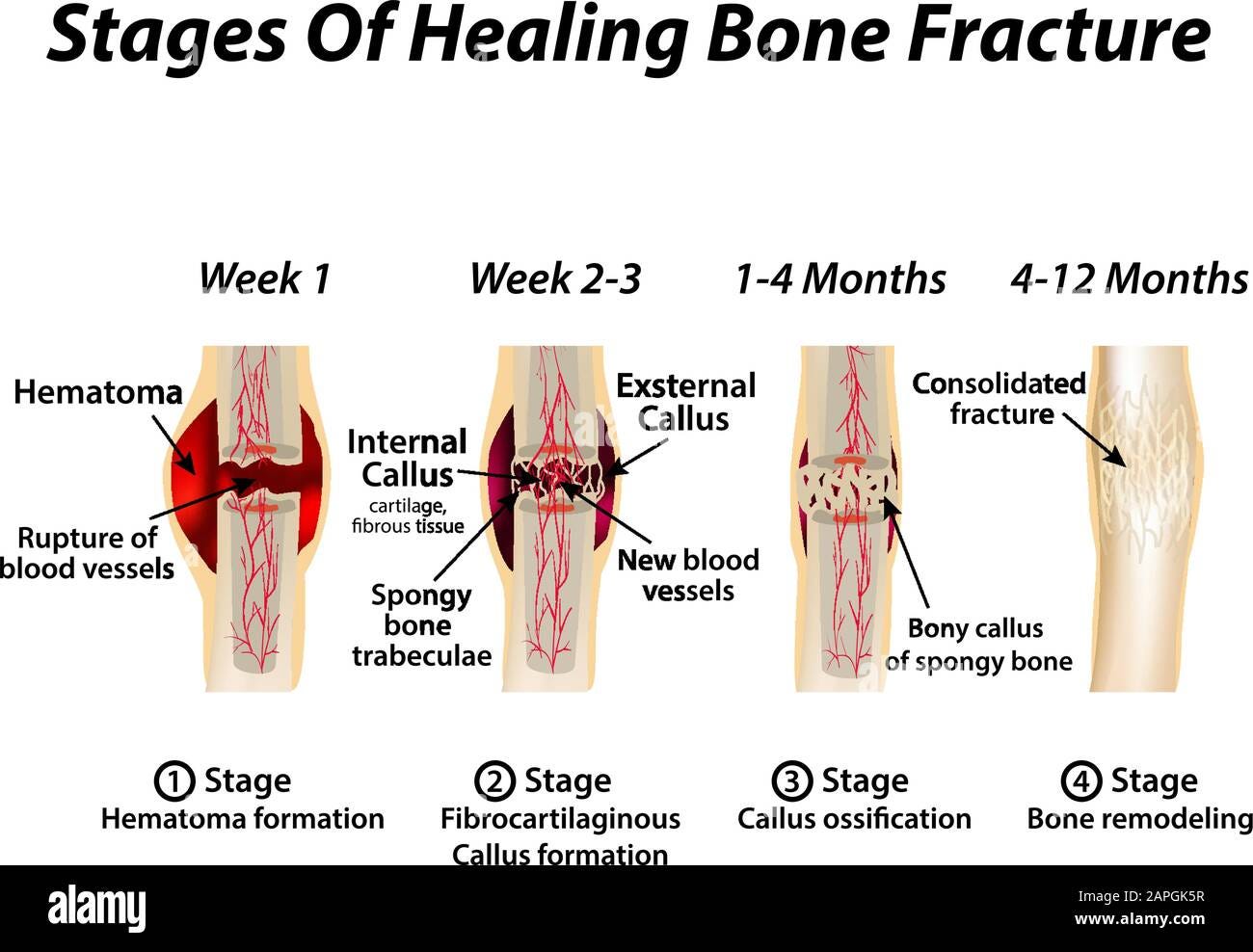
Recovery from bone fractures follows a chronological process (i.e., hematoma/inflammation, cellular proliferation, and remodeling)helping one appreciate the cellular, physiological, and immunological events that occur during healing (Delforge, 2002). Knowledge of the healing process is essential, as it helps reveal the time, place, and form of mechanical loading through movement-based interventions; processes, which continue to restore and enhance the resiliency, density, and function of bone (Delforge, 2002).
Such interventions are necessary, as they help expedite the safe return to activities of leisure (i.e., skiing), and of daily living. Thus, bridging the gap between bone remodeling and return to vigorous movements, such as skiing, is critical for the Exercise Professional to both comprehend and implement in a safe and effective manner.

Bone fractures often require immobilization of the limb to encourage bony union (i.e., bones “connecting” to each other) (Delforge, 2002). Such a process, however, elicits unfavorable side effects; Ceroni et al. (2013) noted that immobilization leads to atrophy, bone loss, and functional limitations in individuals.
Moreover, bone mineral density (BMD) was not only lost at the fracture site; other, more distal regions of the same long bone were also negatively affected (the researchers examined fractured femoral bones) (Ceroni et al., 2013). Ceroni et al. (2013) also stated that there was a BMD loss as high as 50%in adolescents during the first 6-12 months following fracture.
However, BMD returned to pre-injury levels after 18 months (a seemingly long period of time). Such findings emphasize the systemic effect of fractures, which must also be considered when developing a post-rehabilitative program for individuals recovering from bone injuries.

