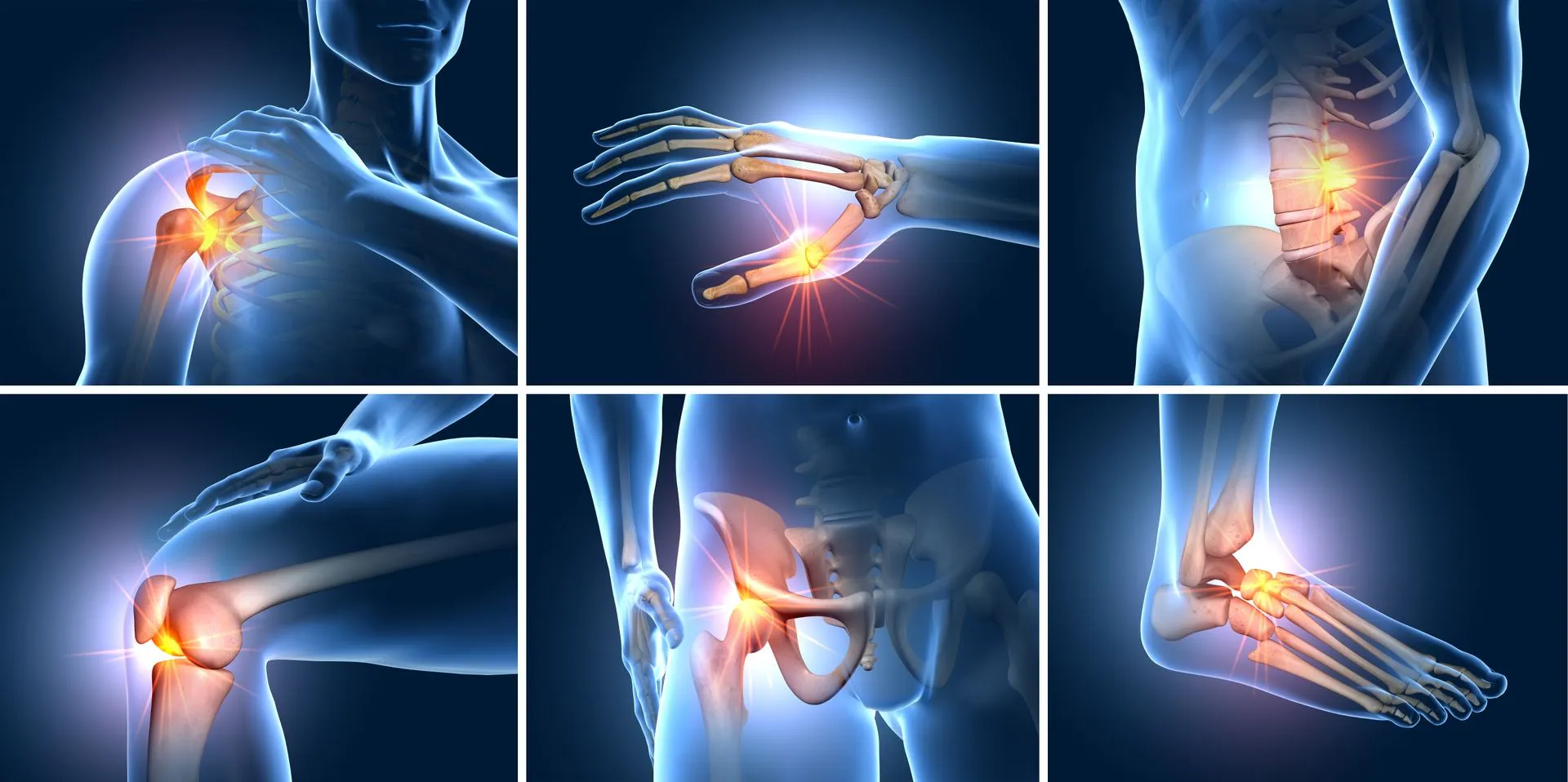
Osteoarthritis (OA) is a degenerative condition characterized by a progressive loss of joint function and increase in joint pain; a disease which tends to affect individuals that are 50+ years of age.1 If such an ailment is left untreated, OA can manifest into a more severe form leaving the afflicted individual with a compromised sense of productivity and quality of life. Ultimately, interventions which help slow said degenerative changes is paramount. Thus, in the following sections, this author would like to explore bromelain as a natural and cost-effective means of helping achieve the same.
