
Asthma is a product of a well-known overactive immune response that targets the lungs and effects an estimated 300 million individuals.1 Its symptoms include wheezing/shortness of breath/coughing and the understanding of its causes has grown to include genetic and other drivers.1(189) As research has mounted regarding the pathophysiology of asthma, more evidence has suggested that nutritional and environmental factors have been the cause of, and solution to, asthma. As such, the following will explore the same.

Interestingly, Kohlstadt1(189) presented an association with asthma and particular lifestyles; the highest concentrations of asthma tended to fall among groups that were leading Westernized lifestyles and eating habits. Common nutritional deficiencies included a lack of vitamin D (below 50-70 ng/ml), which could emanate from insufficient sun exposure and inadequate consumption of vitamin D-rich foods (i.e., salmon, sardines, shitake mushrooms).2,3 Common environmental factors related to asthma included poor air quality to include allergens such as mold, dust mites, cockroach antigens, and smoking. Furthermore, outside air affected by traffic and power generation are now also considered irritants, and causes of, asthma.1(189),4

In addition to nutritional deficiencies and air pollution, evidence has suggested that a lack of hydration (airway dehydration) has been associated with asthmatic episodes. Specifically, Maloney et al5 stated that exercise in virtually all patients with active asthma experienced bronchoconstriction when exercising. Furthermore, Cotter et al6 uncovered a relationship between exercise and hydration; the severity and duration of an asthmatic episode was directly related to the degree of dehydration an individual experienced. As such, dehydration, nutritional deficiencies, and environmental pollutants are all closely associated with restricted breathing. Having considered drivers behind asthma, the following will consider solutions for the same.

Kohlstadt1(191) suggested that increased fish consumption has been associated with a lowered risk of developing asthma. Such was explained by the anti-inflammatory properties of omega-3 fatty acids found in fish. Other interventions included a reduction of refined and processed foods; another characteristic of Westernized societies.1(189) Specifically said industrial foods are rich in pro-inflammatory omega-6 fatty acids, especially arachadonic acid; a fatty acid which particularly contributes to inflammatory cascades involved in many disease states.7
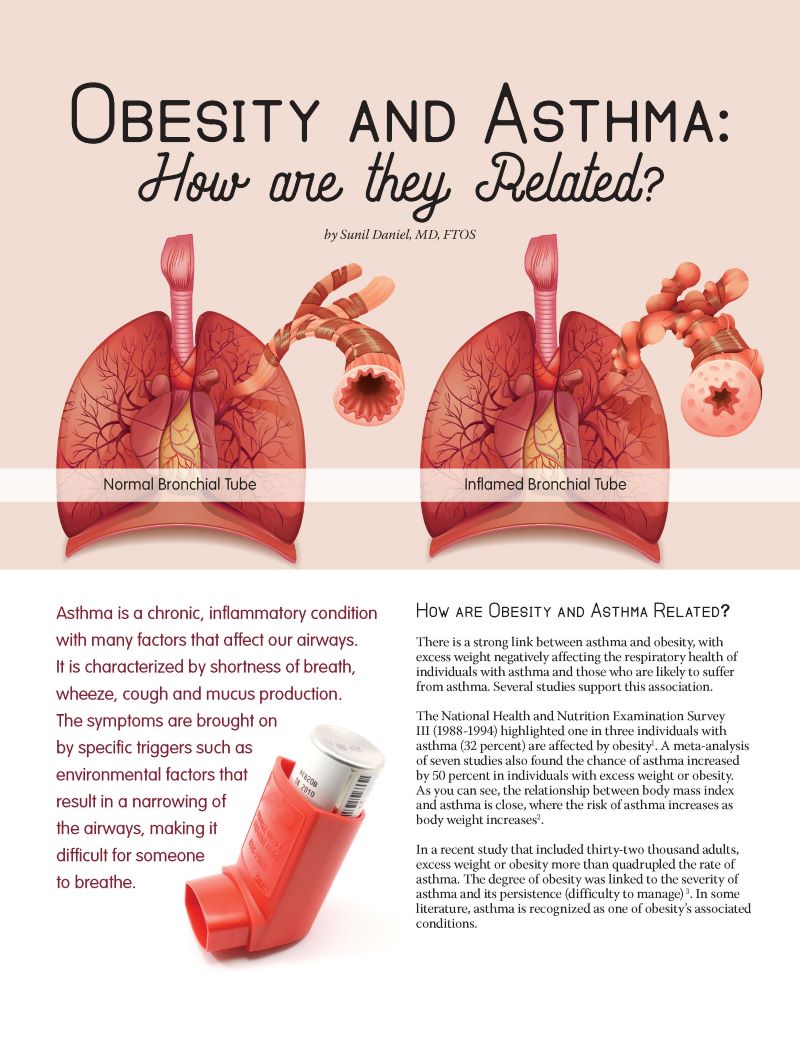
Obesity, a condition often caused by excessive consumption of carbohydrates/processed foods, is also associated with asthma.1(191),8 Obese individuals produce larger amounts of leptin and adipokines; substances which induces airway reactivity and contribute to inflammation, respectively.1(191) Thus, a reduction in processed food should help reduce arachadonic levels while simultaneously helping reduce body fat and associated leptin/adipokine production.
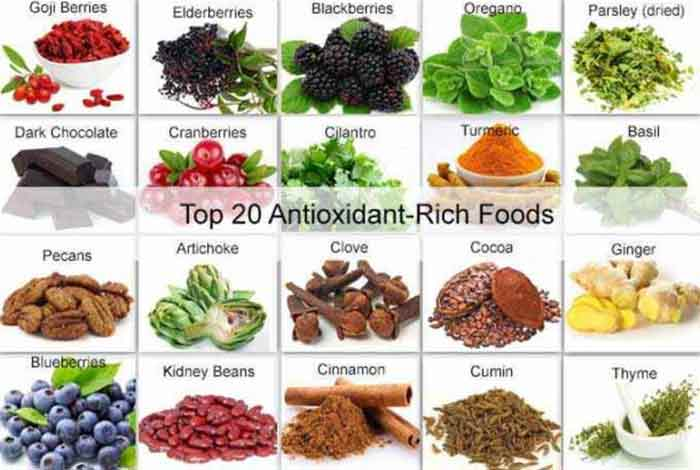
Improving antioxidant levels is another solution to decrease asthmatic episodes and severity of the same.1(191) Antioxidant-rich foods can be found from whole foods to include both fruit and vegetables, which contain vitamin E and vitamin C. Selenium and manganese have also been found to be deficient amongst asthmatics which might indicate replenishment of the same from food.1(191) Brazil nuts have an abundant level of selenium; two nuts a day is enough to satisfy daily requirements.9 Manganese can be found among many foods to include clams, oysters, mussels, nuts, legumes, leafy vegetables, tea, coffee, tea, and several spices, such as black pepper.10

