
Obesity is one of the most prevalent healthcare challenges, worldwide.1 Currently, Handzlik-Orlik et al1(383) stated that bariatric surgery (BS) is considered one of the most effective methods of achieving long-term weight loss, particularly when all other medical interventions have failed. However, BS is associated with complications to include micronutrient deficiencies.1(383) As such, it is essential to closely monitor signs, symptoms, and provide nutritional interventions where indicated to support recovery, weight loss, and overall health. As a means of appreciating BS, complications, and nutritional interventions, the following will explore the same in greater detail.
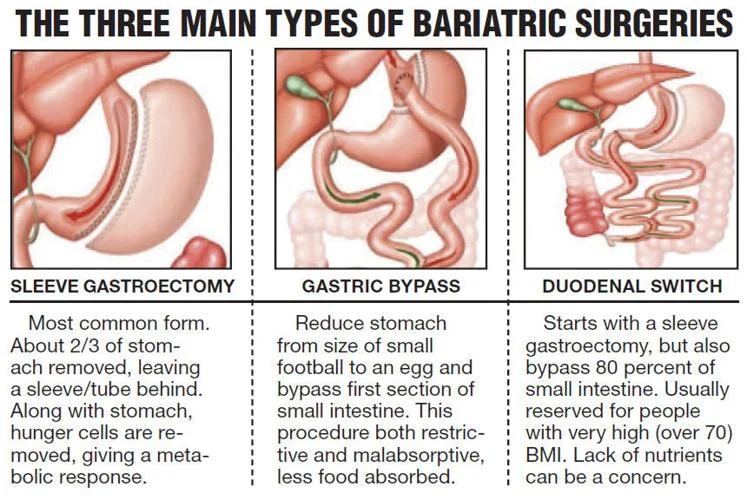
BS procedures can fall under 3 major categories: restrictive, malabsorptive, and mixed.1(383) Restrictive procedures include interventions such as adjustable gastric banding (AGB) and sleeve gastrectomy (SG); both serve as a means to reduce oral food intake by limiting gastric volume and inducing early satiety.1(383) Furthermore, said procedures leave the alimentary canal intact helping reduce rick of metabolic complications.1(383) Malabsorptive procedures include biliopancreatic diversion (BPD), which reduces stomach size and produces conditions for malabsorption.1(383) Mixed procedures such as gastric bypass or sleeve gastrectomy with a duodenal switch implement both techniques concurrently.1(383) Having briefly outlined various BS procedures, the following will consider nutrient deficiencies, biomarkers, and nutritional interventions for the same in greater detail.
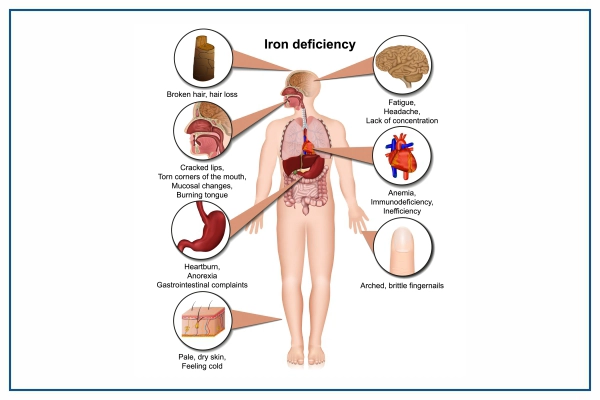
If an individual has gastric bypass surgery, such as the Roux-en-Y procedure (making a small pocket mimicking the stomach), several nutrient deficiencies have been associated with the same.2 For example, iron deficiency is common micronutrient deficiency in Roux-en-Y (RYGB) and is multifactorial in nature. Since iron is predominantly absorbed in the duodenum and proximal jejunum, RYGB bypasses said regions.2(724) Furthermore, iron-rich sources such as red meat tend to be poorly tolerated and is generally avoided during early stages of recovery.2(724) Iron absorption is also compromised because of a lack of hydrochloric acid (HCL); since the stomach is largely bypassed, less HCL is available to convert iron into the ferrous form (the type which is absorbed). Finally, if an individual is obese, hepcidin tends to be released in larger amounts inhibiting iron transport, despite successful absorption.2(724) Tests should be taken 6 months after surgery, and if total iron is below 38.5 ng/ml (for a female), and transferrin saturation is below 10%, 45-65 mg/day of elemental iron is recommended. 2(725),3,4 Finally, tests should be repeated annually.2(725)
