
Laskir et al1 stated that malnutrition is a prevalent condition amongst elderly individuals with type 2 diabetes (T2D) in hospital and geriatric care settings. As such, nutritional management is critical especially in the presence of acute disease, severe co-morbidities, and functional status; all of which are likely amongst geriatrics with T2D.1(2084) Therefore, developing nutritional protocols that manage both macro and micronutrient deficiencies, while maintaining optimal blood glucose levels, is paramount. As a means of appreciating such protocols, the following will explore the same, with particular emphasis on the role of slowly digested carbohydrates/higher fiber consumption in controlling blood glucose spikes.

Laskir et al1(2084) indicated that although oral nutrition supplements currently implemented amongst elderly individuals help manage nutrient deficiencies, they tend to result in high post-prandial blood glucose excursions; a characteristic feature in insulin resistance and, ultimately, T2D. Left unmitigated, high blood glucose can manifest into glucosuria (sugar in urine), a loss of energy substrates, increased risk of infections, and urinary incontinence.1(2085) Thus, reducing said excursions is paramount not only for patient safety, but also for reduced patient stay (if in hospital settings), improved quality of life, and health care resource savings.1(2085) The following will consider the use of diabetic formulas (DFs) to control malnutrition and glucose spikes in greater detail.
Nutritional requirements for the aforementioned population are met by specifically designed DFs. In the past, DFs contained ingredients high in monounsaturated fatty acids and high fructose designed to limit glucose spikes as much as possible.1(2085) Furthermore, evidence supported that DFs, when compared with standard formulas, improved blood glucose levels.1(2085) However, the caveat was that fructose concentrations and fat energy contributions of more than 35% had the potential to negatively affect nutritional guideline compliance and lipid metabolism. Today, most DFs have a lower energy % of fat with slow digestible carbohydrates.1(2085) Though an effective approach, the researchers considered the impacts of higher fiber content/slowly digested carbohydrates in DFs and post-prandial blood glucose spikes compared to current protocols. The following will consider the results from Laskir et al.1(2085)
20 patients for the study were recruited in rehabilitation centres, hospitals, and nursing homes. Inclusion criteria considered patients that were equal to or over 18 years of age and diagnosis with T2D for a minimum six months (prior to study entry) and on stable anti-hyperglycaemic therapy (oral medication and/or insulin) for a minimum of 1 month prior to study.1(2085) The study was a randomized, double blind, crossover design in which, after overnight fasting, patients drank 200 mL of a DF or standard supplement (control) (10.6 g fat, 19.6 g protein, 31.2 g carbohydrates), while continuing anti-diabetic medication.1(2085) The formulas differed in type of carbohydrates and presence of fibre. The postprandial glucose, insulin and glucagon responses were monitored over 4 h. Please see chart below outlining the DF and control formula.
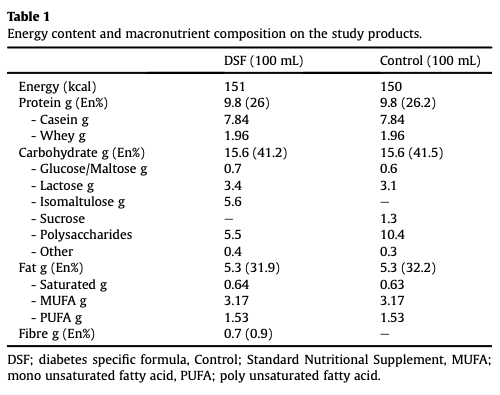
Laskir et al1(2086)
The researchers attempted to match, as closely as possible, caloric content, type and energy % of protein and type and energy % of fat when comparing the control formula and DFs. The DF substituted a percentage of the carbohydrates with isomaltulose; a disaccharide that is slowly digested.1(2086) When comparing post-prandial glucose responses between the intervention (DF) group and the control group, the DF group had significantly lower blood glucose spikes.1(2089) Such results are further supported by other studies that compared and isomaltulose to sucrose (a commonly used sugar); isomaltulose was shown to control blood glucose, and insulin, spikes when compared to sucrose (a commonly used sugar).1(2086)
In conclusion, malnutrition is a prevalent condition amongst elderly individuals with type 2 diabetes (T2D) in hospital and geriatric care settings. As such, nutritional management is critical especially in the presence of acute disease, severe co-morbidities, and functional status; all of which are likely amongst geriatrics with T2D. Results from the above study indicated the effect, and need, of slowly digested carbohydrates (isomaltulose) and higher fiber diets as a means of controlling blood sugar spikes and the prevalence of glucosuria. Considering the ease, cost-effectiveness, and efficacy of introducing fiber and slowly digested carbohydrates, such information should help encourage the implementation of the same amongst individuals with T2D/insulin resistance.
References
1. Laskir H, Lansink M, Regueme SC, et al. Glycemic response after intake of a high energy, high protein, diabetes-specific formula in older malnourished or at risk of malnutrition type 2 diabetes patients. Clin Nutr. 2018;37(6):2084-2090. doi:https://doi.org/10.1016/j.clnu.2017.09.027.
-Michael McIsaac