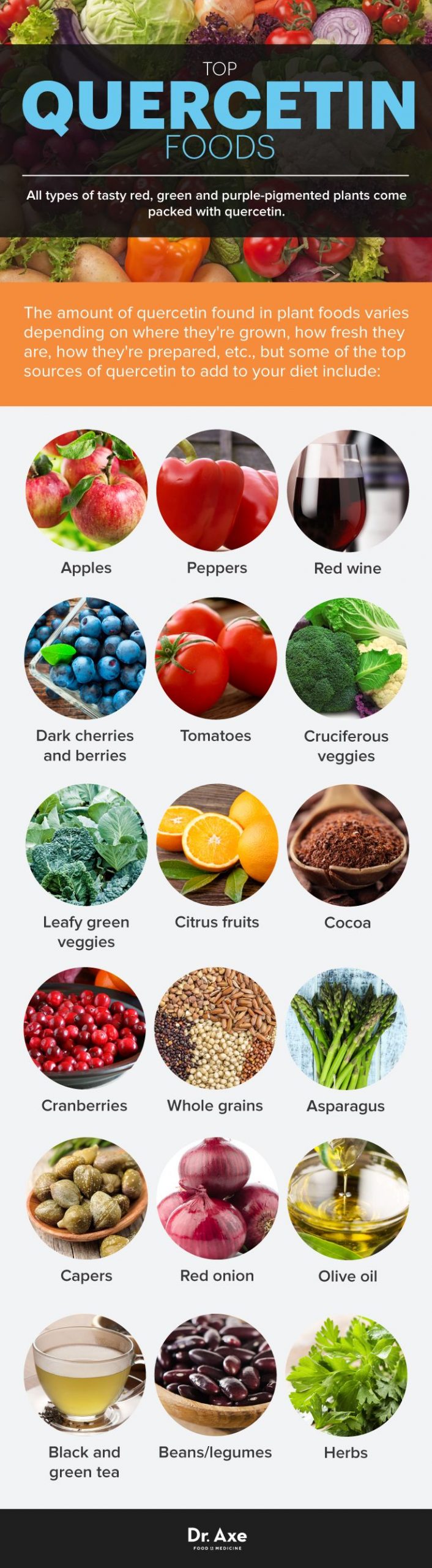
Zinc is another micronutrient found to be deficient amongst asthmatics, and inadequate levels has been associated with higher cytokine-rich (induces/regulates immune responses) environments and decreased metabolism of fatty acids.1(192) Optimal sources of zinc can be found in whole/unprocessed foods such as animal proteins (i.e., organ meats) and seafood (i.e., oysters).11 Quercetin is another nutrient that has been shown to help down-regulate the expression of cytokines, noted earlier, as well as the inflammatory contribution of mast cells; a component of the innate immune system.1(192) Quercetin can be found in abundance among both fruits and vegetables (i.e., nuts, seeds, tomatoes, leaves).12

