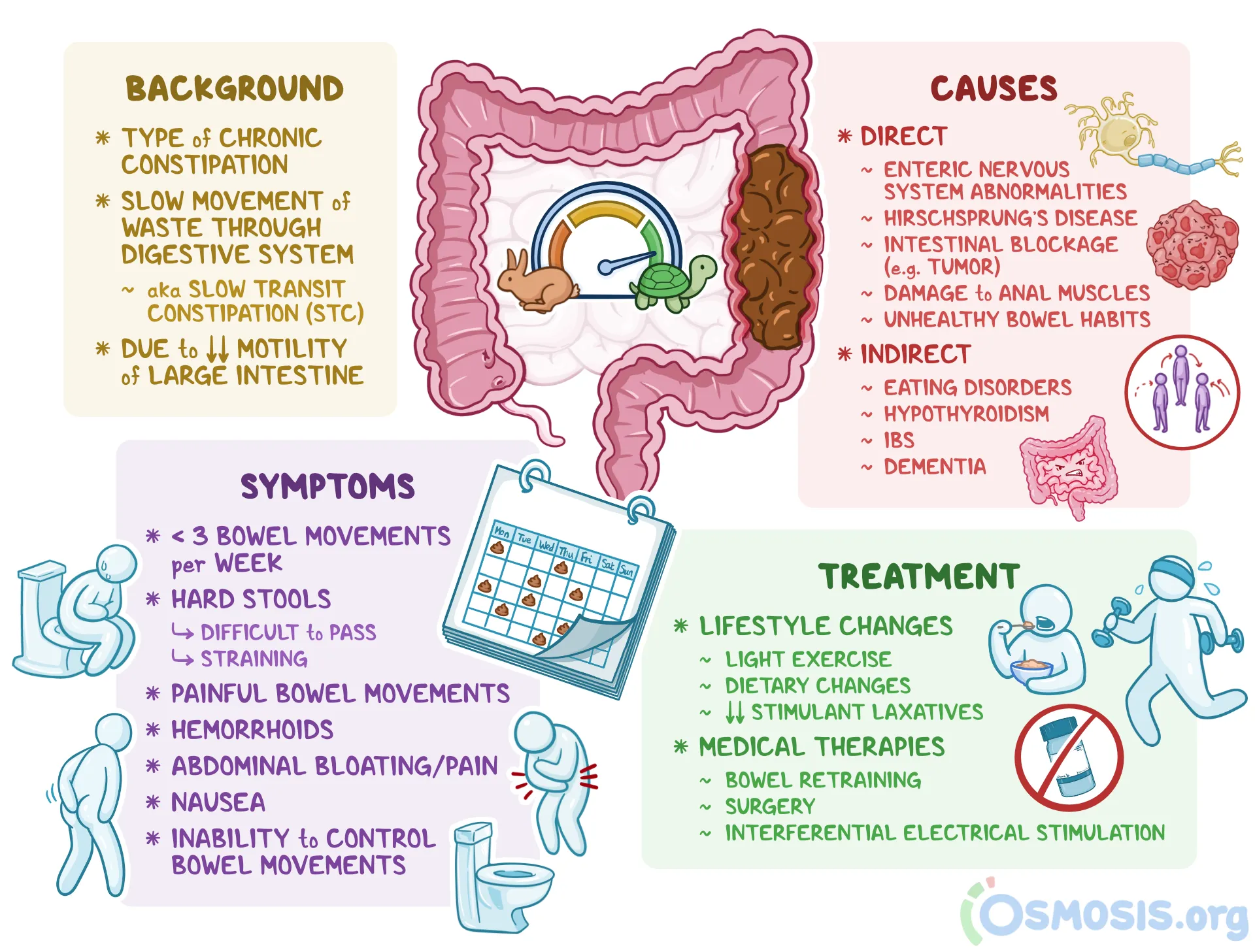
Functional constipation (FC) is a condition in which a complete understanding of its pathophysiology remains equivical.1 Conventional thoughts behind FC involves slow transit time and/or pelvic floor impairment, however, Cirillo et al1(1489) stated that there are wide variations behind the precise identification of the dysfunction. Currently, most individuals with FC experience significant impairments to quality of life while the healthcare system experiences economic challenges from the same.1(1489) As such, it is imperative to develop effective and low-cost interventions to manage FC. As a means of appreciating the effectiveness of such interventions, the following will explore in vivo animal studies and consider flax seed as a method of managing FC.
