Low high-density lipoprotein cholesterol (HDL-C), high low-density lipoprotein cholesterol (LDL-C), a high ratio of total cholesterol/HDL, high alanine aminotransferase (ALT), and a high hemoglobin A1C are common markers on blood chemistry panels. However, left unmanaged, such markers can manifest into conditions unfavorable to health such as cardiovascular heart disease. As a means of appreciating blood chemistry panels, the following will consider biomarkers and the potential physiological consequences of each, as well as nutritional interventions to support a return of said markers to optimal ranges.
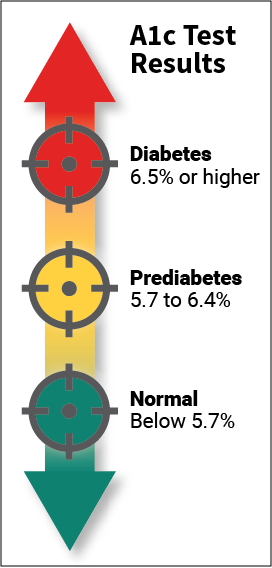
Hemoglobin A1C (HGA1C) is a marker of historical average levels of plasma glucose over the life of a red blood cell (~3 months).1 Normal ranges are generally below 5.7% while ranges between 5.7%-6.4% indicate pre-diabetic conditions, and percentages above 6.5% represent diabetes.1(592) A HGA1C of 5.7% indicating pre-diabetes. Maintaining optimal levels of blood glucose concentrations is essential to avoid hyperglycemia (too much blood glucose); a condition which causes excessive losses of fluids through the kidneys as a means to remove glucose.1(592) Such a process causes dehydration, electrolyte loss, and amino acid loss.2(592) Left un-managed, severe hyperglycemia can induce ketoacidosis; a condition that can induce cerebral edema, hypokalemia, hypoglycemia, acute renal failure, and shock.2
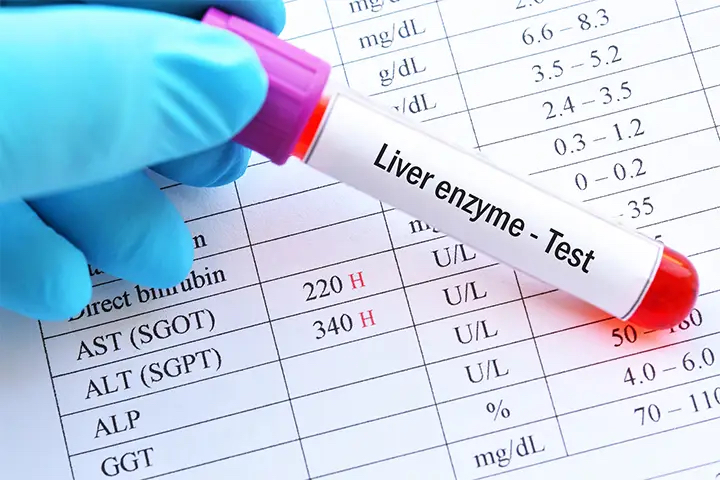
Alanine aminotransferase (ALT) is an enzyme found abundantly within the liver; a protein which facilitates energy metabolism by converting alanine (an amino acid) into pyruvate (a substance used to produce cellular energy).3 Generally, ALT remains within the confines of the liver. However, if the liver becomes compromised, ALT is summarily released into the bloodstream; a potential indicator of liver damage/disease.3(235) Furthermore, elevated ALT blood measures have also associated with Alanine transaminase (ALT) is associated with cardiovascular disease (CVD), obesity, and CVD-related mortality. Finally, clinical and population studies have related ALT with metabolic syndrome, insulin resistance, and type 2 diabetes.4
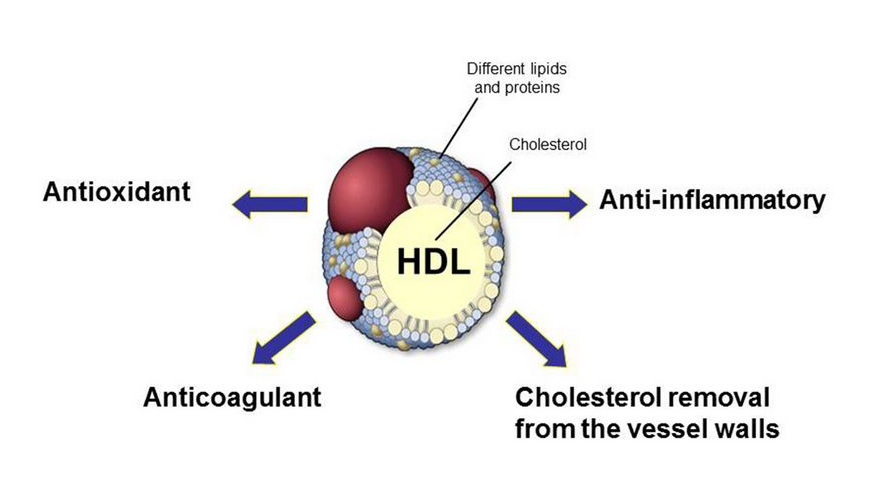
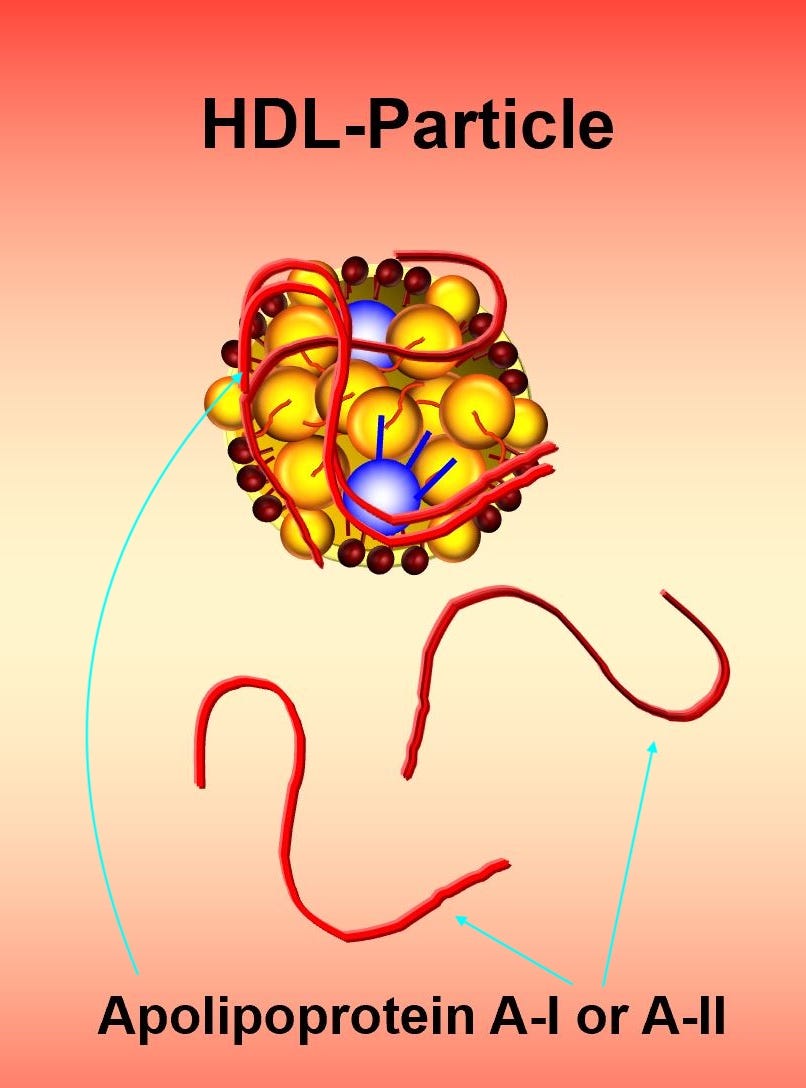