Having considered nutritional influences upon asthma, as mentioned in the introduction, air quality is another relevant consideration. Research has suggested that individuals, especially young children, spend as much as 80% of their waking hours in homes.13 Although asthma-related airborne particles can be indigenous to a home, traffic pollution also constitutes a major portion of said particles found throughout a household as well.13(1) Research suggests that high- efficiency particulate air filtration (HEPA) systems significantly reduces the concentration of indoor particles.13(2)Furthermore, research by James et al13(2) indicated that HEPA systems were particularly effective in reducing asthmatic symptoms.13(2)
In conclusion, asthma is a and a well-known immune response that targets the lungs and effects an estimated 300 million individuals. Its symptoms include wheezing/shortness of breath/coughing and the understanding of its causes has grown to include nutritional and environmental drivers. As seen in the aforementioned sections, several micronutrients have been shown to support optimal lung function, in addition to maintaining optimal bodyweight and household air that has minimum particulate matter present. As an aggregate, such approaches should help support lung function and reduce asthmatic events.
References
1. Kohlstadt I. Advancing Medicine with Food and Nutrients. 2nd London, NY: CRC Press; 2012.
2. Rosen CJ. Vitamin D Insufficiency. N Engl J Med. 2011;364(3):248-254. doi: 10.1056/NEJMcp1009570.
3. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism. 7th ed. Boston, MA: Cengage Learning; 2018.
4. Guarnieri M, Balmes JR. Outdoor air pollution and asthma. Lancet. 2014; 383(9928):1581–1592. doi:10.1016/S0140-6736(14)60617-6.
5. Maloney E, O’Sulliven S, Hogan T. Airway dehydration: A therapeutic target of asthma? Clin Invest. 2002;121(6):1806-1811. doi:10.1378/chest.121.6.1806.
6. Cotter PC, Klein M, Weinberg EG. Hydration in severe acute asthma. J Allergy Clin Immunol. 2017;30(4):224-227. doi:10.1136/adc.66.2.216.
7. Nelson JR, Raskin S. The eicosapentaenoic acid: arachadonic acid ratio and its clinical utility in cardiovascular heart disease. Postgrad Med. 2019;131(4):268-277. doi: 10.1080/00325481.2019.1607414.
8. Ifland JR, Preuss HG, Marcus MT, et al. Refined food addiction: A classic substance use disorder. Med Hypotheses: 2009;72:518-526. doi:10.1016/j.mehy.2008.11.035.
9. Thomason CD, Chisholm A., McLachlan SK, et al. Brazil nuts: An effective way to improve selenium status.Am JClin Nutr. 2008;87(2):379-384. doi: 10.1093/ajcn/87.2.379.
10. Manganese. National Institutes of Health website. https://ods.od.nih.gov/factsheets/Manganese-HealthProfessional/. Accessed February 3, 2020.
11. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism. 7th ed. Boston, MA: Cengage Learning; 2018.
12. Li Y, Yao J, Han C, et al. Quercetin, inflammation and immunity. Nutrients. 2016;8(167):1-14. doi:10.3390/nu8030167.
13. James C, Bernstein DI, Cox J, et al. HEPA filtration improves asthma control in children exposed to traffic-related airborne particles. Indoor Air. 2019;1-9. doi:10.1111/ina.12625.
-Michael McIsaac
