Asthma is a condition induced by underlying inflammatory events, which affects as many as 300 million people causing as many as 300,000 deaths to date.1 Emerging evidence has suggested that nutrition, or lack thereof, has been implicated with asthma signs, symptoms, and underlying inflammation.1(1) One micronutrient, zinc (Zn), has been implicated/associated with inflammation and free radical generation and management; a potentially harmful process which, left unmanaged, can induce cellular and lung damage.2 As a means of appreciating the role of zinc in lung function, the following will consider the same in greater detail.

Zn, a micronutrient and essential metal/cofactor, is not exclusively involved in inflammation/free radical production; Zn can be found in many enzymes to include carbonic dehydratase, alkaline phosphatase, polymerases, and is also obligatory for cell division and DNA synthesis.2(2),3 As such, Zn has a widespread biochemical and physiological reach, similar to magnesium discussed in this author’s previous posts. The following will explore Zn, oxidative stress, and its relationship to asthma in greater detail.
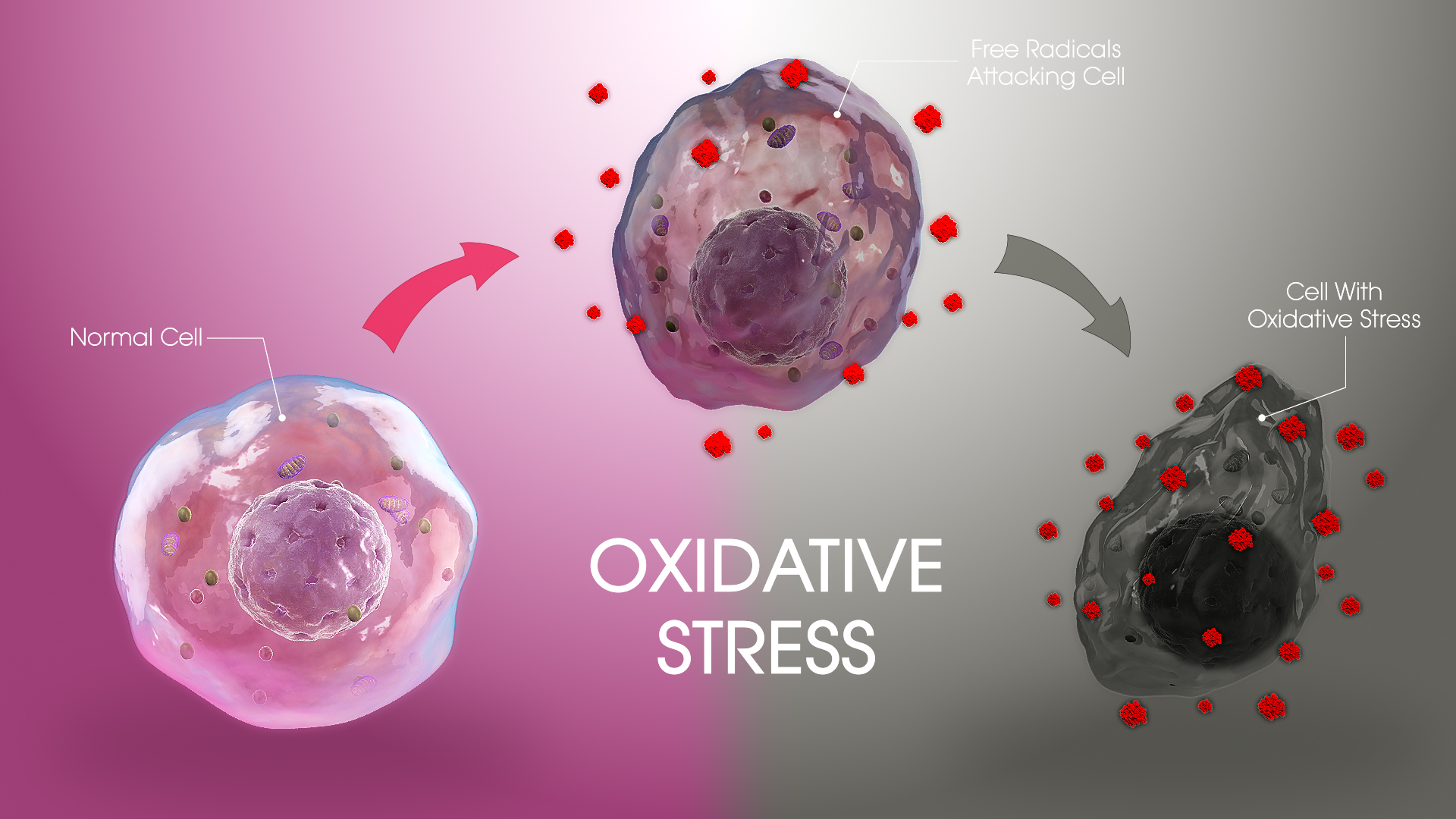
Oxidative stress is produced from free radicals (FRs) which are generated during normal metabolic processes as well as from exposure to pathophysiological states.4 Left unmanaged, FRs can cause damage (oxidative stress) to DNA, cells, and tissues.4(317) Furthermore, FRs have the capacity to breakdown lipid membranes, induce receptor malfunctions, and inactivate enzymes.5 Ultimately, since FRs have the ability to negatively affect an organism’s most basic functional unit (the cell), it has been suggested as a causative factor not only in inflammation but also in toxicity, neuronal injury, atherosclerosis, and Alzheimer’s disease.5(515)
