Brown (2014) indicated that overweight and obesity (OO) are conditions among children that are mounting at an accelerated rate. Moreover, approximately 18% of children aged 6-11 are obese with BMIs greater than or equal to the 95th percentile (Brown, 2014).
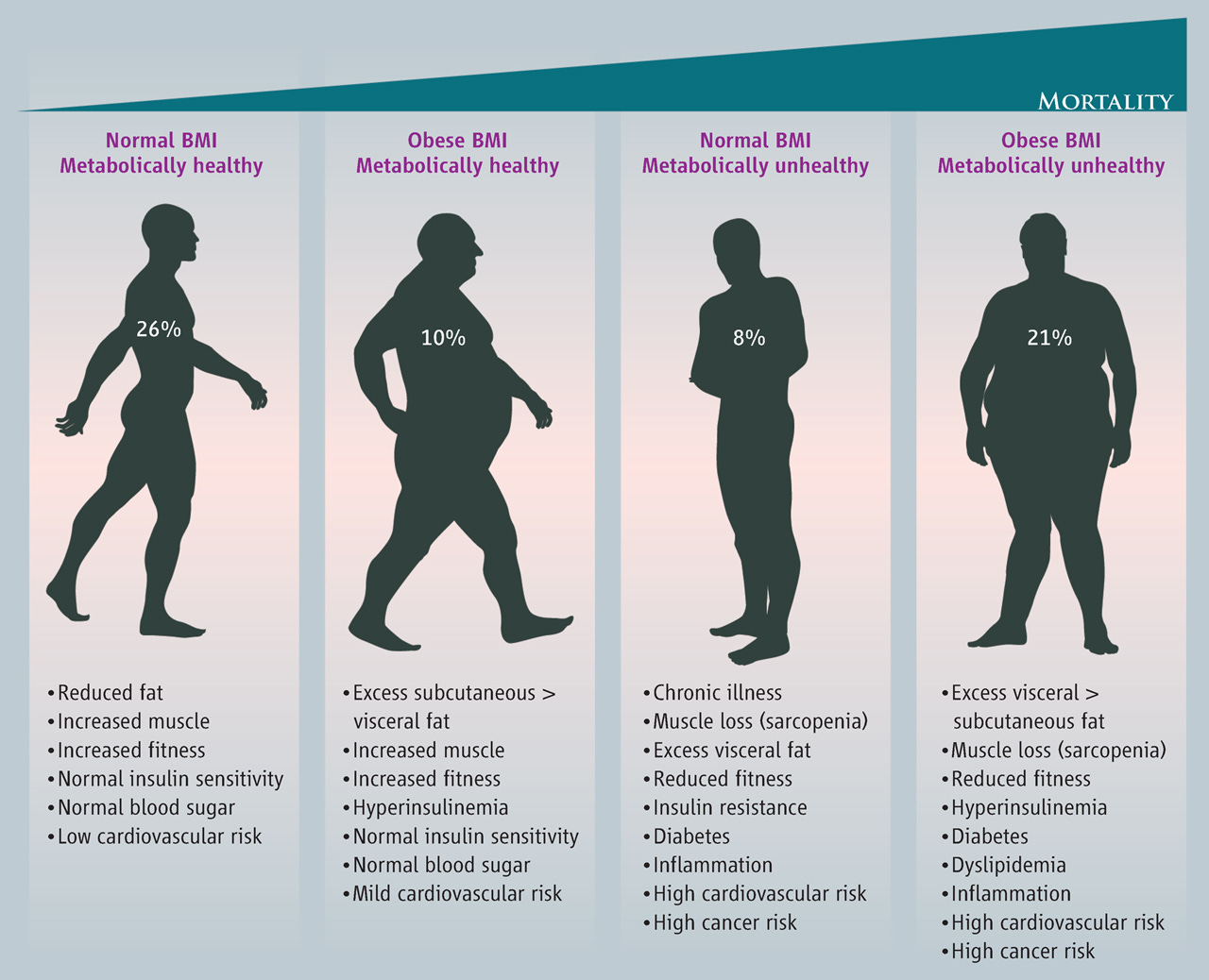
Conditions of overweight and obesity set a foundation for other physiological aberrations such as cardiovascular disease and type 2 diabetes mellitus. As an aggregate, said conditions are linked by common risk factors such as large waistline, high triglyceride levels, low high-density lipoproteins, high resting blood pressure, high levels of blood sugar/insulin resistance, and low-grade chronic inflammation (Kenney et al., 2012; National Heart, Blood, and Lung Institute, 2017). Thus, it is imperative to develop strategies to prevent the genesis of said risk factors.
Brown (2014) indicated that prevention and management can occur throughout a child’s life, but can begin relatively early. BMI rebound is a normal increase in BMI that occurs after BMI declines and reaches its lowest point at 4-6 years of age. Research has suggested that BMI rebound occurring before 5.5 years of age is strongly correlated to development of obesity later in life. Thus, early intervention is critical. Brown (2014) suggested that childhood OO should be addressed by three methods: assessment, prevention, and treatment.