As discussed in this author’s previous posts, HDLs carry excess cholesterol (and to a lesser extent triglycerides, phospholipids, and protein) from the peripheral tissues back to the liver; a process known as reverse cholesterol transport.5 LDLs are particles which transport and deposit cholesterol (as well as triglycerides, phospholipids, and protein) along peripheral tissues, and have been associated with increased risk of CVD, especially small/dense subclasses.6 Optimal concentrations of said cholesterol transporters are relevant to reduce risk of CVD. However, the ratio of total cholesterol to HDL cholesterol (HDL-C) is another meaningful marker, of which an outcome of less than or equal to 5 is optimal.7 In addition to optimal HDL-C (characterized by a Apolipoprotein A protein within HDL) concentrations, research also indicates that large HDL particles (HDL2) are associated with reduced risk of CVD, while smaller HDL particles were associated with increased risk.7(114)
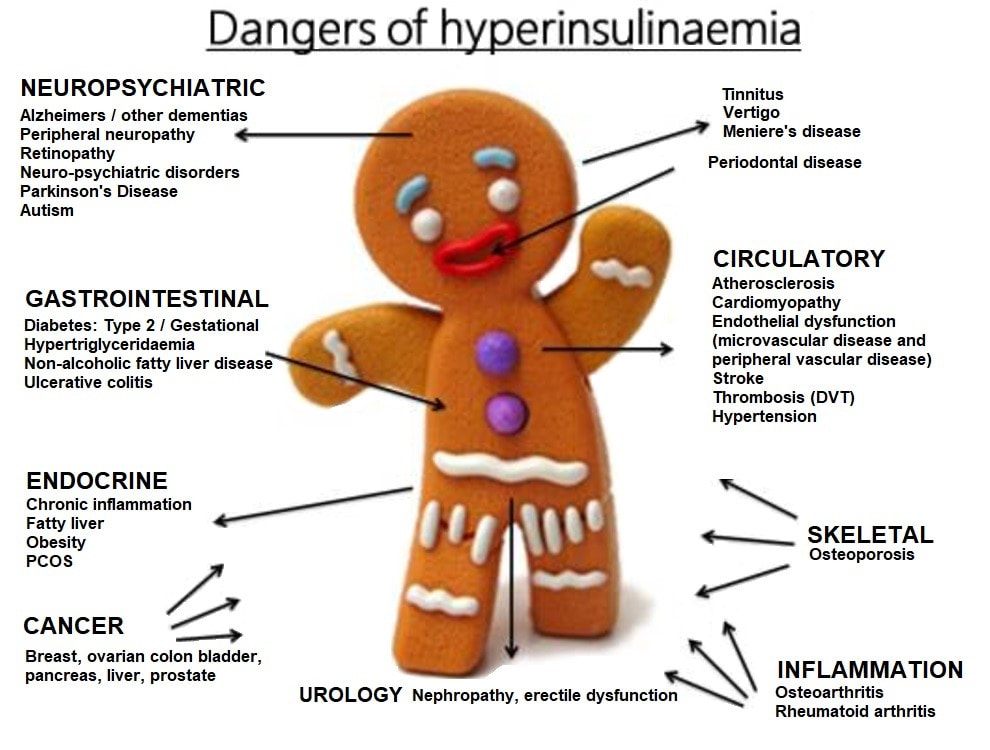
Having briefly considered the physiological consequences of aberrant biomarkers, it is essential to develop strategies which return such markers back to optimal ranges. One additional test this author would request would be fasting insulin, as a means of elucidating the nature of elevated HGA1C. Often, elevated glucose levels occur from a condition known as insulin resistance; a process characterized by higher than normal levels of insulin required to store excess glucose away.3(556) Initially, higher levels of insulin maintain blood glucose levels. However, progressively larger concentrations of insulin begin to fail at maintaining glucose levels; a condition known as hyperinsulinemia. Such a condition is problematic as it increases triglycerides, LDLs, risk of CVD, elevated ALT, and non-alcoholic fatty liver disease (NAFLD); markers which are already elevated in the above blood chemistry panel7(556)

Since HGA1C is associated with chronic hyperinsulinemia, high LDLs, and NAFLD, this author would implement strategies that reduced hyperinsulinemia/elevated blood glucose. One such strategy would be to reduce high glycemic foods (processed carbohydrates) with lower glycemic options (i.e., leafy green vegetables).7(556) This author would also recommend choosing foods rich in chromium and magnesium; micronutrients found to improve insulin sensitivity. In conjunction to reduced glycemic index foods, this author would also recommend foods rich in omega-3 fatty acids (O3FAs) which may also help improve insulin sensitivity while concomitantly facilitating the increase of HDLs and improving the total cholesterol/HDL ratios.7(556),9
