
The cardiovascular system serves many important functions, and supports every other physiological system. The more positive adaptation the cardiovascular system experiences, the more proficient it can fulfill its roles. Conversely, a diseased cardiovascular system will hinder all other physiological processes. I would like to briefly review the functions of the cardiovascular system, look deeper into associated pathophysiological states, and cover corresponding etiologies.

The cardiovascular system is composed of the heart, blood vessels, and blood (Kenney, Wilmore, & Costill, 2012). Synergistically, these systems perform several central tasks: delivery of oxygen, removal of metabolic byproducts, hormone transfer, thermoregulation, acid-base balance, and regulation of immune function (Kenney et al., 2012). In essence, the cardiovascular system could be viewed as a framework that all other physiological systems are supported by. It would seem logical, then, that any aberration of this system would evoke deleterious effects on all other physiological processes.

Coronary heart disease (CHD) is associated with a narrowing of the arteries through plaque accumulation, or atherosclerosis, which supplies the heart muscle, or myocardium. It is characterized by a progressive narrowing of the arterial walls that can begin as early as infancy (Kenney et al., 2012). As this process worsens, the heart fails to receive the appropriate nutrients necessary for the workload placed upon it. If workload remains unchanged, the heart enters an ischemic state, thereby experiencing a deficiency of blood. This can induce sensations of pain in the chest region, approximate to the heart (Kenney et al., 2012). If additional narrowing of the arteries continues and/or workload increases, worsening ischemia can lead to a heart attack, or myocardial infarction (Kenney et al., 2012). This causes cell death, or necrosis, which is permanent and irreversible. The etiology of CHD is multifactorial, and the rate at which CHD progresses is determined largely by genetics and lifestyle factors. Some of these include smoking history, diet, physical activity, and stress. CHD accounts for 51% of deaths from cardiovascular disease (Kenney et al., 2012).
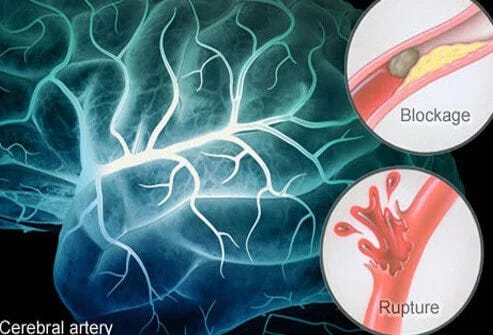
Stroke accounts for 17% of total deaths from cardiovascular disease, and was associated with 232,000 deaths in 2006 (Kenney et al., 2012). This particular disease negatively affects the arteries supplying the brain, or cerebral arteries. There are two major categories of strokes: ischemic and hemorrhagic. In an ischemic stroke, blood flow is restricted or completely halted. In a hemorrhagic stroke, a vessel ruptures diverting flow away from the target tissue. Despite the unique mechanisms of ischemic and hemorrhagic strokes, their outcomes remain common: blood flow is restricted to regions of the brain (Kenney et al., 2012). Much like a myocardial infarction, diminished blood flow evokes cell death, or necrosis. Stroke along the right side of the brain will effect or cause paralysis on the left side of the body, vision problems, quick and inquisitive behavioral style, and memory loss (Kenney et al., 2012). Necrosis to the left side of the brain causes paralysis along the right side of the body, speech and language problems, slow and cautious behavioural style, and memory loss (Kenney et al., 2012).
Hypertension refers to chronic higher-than-normal blood pressure, and is heavily influenced by body size (Kenney et al., 2012). Consequently, children generally have lower blood pressure than adults. For adults, normal blood pressure is considered 120/80 (mmHg). Pre-hypertension is considered 120-139/80-89, and hypertension is considered 140-159/90-99 (Kenney et al., 2012). Over time, the heart has to produce more force per heartbeat to evacuate blood from the ventricles. This causes an enlargement of the cardiac muscle. Moreover, associated arteries and arterioles become scarred, hardened and less elastic. As these degenerative processes continue, they often lead to atherosclerosis, myocardial infarctions, heart failure, stroke and kidney failure (Kenney et al., 2012).
Heart failure is the fourth CHD related disorder. It is characterized by a failure of the myocardium to maintain adequate cardiac output to target tissues. It is usually the product of damage to, or overworking of, the heart (Kenney et al., 2012). Many other diseases cause heart failure such as hypertension, viral infection, valvular heart disease and heart attack. It should also be noted that hypertension precedes 75% of heart failures (Kenney et al., 2012).
The cardiovascular system plays many central roles to other physiological systems within the body. Failure of either, or all, of its constituents (heart, blood, blood vessels) will severely hamper homeostasis of the human movement system. Recognizing the diseased states of the cardiovascular system not only allows us to understand its pathophysiology: it enables us to more deeply appreciate, respect, and protect a well working cardiovascular system.
References
Kenney, W. L., Wilmore, J. H., & Costill, D. L. (2012). Physiology of sport and exercise (5th ed.). Champaign, IL: Human Kinetics.
-Michael McIsaac
