The following will consider blood panels with high total cholesterol, high LDL cholesterol (LDL-C), high lipoprotein (a), high free androgen index, high gamma tocopherol, low zinc, low beta-carotene, and high trans fatty acids. As a means of appreciating said markers, associated cardiovascular health consequences, and solutions to optimize said markers, the following will explore the same.
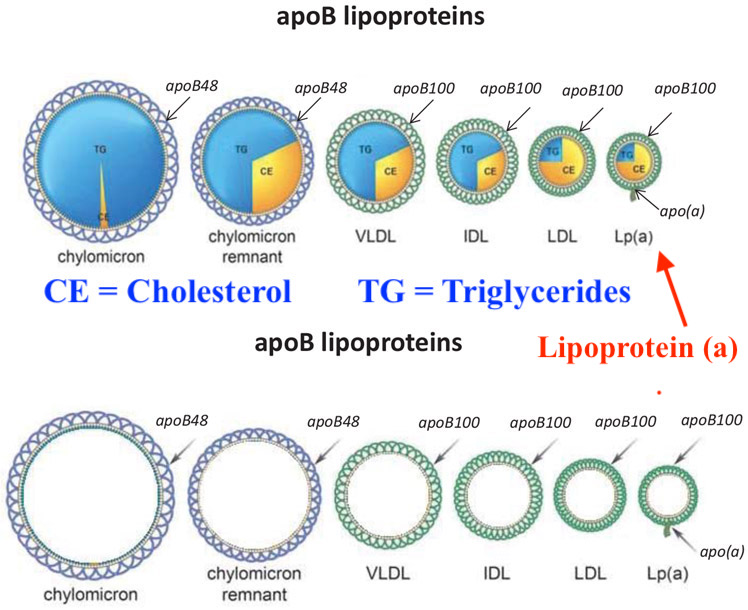
This author has covered the physiological aberrations that occur from high total cholesterol and high LDL-C in previous posts. Thus, focus will be placed on other markers found from the above section such as high lipoprotein (a), or LP(a). LP(a) is a genetically inherited (from the APOA gene) and expressed form of LDL with a glycoprotein known as apolipoprotein (a) on its surface; one which is particularly associated with cardiovascular disease (CVD).1 However, research has indicated that pharmacological interventions to reduce concentrations of LP(a) have provided no clinically meaningful outcomes except for a novel treatment using lipoprotein apheresis (LA).1(895) However, Moriarty et al1(899) indicated using said intervention is suggested in until future treatments become available; LA therapy should be considered for patients with elevated LP(a) and progressive CVD, on maximum lipid-modifying pharmacotherapy, irrespective of their LDL-C levels.
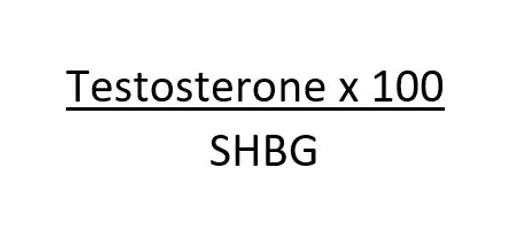
Free androgen index (FAI) is the ratio between total testosterone and sex hormone binding globulin (SHBG).2 According to Nadir et al,2(128) FAI is thought to be the most sensitive measurement for the evaluation of hyperandrogenaemia (high levels of androgens in females) found in polycystic ovary syndrome (PCOS) and is thus the most preferred test for the same. PCOS is generally associated with overweight, though obesity does not constitute the only cause of metabolic abnormalities.2(128) Insulin resistance (IR) is also associated with PCOS, but may also occur amongst lean females with PCOS.2(128) Dyslipidemia represents another common metabolic abnormality in PCOS, with decreased levels of HDLs and elevated triglycerides (TG).2(128) Furthermore, Nadir et al2(131) indicated that elevated LDL-C levels, and small/dense LDL particles, were also present in women with PCOS.