In conclusion, elevated HGA1C/ALT/LDLs and low HDLs can increase the risk of CVD as well as other conditions. Although the above recommendations are not a complete solution to managing such markers, it does demonstrate value in finding a common thread between such conditions (when possible) like hyperinsulinemia/elevated HGA1C. Such an approach can allow for the possibility of managing multiple biomarkers in a near simultaneous fashion. Ultimately, said method can help move the individual towards improved health in a more effective and meaningful manner.
References
1. Reisner EG, Reisner HM. An Introduction to Human Disease: Pathology and Pathophysiology Correlations. 10th ed. Burlington, MA: Jones & Bartlett Learning; 2017.
2. Westerberg DY. Diabetic ketoacidosis: Evaluation and treatment. Am Fam Physician. 2013;87(5):337-346. https://www.aafp.org/afp/2013/0301/p337.html. Accessed Jan 20, 2020.
3. Lord RS, Bralley, JA. Laboratory Evaluations for Integrative and Functional Medicine. 2nded. Duluth, GA: Genova Diagnostics; 2012.
4. Bekkelund SI, Jorde R. Alanine aminotransferase and body composition in obese men and women. Dis Markers. 2019;2019:1-11. doi:10.1155/2019/1695874 (Links to an external site.).
5. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism.7thed. Boston, MA: Cengage Learning; 2018.
6. Pizzorno J, Katzinger, J. Clinical pathophysiology: A functional perspective. Coquitlam, BC: Mind Publishing Inc; 2012.
7. Hwang YC, Fujimoto WY, Kahn SE, et al. Higher high density lipoprotein 2 (HDL2) to total HDL cholesterol ratio is associated with a lower risk for incident hypertension. Diabetes Metab J. 2019;43(1):114-122. doi:10.4093/dmj.2018.0053.
8. Lin J, Ridker PM, Pradhan A, et al. hemoglobin A1c concentrations and risk of colorectal cancer in women. Cancer Epidemiol Biomarkers Prev. 2005;14(12):2010-3012. doi: 10.1158/1055-9965.EPI-05-0533.
9. Simopoulos AP. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med. 2008;233(6):674-688. doi:10.3181/0711-MR-311.
-Michael McIsaac