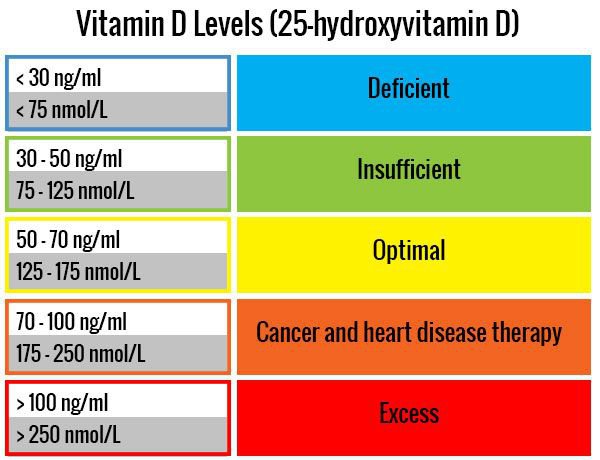
Vitamin D (measured as 25-hydroxyvitamin D, or 25OHD, in the blood) also tends to be deficient amongst patients undergoing BS.1(384) Furthermore, said nutrient tends to be low before surgery likely due to suboptimal sun exposure and/or inadequate consumption of foods rich in vitamin D.1(384) Finally, the presence of excessive adipose tissue among obese individuals tends to absorb 25OHD and limit its availability in the blood for cellular use.1(384) This author would suggest immediate analysis of 25OHD levels; if serum 25OHD is less than 30 ng/ml, deficiency is present.4(44) Cannell et al5 suggested 1000 IU of vitamin D3 for every 15 kg bodyweight as a starting point; follow-up serum 25OHD testing should occur at least every 6 months thereafter to monitor said nutrient concentration.6 Lord et al4(43) indicated that individuals routinely exposed to sunlight (i.e., near the equator) had 25OHD levels between 54 to 90 ng/ml. As such, if the body is willing to produce and maintain said 25OHD concentrations, it would seem logical to replicate such levels in the absence of sunlight.
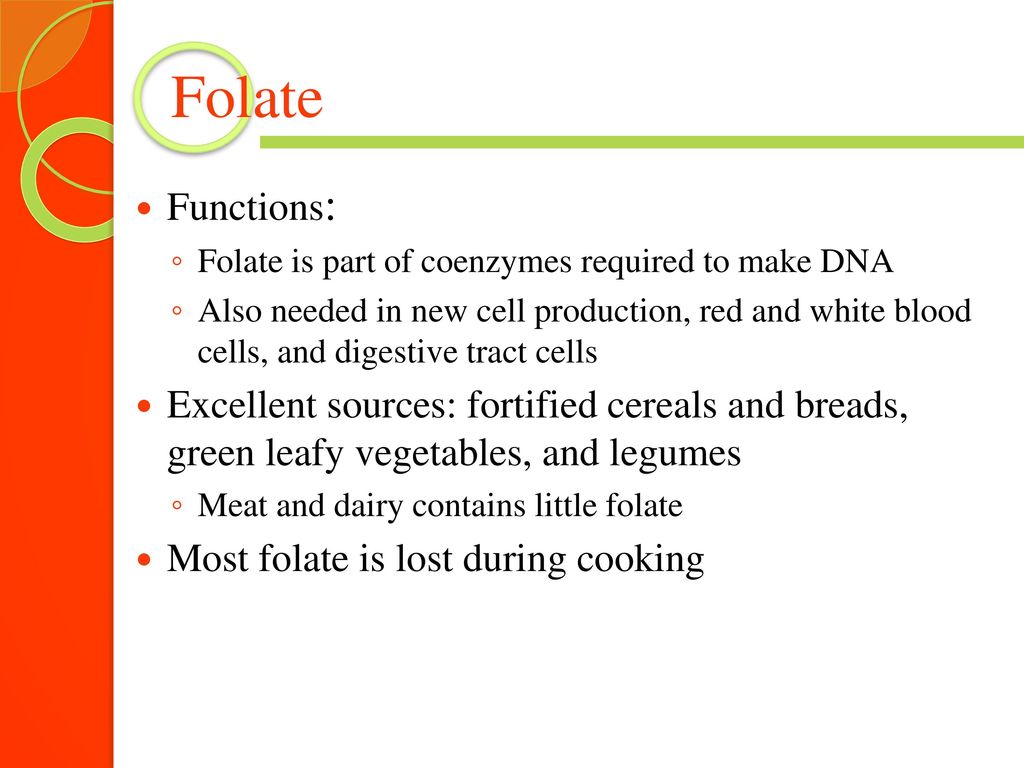
Folate (B9) is another micronutrient that tends to be deficient among individuals who undergo BS. Since the stomach/duodenum/jejunum is bypassed in the case of RYGB, such surgery is likely to account for a portion of B9 deficiency.7 The other, and perhaps more relevant, cause of B9 deficiency is a general lack of consumption of folate-rich foods (i.e., leafy vegetables, meat, poultry).1(386) Specifically, 25% of obese patients undergoing BS has B9 deficiency beforehand. Since B9 plays many roles to include metabolism of nutrients such as choline, amino acids, pyrimidines, purines, DNA synthesis/repair, and cell division, it is imperative that optimal levels are maintained so as to avoid conditions/diseases associated with the same.8,9 Since B9 is generally a cause of under-consumption folate-rich foods, increasing the same would be a logical first step. If there is difficulty consuming adequate amounts of B9, supplementation of 400 mcg/day is advised.1(386) Finally, B9 can be evaluated by serum B9 (<3 ng/ml is deficient) or through formiminoglutamate (>50 mg is deficient).4(38)
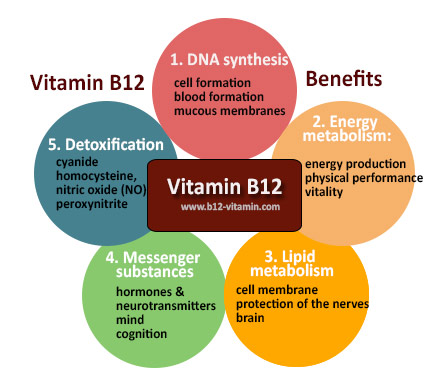
Vitamin B12 is highly prevalent deficiency following BS, and is widely caused by a lack of intrinsic factor (IF) production.1(385) IF is a glycoprotein synthesized and secreted by gastric parietal cells (located in the stomach).10 IF has a high affinity for the binding and transport of B12; once IF/B12 reaches terminal ileum, it is absorbed after contacting specific receptors in the membranes of cells of ileal lumen.10(3) However, such processes are inhibited in BS patients since the