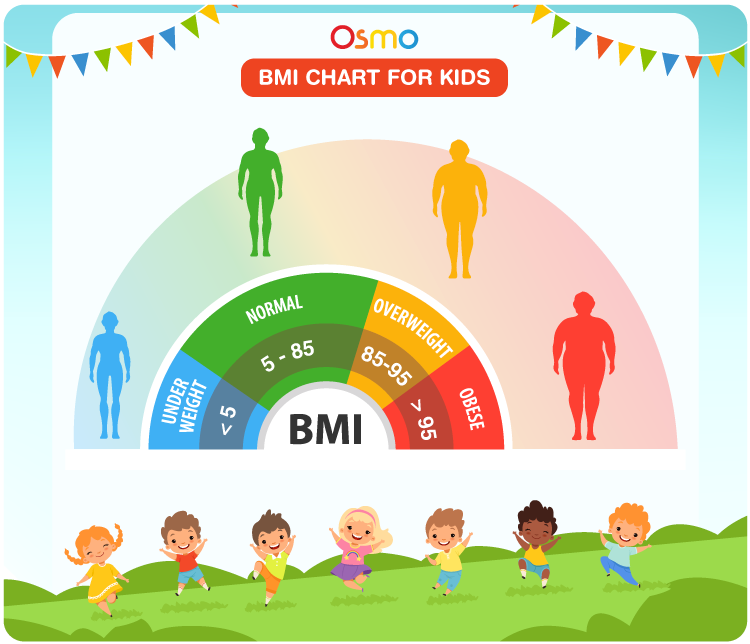
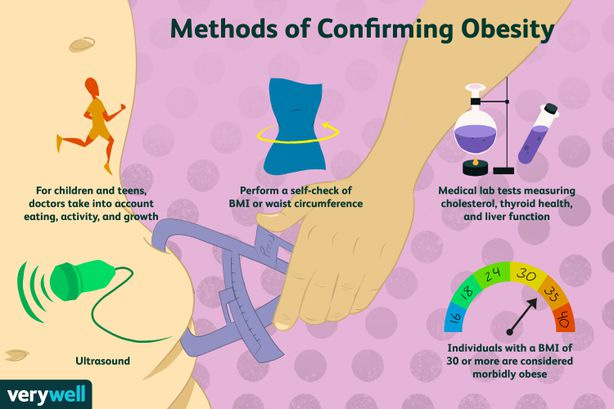
Assessment includes implementation of BMI; if BMI-for-age percentile is between the 85th and 94th, the child is considered overweight. If the BMI-for-age percentile is equal to or greater than 95th, the child is considered obese. Other components of the assessment could include an evaluation of the child’s medical risk, in addition to dietary behaviours, physical activity behaviours, in addition to the family’s attitude towards health

Prevention of OO includes healthy nutrition and physical activity including: limiting sugar based beverages, increasing vegetable and fruit consumption, limiting television to less than 2 hours a day, eating breakfast, limiting fast food, limiting portion sizes, eating foods rich in calcium, consumption of fibre, promoting vigorous activity 60 minutes a day, and limiting energy dense foods (Brown, 2014).

Treatment of OO can be broken down into four main stages: Prevention plus (PP), structured weight management (SWM), comprehensive multidisciplinary intervention (CMI), and tertiary care intervention (TCI) (Brown, 2014). PP is characterized by identifying physical and nutritional behaviours that would be set as goals for the child, in addition to including the family in a support system (Brown, 2014). SWM is a progression of prevention plus in that it includes a planned diet with restrictions on television time (<1hour) and includes the expertise of a registered dietician to continually assess and monitor the child (Brown, 2014). CMI is characterized by an increase in intensity of structure and goal setting, with the presence of a multidisciplinary team. Said stage also includes food monitoring, short-term diet that has a negative energy balance, and physical activity goal setting (Brown, 2014). TCI is for severely obese children who have filed the first three stages outlined. However, TCI is not appropriate for toddlers or preschool children (Brown, 2014).
In conclusion, it is imperative to be aware of the early signs of OO. This author would begin by encouraging parents to value their personal health as much as their child who is OO, as a means of developing a fertile environment for long-term behaviour change. Providing education on the negative impacts of starchy-carbohydrate-rich foods and positive benefits of physical activity/whole foods (meat, fish, poultry, dairy, vegetables, and fats) and optimal hydration would be paramount. Such interventions and methods would provide a cornerstone for meaningful and sustainable lifestyle changes for the child and family.
References
Brown, J. E. (2014). Nutrition through the life cycle (5th ed.). Stamford, CT: Cengage Learning.
Kenney, W.L., Wilmore, J.H., & Costill, D.L. (2012). Physiology of sport and exercise (5th ed.). Champaign, IL: Human Kinetics.
National Heart, Blood, and Lung Institute (2011). What is metabolic syndrome? Retrieved April 4, 2017, from http://www.nhlbi.nih.gov/health/health-topics/topics/ms/
-Michael McIsaac