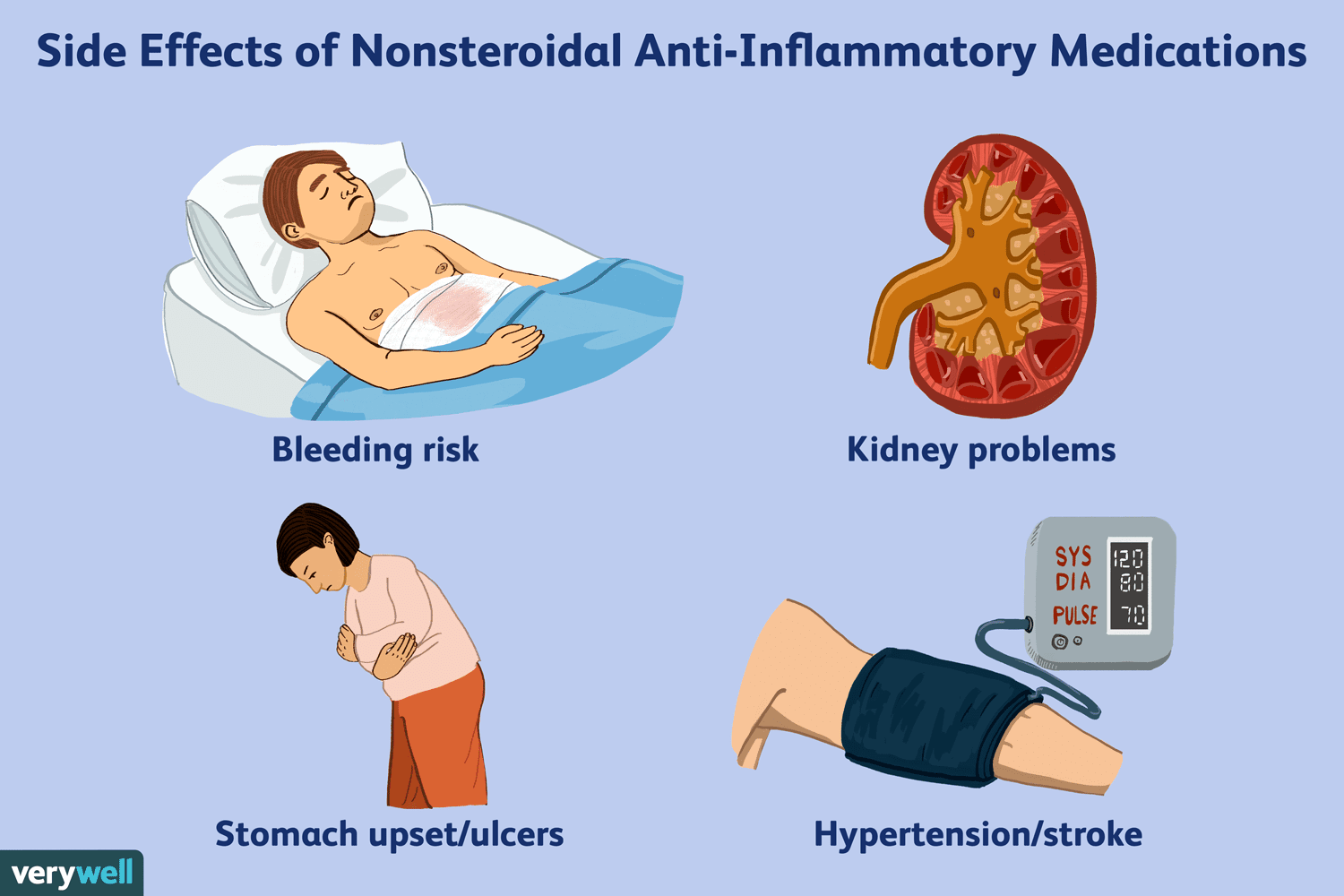
Traditionally, non-steroidal anti-inflammatories (NSAIDs) have been used to reduce pain as well as joint swelling amongst OA patients. However, there is a prevalence of unfavorable side effects (up to 40% of users) from said pharmaceutical to include heartburn, abdominal pain, vomiting, nausea, and dyspepsia (indigestion).2 Furthermore, advanced age (i.e., 65 years) current aspirin use, and previous gastrointestinal issues increase an individual’s chance of experiencing the aforementioned side-effects by approximately 3 to 4 times. Such ailments have made NSAIDs less appealing for individuals managing OA and have increased public interest in a viable and safer alternative. In the following sections, bromelain will be considered as a means of reaching such an end.