stomach is largely circumvented in said surgeries. B12 can be assessed via serum (<150 pg/ml equals deficiency) levels to indicate availability as well through methylmalonic acid (MMA) (>3 ug/mg suggests deficiency); an organic acid, which helps determine the degree of B12 use, or lack thereof.4(32) If B12 is determined to be deficient, consumption of animal proteins is suggested.8(352) If difficulty is experienced consuming adequate levels of animal protein, supplementation of high dose B12 therapy might be indicated using 1000 mcg/day, with levels should be re-assessed every 6 months.1(386)
In conclusion, obesity is one of the most prevalent healthcare challenges, worldwide. Currently, BS is considered one of the most effective methods of achieving long-term weight loss, particularly when all other medical interventions have failed. However, BS is associated with complications and micronutrient deficiencies, demanding surveillance of the same. If micronutrient deficiencies are elucidated, introduction of foods rich in the same and/or supplementation with said micronutrients is indicated. Ultimately, such vigilance should help support recovery, weight loss, and overall quality of life.
References
1. Handzlik-Orlik G, Holecki M, Orlik B, et al. Nutrition management of the post-bariatric surgery patient. Nutr Clin Pract. 2015;30(3):383-392. doi:10.1177/0884533614564995.
2. Isom KA, Andromalos L, Ariagno M, et al. Nutrition and metabolic support recommendations for the bariatric patient. Nutr Clin Pract. 2014;29(6):718-739. doi:10.1177/0884533614552850.
3. Iron Deficiency Anemia: Diagnosis. Mayo Clinic Website. https://www.mayoclinic.org/diseases-conditions/iron-deficiency-anemia/diagnosis-treatment/drc-20355040. Accessed March 23, 2020.
4. Lord RS, Bralley, JA. Laboratory Evaluations for Integrative and Functional Medicine. 2nd ed. Duluth, GA: Genova Diagnostics; 2012.
5. Cannell JJ, Hollis BW. Use of vitamin D in clinical practice. Altern Med Rev. 2008;13(1):6-20. http://archive.foundationalmedicinereview.com/publications/13/1/6.pdf. Accessed March 23, 2020.
6. Kohlstadt I. Advancing Medicine with Food and Nutrients. 2nd ed. London, NY: CRC Press; 2012.
7. Visentin M, Diop-Bove N, Zhao R, et al. The intestinal absorption of folates. Annu Rev Physiol. 2014;76:251-274. doi:10.1146/annurev-physiol-020911-153251.
8. Gropper SS, Smith JL, Carr TP. Advanced Nutrition and Human Metabolism. 7th ed. Boston, MA: Cengage Learning; 2018.
9. Sanvisens A, Zuluaga P, Pineda M, et al. Folate deficiency in patients seeking treatment of alcohol use disorder. DrugAlcohol Depend. 2017;180:417-422. doi: 10.1016/j.drugalcdep.2017.08.039.
10. Bizzaro N, Antico A, Villalta D. Autoimmunity and gastric cancer. Int J Mol Sci. 2018;19(2):1-14. doi:10.3390/ijms19020377.
-Michael McIsaac
