
Bacterial vaginosis (BV) is a condition affecting approximately 21 million females between 14-44 years of age within the United States, with recurrence rates as high as 58%.1 The genesis of BV occurs from an imbalance of normal anaerobic lactobacillus populations relative to anaerobic bacteria in the vaginal fluid; a condition known as dysbiosis.2
Ultimately, if BV is left unmanaged, said condition can negatively affect an individual’s health and overall quality of life. As a means of appreciating BV, the following will consider the same in greater detail, in addition to exploring the efficacy of St. John’s wort as a pharmaceutical alternative in treating said condition.
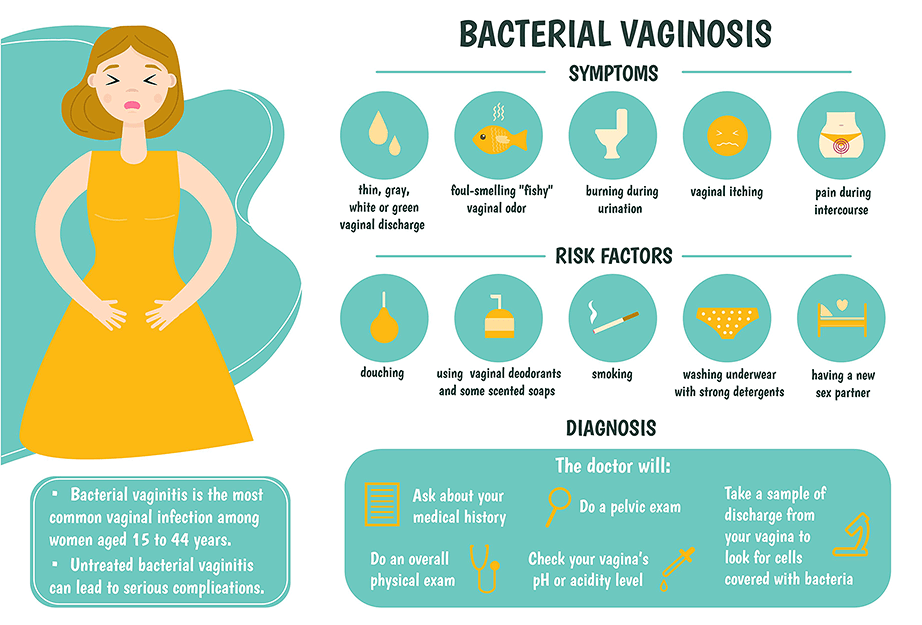
As mentioned in the introduction, BV is characterized by an overgrowth of anaerobic bacteria known as Gardnerella vaginalis as well as other microbes known as Prevotella bivia, Atopobium vaginae, and Peptostreptoccus.1(1) As overgrowth of anaerobic microbes continues, symptoms begin to present as a milky, white, malodorous discharge after sexual intercourse.1(1) BV becomes problematic since normal levels of lactobacillus is associated with a reduced risk of contracting sexually transmitted infections (STIs) such as herpes simplex virus (HSV), human papilloma virus (HPV), and human immunodeficiency virus (HIV).2(1481-1482)
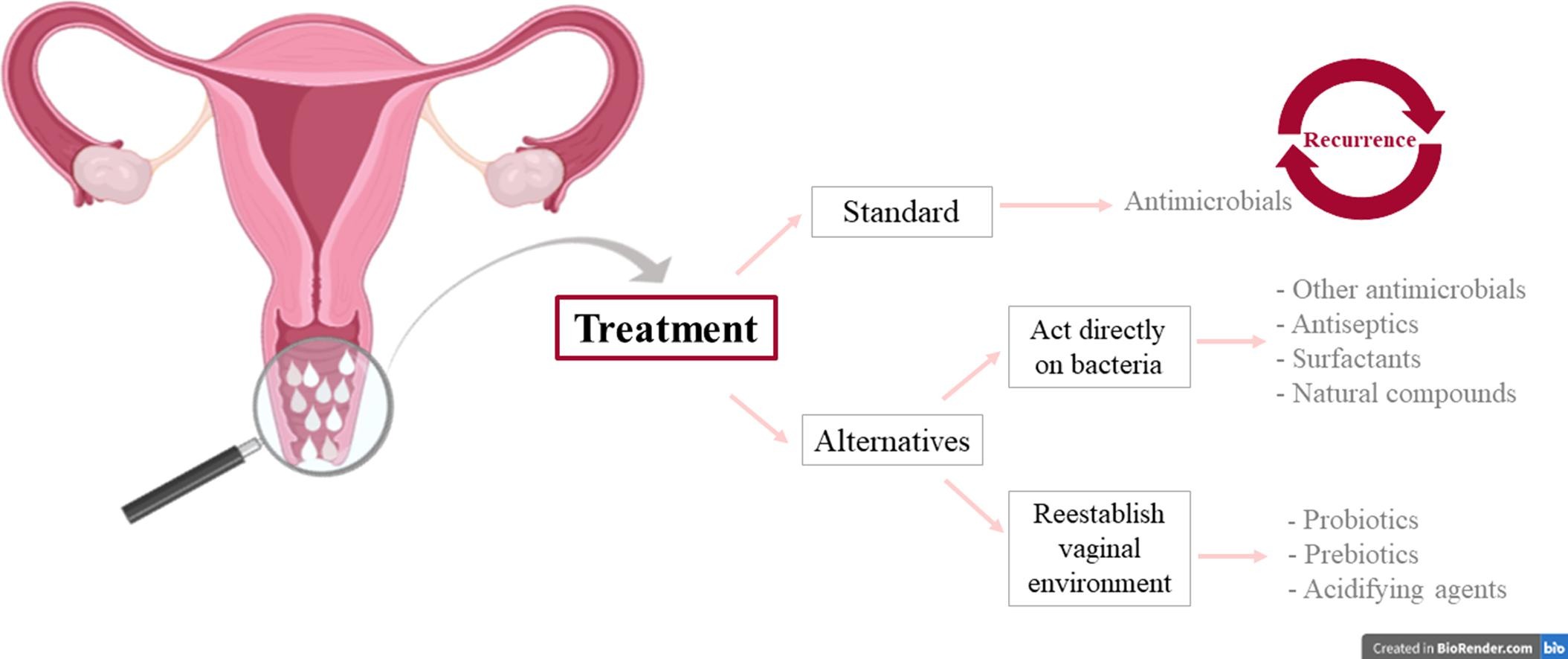