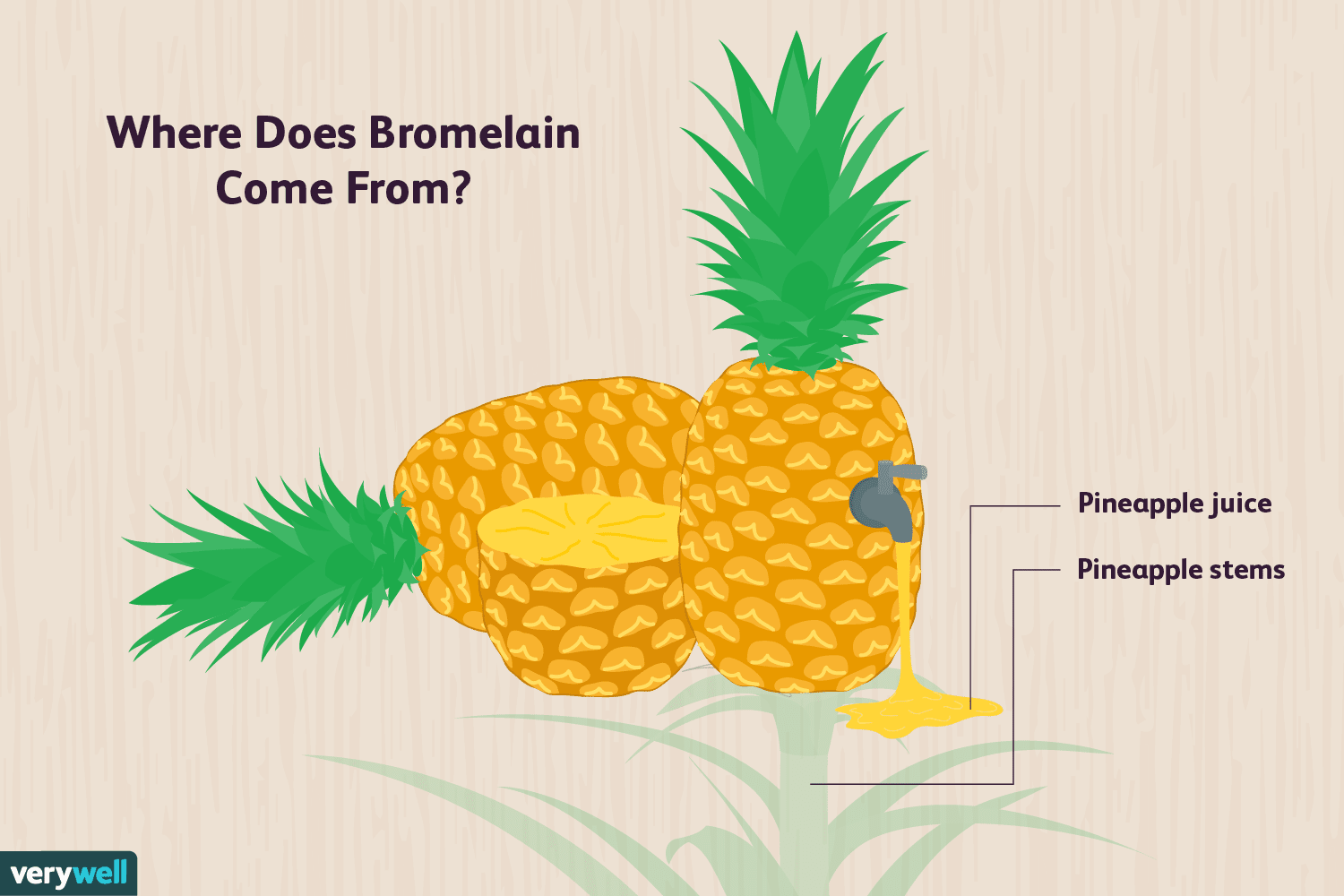
Bromelain is a substance derived from the fruit, and stem, of the pineapple plant containing analgesic (pain-lowering), proteolytic, and anti-inflammatory capabilities.2(2531) Interestingly, bromelain was initially proposed as a treatment intervention for OA, and rheumatoid arthritis, dating back to circa 1964 suggesting its familiarity amongst researchers and clinicians as a viable alternative to NSAIDs.2(2531) Kasemsuk et al2(2531-2532) stated that bromelain is currently implemented as a natural adjunct/replacement treatment for acute inflammation, and has been found to be as equally effective as diclofenac (an NSAID).2(2532) What is less known is the anti-inflammatory/analgesic effects of bromelain for mild-to-moderate knee OA. Thus, in the following sections, this author will explore research exploring the same.