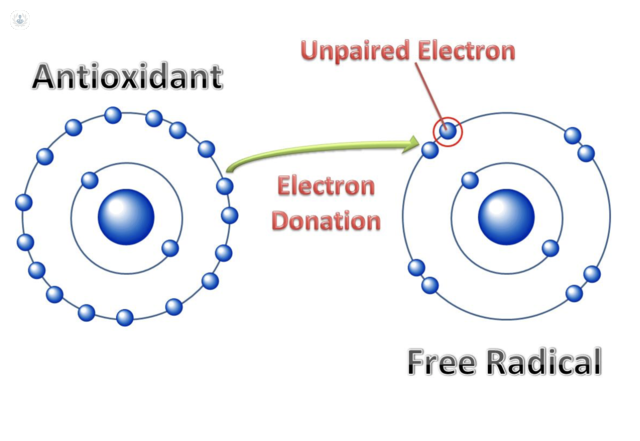
Oxidative stress, and the proliferation of FRs, is managed by antioxidants; substances which have the capability to reduce the damage induced by FRs.2(1) All FRs have unpaired electrons (the damaging trait), which seek electrons from nearby cells/DNA. Antioxidants can supply such electrons to FRs nullifying their oxidative effects upon other cells and tissues. 5(518) Zn, among its many functions, serves as an electron donor/antioxidant.2(1) Most interestingly, diets low in Zn (in addition to other antioxidants like selenium and vitamin C) has been associated with increased risk for asthma.2(1)
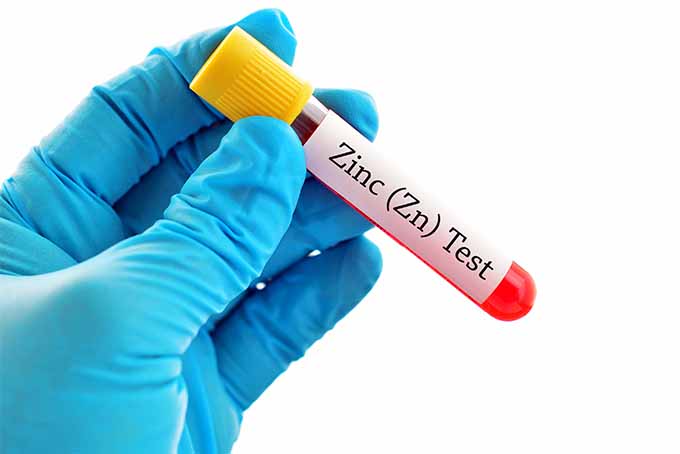
Yousef et al2(1-2) conducted a prospective case control study with 46 asthmatic patients (20 males, 26 females) and 30 healthy adults (12 males and 18 females). Blood samples were taken from three groups: group one included 26 patients presenting with acute asthma attacks, group two had 20 patients with asymptomatic bronchial asthma, and group three had 30 healthy individuals.2(2) Blood was collected and analyzed to measure serum zinc levels. Hypozincemia was defined as Zn concentrations below 60 mcg/dL. After analysis of Zn levels, Yousef et al2(2) determined that 44% of the participants in the study had hypozincemia, with the majority from group one and group two (asthmatic symptoms).2(2)
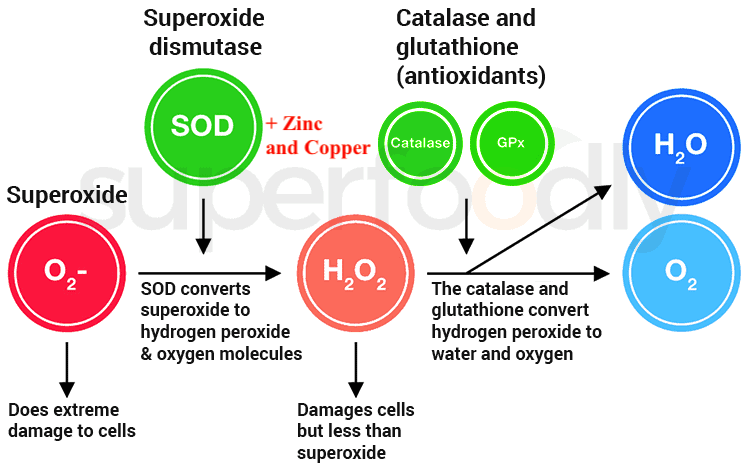