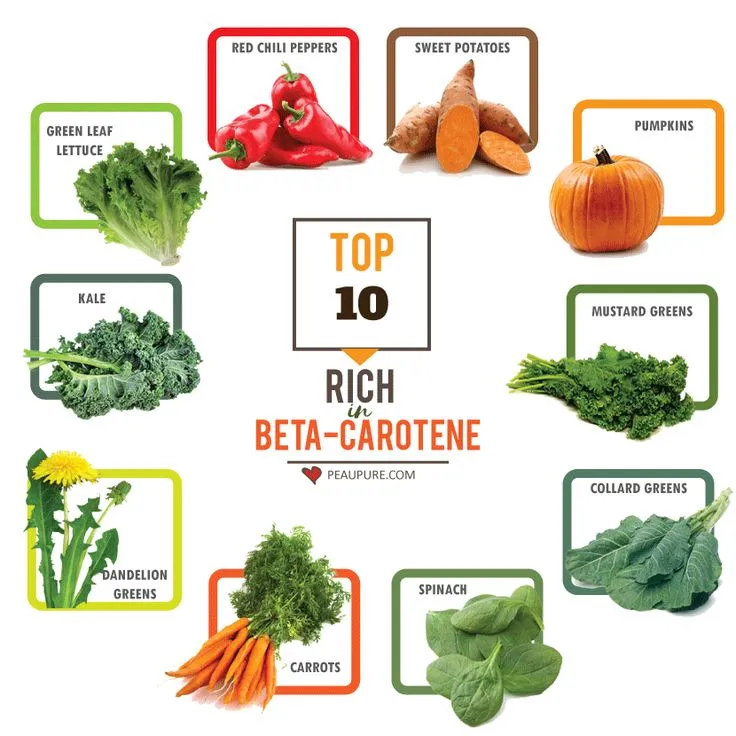
Low beta-carotene (precursors to vitamin A) levels can become problematic as said micronutrient is responsible for growth, reproduction, bone development, proper immune system function, and antioxidant protection.3,4 Thus, sub-optimal levels can contribute to aberrations in said functions. Furthermore, zinc deficiencies (as indicated in the introduction) have also been correlated to compromised vitamin A metabolism and transport, especially amongst individuals with compromised liver function.5

Zinc is essential as it is an essential cofactor/metal in many enzymes to include alkaline phosphatase, carbonic dehydratase, and polymerases and is obligatory for cell division and DNA synthesis.6 Deficiencies in Zn can induce several maladies such as increased risk of infections, impaired brain development, dermatitis, alopecia, low testosterone, impaired smell/taste, and infertility.6(1085),7
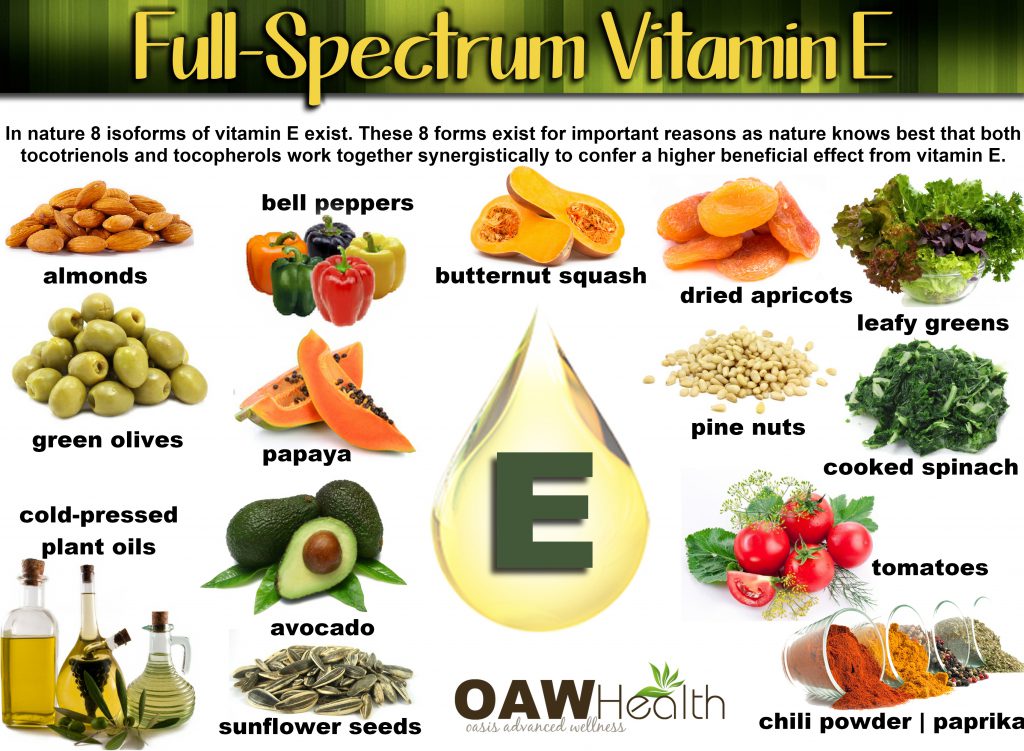
Gamma-tocopherol, a form of vitamin E, is a fat-soluble compound most widely recognized by its anti-oxidant capabilities and capacity to maintain/protect cell membranes and lipoproteins.3(403) Although Gropper et al3(407) stated that vitamin E tends to be one of the least toxic fat-soluble vitamins, higher levels can potentially lower other key micronutrients to include selenium. Furthermore, high levels of vitamin E can also reduce blood levels of beta-carotene; a biomarker stated as low in the previous section and likely due to high gamma tocopherol levels.3(406) In addition to high levels of gamma tocopherol levels, high levels of trans fatty acids can also induce unfavorable physiological changes within the body. As such, the following will consider the same.

