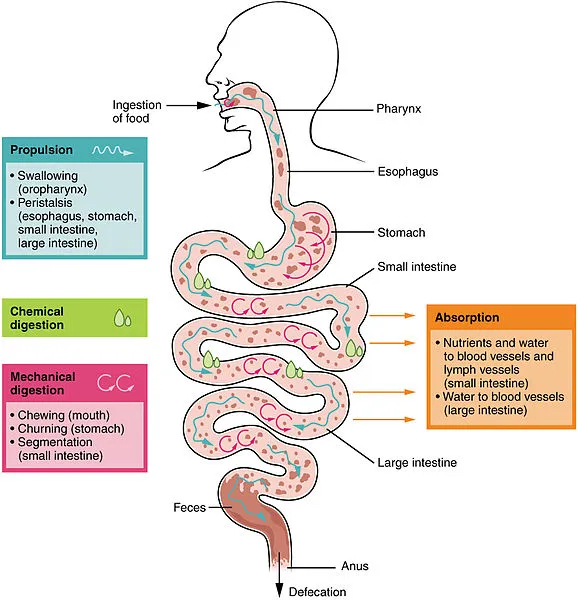
Digestion can be defined as chemical and mechanical methods of breaking down macronutrients such as carbohydrates, fats, and proteins into smaller molecules.1(422-423)Such processes use chewing (i.e., mechanical), hydrochloric acid (chemical), pancreatic juices (chemical), and liver bile (chemical) processes to achieve said end.1(422-423) When there are aberrations in the aforementioned mechanical and chemical processes, foods become inadequately broken down; a process known as maldigestion.1(422-423) As a consequence, maldigestion can then negatively impact the ability of the intestinal wall to absorb micronutrients, one process that can lead to compromised entry of nutrients (malabsorption) into the bloodstream from the GIT. Absorption of micronutrients is possible through an intricate and delicate process of accepting and separating micronutrients from harsh gastric juices, pancreatic enzymes, and pathogens.1(25) If said process incurs disruptions in function, absorption can become compromised in addition to a cascade of immunological events, nutrient depletions, and diseased states.1(425-426)Having briefly reviewed digestion and absorption, the following will explore tests that help identify inadequacies of both.
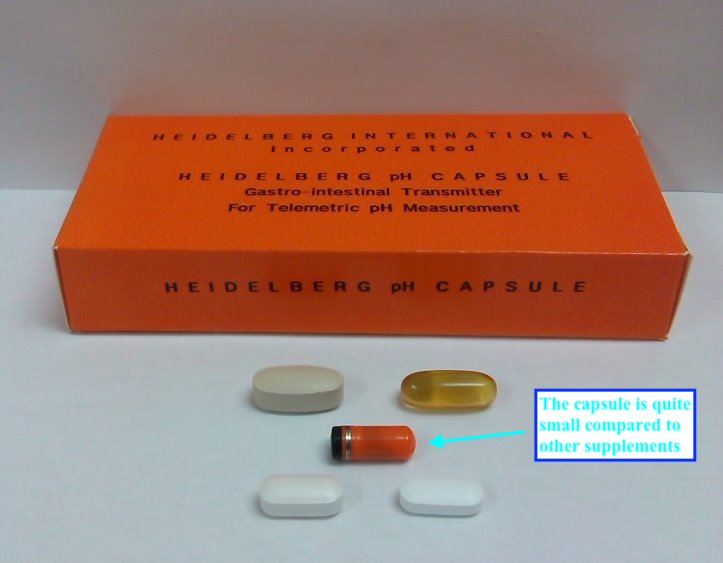
The stomach produces a strongly acidic substance known as hydrochloric acid (HCL); a secretion essential for the assimilation of minerals such as calcium and zinc, as well as the digestion of protein (in the presence of proteolytic enzymes) and sterilization of gastric contents1(418) One method of monitoring and assessing stomach acid is through the Heidelberg test. One such test is the Heidelberg capsule test.1(419).Although time consuming, the test requires approximately 90 minutes and is achieved by swallowing a small pH probe. As the probe passes along the GI tract, readings are gathered regarding pH (acidity) in different locations to include the stomach.1(419)Once baseline readings are gathered (normal stomach pH is 1-2), a challenge solution of sodium bicarbonate (high pH/high alkalinity) is consumed to rapidly increase stomach pH (alkalinity). If parietal cells (produce HCL) are functioning optimally, they will generally increase stomach acidity (lower pH) back to a pH of 1-2 within a 20 minutes period.1(419)If hypochloridria (low stomach acid) is present, reacidification of the stomach will require more than 20 minutes. Furthermore, Lord and Bralley1(420) indicated that concurrent measurement of micronutrients whose digestion and absorption are dependent upon high acidity (iron, zinc, copper, manganese) can also be measured to help confirm adequate stomach acidity, or lack thereof.