Several steps should occur before introducing a client to a post-rehabilitative program. First, the client should fill out a medical questionnaire, as a means of determining suitability to train, and to support the physician’s decision to embark on a movement-based program.
Secondly, a movement screen should be implemented to “tease out” movement impairments, which has been associated with individuals recovering from extended periods of immobilization, and which can deepen and exacerbate the original injury and dysfunction.
Medically, such a phenomenon has been termed the chronic musculoskeletal pain cycle (Delforge, 2002). Thus, it is this author’s contention that movement impairments should be focused upon first before improving BMD and strength of fractured bones.
Assuming that the medical questionnaire and movement screen confirmed suitability to train (in addition to consent to proceed from the client’s supervising medical professional), there is no presence of severe pain, and movement dysfunctions have been mitigated, this author would begin to include exercises, which would load the bone (for said discussion, it will be assumed the client fractured the femur).
Wolf’s law states that adaptive changes in the structure and mechanics of bone are commensurate with functional demands placed on the bone (Delforge, 2002). Thus, functional demands, in the form of strength training, placed on osseous tissue should elicit increases in BMD, size, and strength over time.

If the client sees this author between 12 and 18 months post-injury (an assumption for argument’s sake), caution would be taken as it has been demonstrated that BMD is still continuing to develop during the aforementioned time frames. Simple walking motions, for example, can create joint forces as high as 6.9 times bodyweight according to Oatis (2016).
Explosive, more dynamic motions, such as jumping and landing (found in skiing) can create forces even higher than that of ADls (i.e., walking) (Cleather, Goodwin, & Bull, 2013). Knowledge of such mechanical findings allows one to appreciate how simple demands (i.e., walking) can load osseous tissue.
It also allows this author to gauge the demands of the client’s chosen leisurely activity (i.e., through the perspective of joint and bone loading) as a means to build the BMD to reach such ends, while respecting the current state and loading capacity of the bone.

Bones work mostly in compression (tensile and torsional loads are also experienced), thus, exercises would be chosen to reflect the same. Motions would also be slow and deliberate, as a means of controlling loading rate, to avoid exposure to abrupt/aggressive increases in forces, which could re-injure the callus (Oatis, 2016).
Muscle contractions would be isotonic in nature, which would include both eccentric and concentric motions. Rationale for inclusion of both contractions is based on the fact that ADLs, and activities like skiing, require both. Target terminal strength exercises would include: bilateral deadlifts/single leg deadlifts (i.e., hip dominant) and split squats/rear foot elevated split squats/single leg squats (i.e., knee dominant).
Eventually, lower body power exercises would also be included to induce greater loads through the femurs (i.e., sagittal plane bilateral jumps to a box/bilateral jumps/single leg jump to a box/single leg jump, in addition to frontal plane plyometrics variations).
However, such exercises require a larger demand from the sensorimotor system, as the degrees of freedom (i.e., coordinating many joints simultaneously) are high. Additionally, the long bones of the femur may not handle loads without the risk of re-fracture, as BMD would still be developing between 12-18 months post-injury (Ceroni et al., 2013).

Simpler exercises that reduce the degrees of freedom and mechanical loading would be introduced initially. Such exercises would include half-kneeling variations (which gently places loads down through each leg) in addition to hip bridges (i.e., hip dominant) in which a larger portion of bodyweight is removed from the femurs, allowing for subtle increases of external load through placing weights across the abdomen.
Bilateral deadlift patterning could be included next (without weight) to prepare the client for larger levels of resistance. Although the aforementioned exercises are simpler in nature, they respect the stages of healing that the callus is undergoing, providing a “base” to build upon, both from a sensorimotor and mechanical loading perspective.
The aforementioned exercises also help circumvent bone fatigue (premature, repetitive, low level forces on bone, which are more likely to cause re-fracture than a high level abrupt force through the bone) (Delforge, 2002). Finally, the exercises acknowledge and target muscle atrophy that has been shown to occur, both proximally and distally, relative to the callus (Ceroni et al., 2003).
In conclusion, knowledge of bone healing has encouraged this author to consider the time, place, and form of mechanical loading; all forms of exercise progressions post-injury (i.e., sets, repetitions, weight, exercise complexity) should be implemented in a slow and pragmatic fashion. In this way, restoring BMD, hypertrophy, activities of daily living, and leisure are expedited in a manner that compliments the stages of healing, while being effective, and safe.
References
Ceroni, D., Martin, X. E., Delhumeau, C., Farpour-Lambert, N. J., De Coulon, G., Dubois-Ferrière, V., & Rizzoili, R. (2013). Recovery of decreased bone mineral mass after lower-limb fractures in adolescents. Journal of Bone and Joint Surgery, 95-A(11), 1037-1043.
Cleather, D. J., Goodwin, J. E., & Bull, A. M. J. (2013). Hip and knee joint loading in vertical jumping and push jerking. Clinical Biomechanics, 28, 98-103.
Delforge, G. (2002). Musculoskeletal trauma; Implications for sports injury management.Champaign, IL: Human Kinetics.
Oatis, C. A. (2016). The mechanics and pathomechanics of human movement (3rded.).New York, NY: Lippincott Williams
-Michael McIsaac