As mentioned previously, FRs can damage tissues and organs to include the lungs. Antioxidants such as glutathione peroxidase (GSH) and superoxide dismutases (SODs) helps control the cellular destruction from FRs.2(3) Most relevantly, Zn, in addition to copper, are required for the optimal function of SODs, while selenium is integral for GSH.2(3)Ultimately, if lung inflammation and oxidative stress are to be managed optimally, evidence suggests that optimal Zn levels can help manage the same.
In conclusion, Asthma is a condition induced by underlying inflammatory events, which affects as many as 300 million people causing as many as 300,000 deaths to date. Emerging evidence has suggested that nutrition, or lack thereof, has been implicated with asthma signs, symptoms, and underlying inflammation. Zn, a constituent of a larger set of antioxidants like SODs, has been shown to be higher in healthy individuals compared to those with asthma. As such, low Zn is a likely risk factor for asthma, and raising levels within normal ranges may help manage such a condition.
References
1. Abubat F, AlAwan A, Masuadi E, et al. The role of magnesium supplements for the management of stable bronchial asthma: A systematic review and meta-analysis. NPJ Prim Care Respir Med. 2019;29(1):1-8. doi:10.1038/s41533-019-0116-z.
2. Yousef AM, Elmorsy E. Serum zinc levels in bronchial asthma. EgyptJ Chest Dis Tuberc. 2017;66(1):1-4. doi:10.1016/j.ejcdt.2016.10.009.
3. Crook MA. Zinc deficiency. Nutrition. 2011;27(10):1085-1086. doi:10.1016/j.nut.2011.06.001.
4. Chen GL, Chen SG, Chen F, et al. Nutraceutical potential and antioxidant benefits of selected fruit seeds subjected to an in vitro digestion. J Funct Foods. doi:10.1016/j.jff.2015.11.003.
5. Lord RS, Bralley, JA. Laboratory Evaluations for Integrative and Functional Medicine 2nd ed. Duluth, GA: Genova Diagnostics; 2012; 20:317-331.
-Michael McIsaac