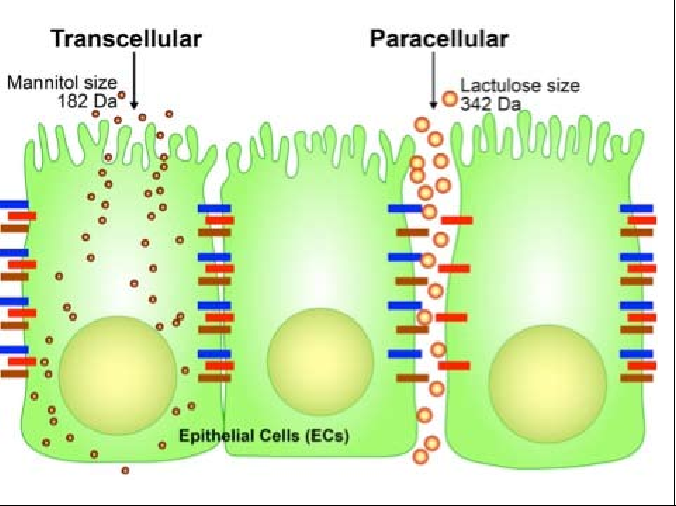
Absorption can be monitored via multiple tests to include the lactulose-mannitol protocol (LMP). The LMP was implemented to measure intestinal hyperpermeability; a condition found in all inflammatory bowel diseases. Furthermore, hyperpermeability (entry of larger undigested particles) has also been linked to food sensitivities and pancreatitis.1(426)As such, awareness of its presence is relevant in monitoring, tracking, and managing pathophysiology of said conditions. The LMP is a test which uses a direct measure of hyperpermeability to the disaccharide lactulose. The LMP is a challenge test in which patients consume 5 grams of lactulose/mannitol. Since said sugars are not metabolized, the human body summarily excretes them into the urine within 6 hours.1(426) Of note is that mannitol is generally absorbed through the GIT in a passive fashion. However, lactulose is usually not absorbed unless the mucosal barrier becomes dysregulated.1(426) Therefore, a calculation can be used in which a comparison can be made between the percent absorption of mannitol and lactulose. A normal ratio of mannitol to lactulose is <0.3.1(426) Thus, elevated ratios indicate lactulose was absorbed suggesting leaky gut syndrome and malabsorption issues.
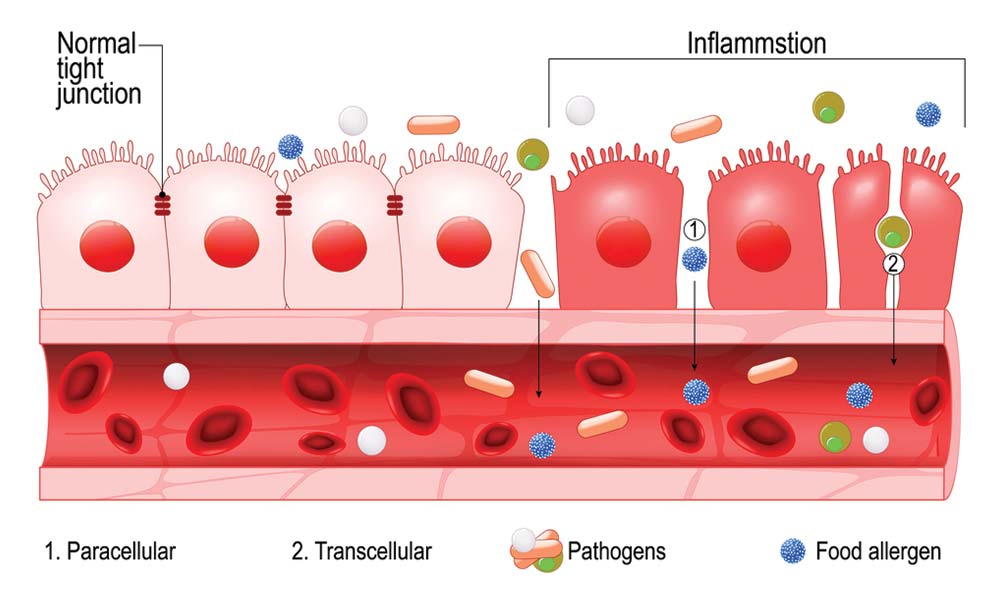
Dysregulation of digestion and absorption processes not only induce inflammatory cascades and nutrient deficiencies; aberrations in gut function can also become the progenitor of food sensitivities and food allergies. Innate and acquired immunity are processes along the intestinal mucosal barrier which help reduce entry of pathogens into the bloodstream. Such regions of the intestine are replete with gut associated lymphoid tissue (GALT) which provides antibodies and other responses to eradicate pathogenic invasions.1(430)2 When the recognition and control of pathogens fail followed by subsequent penetration past the mucosal barrier, GALT can induce powerful inflammatory processes.1(427)Furthermore, any loss or breach in barrier function maintained by tight junctions can also allow for antigen/undigested food molecule entry and further immune responses.1(430)Such conditions encourage an immune response towards the presence of foods, ultimately leading to sensitivities and allergies.1(430) Therefore, the following will categorize major classes of immune responses to foods.