BV also exposes females to an increased risk of endometritis, preterm labor, and inflammatory disease.1(1)Typical treatment for BV usually includes metronidazole; an antibiotic which tends to have a 70-80% success rate.3 However, up to 30% of treated females tend to experience a recurrence of BV symptoms.3(897) Considering the downstream manifestations of vaginal dysbiosis, it is imperative to implement interventions which maximize favorable outcomes, while minimizing side effects.
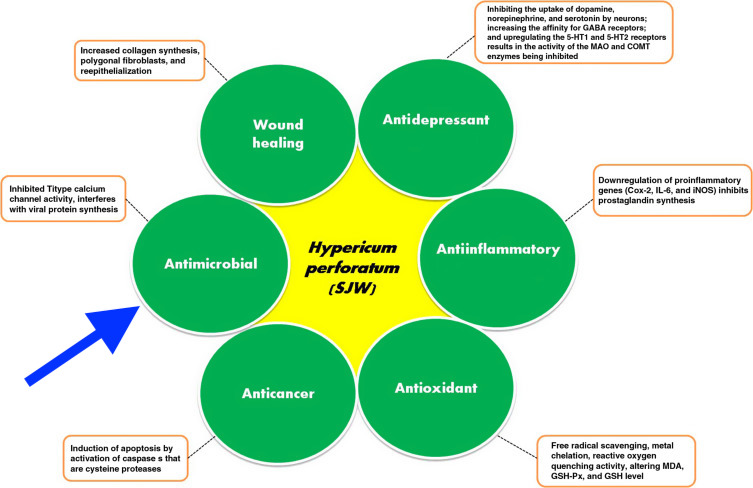
Metronidazole, though effective, does have unfavorable side effects to include vaginal candidiasis (fungal overgrowth), peripheral neuropathy, transient neutropenia (low white blood cell count), nausea, dizziness, and drowsiness.3(897)Furthermore, metronidazole can induce allergic reactions and drug resistance; outcomes, which can make said antibiotic an unappealing option.3(897) One particular alternative to antibiotic therapy can include St. John’s wort, also known as Hypericum perforatum L. (HPL); a botanical from the herbaceous and perennial plant that has been implemented for generations in traditional medicine for anxiety, sleep disorders, and depression.3(897)4
HPL has also been gaining attention as a means of managing menstrual disorders, bladder irritation, and as an analgesic (relieves pain).3(897) Furthermore, HPL has no known serious side effects in its medicinal use, making it an appealing candidate for individuals who require its benefits. Of particular relevance, and potential application to BV, is the antibacterial qualities of HPL found during in-vitro studies according to Charandabi et al3(897) The following sections will explore the same in greater detail.