Kasemsuk et al2(2531) constructed a randomized, single-blind, active-controlled pilot study whereby 40 knee OA patients were randomized into two groups: oral bromelain at 500 mg/day or diclofenac at 100 mg/ day. The clinical effectiveness of both interventions was monitored at baseline in addition to week 4 and week 16 of the study period. Kasemsuk et al2(2532) indicated that treatment compliance was checked at each visit by pill counting, while perception of pain and quality of life was captured by questionnaire results using the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) and short form 36 questionnaire (SF36).2(2531) Said WOMAC questionnaire includes 24 items of physical function (0–68), stiffness (0–8), and pain (0–20) while SF36 was assessed using physical and mental component summaries; SF-36 was scored from 0 to 100 (0 = extreme problems, 100 = no problems).2(2532) The following will consider findings in greater detail.

The data suggested no difference in relief (thus, similar effects) measured through WOMAC scores, and quality of life via SF36 data, when comparing bromelain and diclofenac treatments at week 4; both interventions induced an improvement of total WOMAC scores, and the WOMAC pain subscales in knee OA, at the conclusion of week 4.2(2538) However, quality of life (SF36) and functional subscales were improved only in diclofenac group. Interestingly at week 16, patients given bromelain showed additional improvement in physical stiffness, function, and SF36 results when compared to baseline.2(2538)Furthermore, 16-week treatment with 500 mg/day of bromelain was determined as safe, and considered effective in ameliorating symptoms in patients with mild-to-moderate OA.2(2538) Though the sample size was small in said study, preliminary data from bromelain does appear encouraging and may serve as a viable alternative to NSAIDs with less side effects.
In conclusion OA is a degenerative condition characterized by a progressive loss of joint function and increase in joint pain; a disease which tends to affect individuals that are 50+ years of age. If such an ailment is left untreated, OA can manifest into a more severe form leaving the afflicted individual with a compromised sense of productivity and quality of life. NSAIDs have been a traditional intervention to manage OA-related pain, however, such a pharmaceutical’s use has to be tightly weighted against its known side effects discussion previously. Alternatively, bromelain may serve as a viable replacement/adjunct to NSAIDs, specifically for individuals with mold-to-moderate OA. Ultimately, bromelain could allow one to circumvent side effects associated with its pharmaceutical counterpart, while experiencing similar improvements in quality of life and reductions in pain.
References
1. Altamura S, Di Martino A, Andriolo L, et al. Platelet-rich plasma for sport-active patients with knee osteoarthritis: Limited return to sport. Biomed Res Int. 2019:1-6. doi: https://doi.org/10.1155/2020/8243865.
2. Kasemsuk T, Saengpetch N, Sibmooh N, et al. Improved WOMAC score following 16-week treatment with bromelain for knee osteoarthritis. Clin Rheumatol. 2016;35:2531-2540. doi: 10.1007/s10067-016-3363-1.
-Michael McIsaac