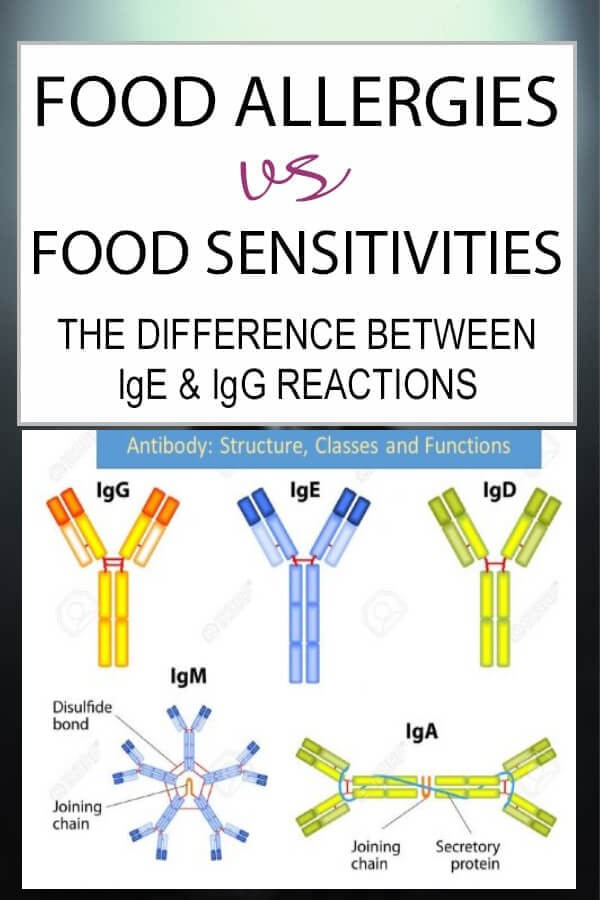
Food allergies can be defined as an immune response directed by basophil (innate) or mast cell (innate) histamine release. Such a response is immediate in nature and is likely to be severe.1(434) Such initiation of innate responses are driven by the presence of IgG or IgE antibodies; molecules produced by B lymphocytes (adaptive immunity) that bind to the surfaces of pathogens and is considered a type 1 allergic reaction.1(434) A food sensitivity is produced from an immune system-controlled response involving several immunoglobulin complexes, which also initiate a complement cascade (facilitates antibody and phagocytic cells) to clear pathogens.1(434) Such a process is slower that a type 1 allergic reaction and can take up to 7 days to complete.1(434). A food intolerance is the third type of adverse food reaction characterized by a non-immunological mechanism such as monosodium glutamate (MSG) or lactose intolerance.1(434)

In conclusion, the GIT a gateway facilitating immune function and entry of key macronutrients and micronutrients into the inner systems of the human body. As evidenced, dysregulation of such a system can become the progenitor of chronic inflammation, nutrient deficiencies, and other diseases such as gastroesophageal reflux, irritable bowel syndrome, Hashimoto’s thyroiditis, arthritis, and diabetes.1(416-417) As such, it is imperative to become aware of not only signs and symptoms of dysregulated GIT function, but tests and screens that can help monitor and track the presence of gut dysregulation.
References
1. Lord RS, Bralley JA. Laboratory Evaluations for Integrative and Functional Medicine.Duluth, GA: Genova Diagnostics; 2012.
2. Gropper SS, Smith, JL, Carr, TP. Advanced Nutrition and Human Metabolism (7thed.). Boston, MA: Cengage Learning; 2018.
-Michael McIsaac