As mentioned briefly in the aforementioned section, HPL exhibited potent antibacterial effects during in-vitro studies, though no in-vivo experiments were conducted. As such, Charandabi et al3(897) conducted an experiment whereby 162 women diagnosed with BV were randomly allocated into 2 groups using a permuted block method, with block sizes of 4 and 6 (allocation ratio of 1:1).3(898) All participants received two 40-gram tubes of vaginal gels to use over a 5-day period (twice a day); one tube of 3% H. perforatum as well as one tube of placebo of metronidazole.
The other combination included one tube of 0.75% metronidazole and one tube of placebo of H. perforatum.3(898) The researchers noted that placebos were used as it was not possible to make the two drugs identical in order to maintain blinding.3(898) 10 to 12 days after said treatments, participants were re-evaluated to determine efficacy of all interventions. The following sections will consider the outcomes in greater detail.

After the experiment was completed, the researchers indicated that 3% HPL for the prevention and treatment of BV was not only well tolerated; HPL was similar in its effect to 0.75% metronidazole gels with no serious side effects.3(900)Specifically, a positive response of 82% was found among the HPL group and while a positive response of 85% was found in the 0.75% metronidazole group.3(899) Furthermore, the frequency of homogenous discharge (a characteristic of BV) was significantly less when compared to the metronidazole group.3(899)
The presence of clue cells (a marker of bacterial vaginosis) and positive whiff test (i.e., a fish-like odour from the presence of putrescine/cadaverine/histamine/trimethylamine), were also significantly decreased in the both groups compared to the baseline measures, though no significant differences were recorded between HPL and metronidazole interventions.3(899)Such results suggest that HPL is comparable to metronidazole in its efficacy, while having significantly less side effects. HPL, therefore, could serve as a viable alternative to traditional pharmaceutical interventions, especially for individuals who have experienced drug resistance and who prefer herbal therapies.

In conclusion, BV is a condition affecting approximately 21 million females between 14-44 years of age within the United States, with recurrence rates as high as 58%. Considering that normal levels beneficial lactobacillus bacteria is associated with a reduced risk of contracting sexually transmitted infections and lowered risk of endometritis, preterm labor, and inflammatory disease, it is imperative that BV is treated in an expeditious fashion. Though traditional pharmaceutical therapies show a degree of promise, recurrence rates still occur as well as unfavorable side effects. However, the research of Charandabi et al3(901) has suggested that HPL could serve as a viable adjunct, or replacement, to metronidazole with little to no serious side effects.
References
1. Chavoustie SE, Maribona AS, Hanna M. Bacterial vaginosis and the risk for sexually transmitted infections. OB/GYN. 2020;65(4):1-6. http://eds.b.ebscohost.com/eds/pdfviewer/pdfviewer?vid=8&sid=5e356e79-cc8f-40af-8f4b-afc6950f4a55%40pdc-v-sessmgr04. Accessed July 14, 2020.
2. Singh R, Ramsuran V, Mitchev N, et al. Assessing a diagnosis tool for bacterial vaginosis. Eur J Clin Microbiol Infect Dis. 2020;39:1481-1485. doi: https://doi.org/10.1007/s10096-020-03862-3.
3. Charandabi SMA, Mohammadzadeh Z, Khalili AF, et al. Effect of Hypericum perforatum L compared to metronidazole in bacterial vaginosis: A double-blind randomized trial. Asian Pac J Trop Biomed. 2014;4(11):896-902. doi:10.12980/APJTB.4.201414B160.
4. Lakhan SE, Vieira KF. Nutritional and herbal supplements for anxiety and anxiety-related disorders: Systematic review. Nutr J. 2010;9(42):1-14. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2959081/. Accessed July 14, 2020.
-Michael McIsaac