Trans fatty acids (TFAs) are a form of unsaturated fatty acids that can occur naturally in dairy and meat or can be, and generally is, industrially produced to enhance the shelf-life and texture of food products.8 Even though unsaturated fatty acids are beneficial to human health, TFAs pose significant health risks with particular likelihood of inducing coronary heart disease.8(1) Furthermore, the main source of industrially produced TFAs is partially hydrogenated oils; substances often found in baked products and fried snacks. Thus, removal of TFAs from the food supply has been considered the most logical and straightforward public health interventions for rapid improvements in health; an approach considered paramount in mitigating diet-related noncommunicable diseases.8(1-2)

One intervention to help improve said biomarkers is the removal of trans fats via reductions in processed food consumption. Considering the evidence supporting widespread deleterious effects of TFAs, such an approach is likely to confer health benefits beyond attenuation of CVD. Another nutritional protocol to help improve cardiovascular health is a reduction in vitamin E consumption. As such, this author would gather a 3-day dietary record to further elucidate the source of excessive vitamin E consumption. If successful reduction of gamma tocopherol were ascertained, it is likely beta carotene levels would return to normal levels. This author would also increase zinc levels via food sources to include seafood and beef sources.3(500) Such an approach would likely support immune function and hundreds of biochemical reactions.3(504)

This author would also recommend foods rich in CoQ10 as said micronutrient helps in oxidative phosphorylation/energy production within the mitochondria of the cell. Furthermore, evidence suggests CoQ10 helps reduce hypertension, and can be found in red meat, heart, and liver.8 Although said micronutrient is not out of normal range, it still remains near the low range. This author would also increase omega-3 fatty acids via fish consumption as a means of improving HDL-C concentrations. Although EPA and DHA are within range, additional omega-3 fatty acids should help improve the total cholesterol/HDL ratio and support decreases in LDL-cholesterol.9
References
1. Moriarty PM, Gray JV, Gorby LK. Lipoproetin apheresis for lipoprotein(a) and cardiovascular disease. J Clin Lipidol. 2019;13(6):894-400. doi:10.1016/j.jacl.2019.09.010.
2. Nadir A, Temizkan S, Ozderya A, et al. Dehydroepiandrosterone sulfate/free androgen index ratio predicts a favorable metabolic profile in patients with polycystic ovary syndrome. Gynecol Endocrinol. 2019;35(2):128-132. doi:https://doi.org/10.1080/09513590.2018.1505843.
3. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism.7thed. Boston, MA: Cengage Learning; 2018.
4. Grune T, Lietz G, Palou A, et al. Beta carotene is an important vitamin A source for humans. J Nutr. 2010;140(12):2268S–2285S. doi:10.3945/jn.109.119024.
5. Christian P, West, KP. Interactions between zinc and vitamin A: An update.Am JClin Nutr. 1998;68(2),435S-441S.doi:10.1093/ajcn/68.2.435S.
6. Crook MA. Zinc deficiency.Nutr. 2011;27(10), 1085-1086. doi:10.1016/j.nut.2011.06.001.7. 7.
7. Liu YL, Zhang MN, Tong GY, et al. The effectiveness of zinc supplementation in men with isolated hypogonadotropic hypogonadism.Asian J Androl. 2017;19(3):280-285. doi:10.4103/1008-682X.189621.
8. Downs S, Bloem MZ, Zheng M. The impact of policies to reduce trans fat consumption: A systematic review of the evidence. Curr Dev Nutr. 2017;1(12):1-10. doi:10.3945/cdn.117.000778.
9. Kohlstadt I. Advancing Medicine with Food and Nutrients. 2nd London, NY: CRC Press; 2012.
10. Blom WAM, Koppenol W, Hiemstra H, et al. A low-fat spread with added plant sterols and fish omega-3 fatty acids lowers serum triglyceride and LDL-cholesterol concentrations in individuals with modest hypercholesterolaemia and hypertriglyceridemia. Eur J Nutr. (2019) 58:1615–1624. doi:https://doi.org/10.1007/s00394-018-1706-1.
-Michael McIsaac