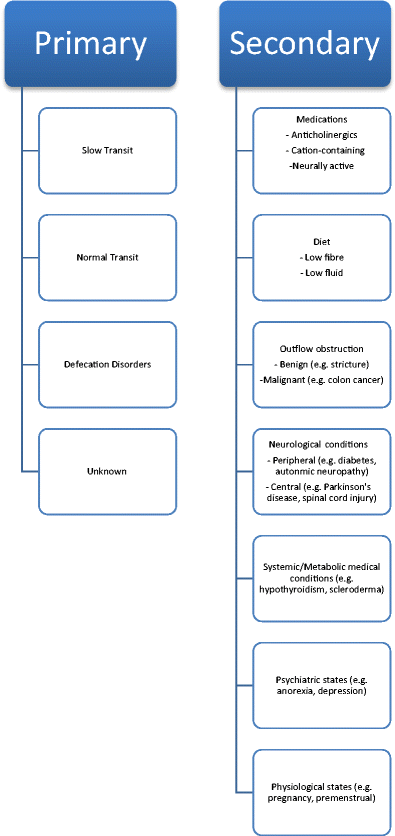
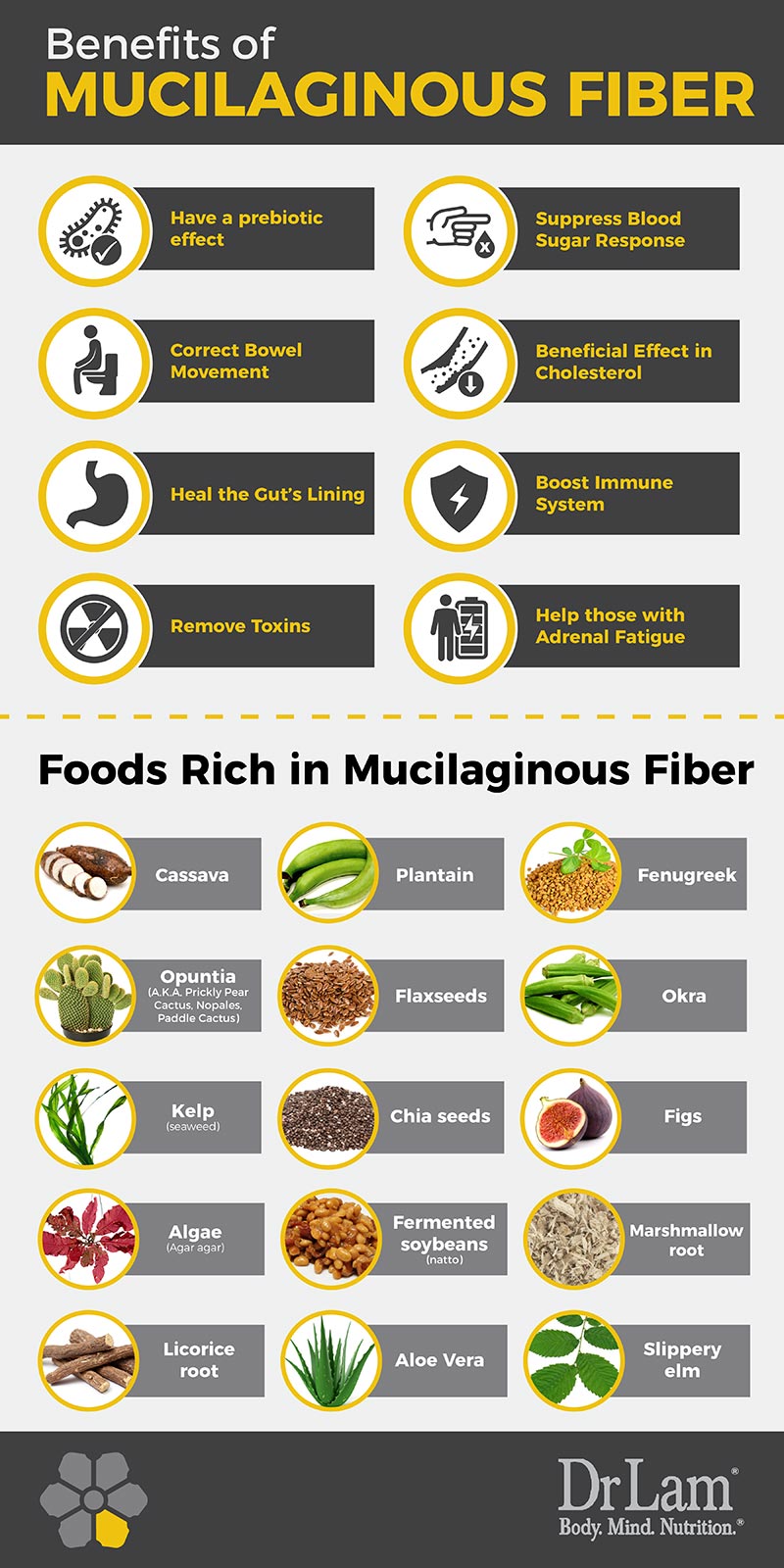
FC can have primary and secondary causes and are also associated with irritable bowel syndrome (IBS).2 Constipation, left unmanaged, can also cause bowel perforations (leading to bleeding and sepsis) as well as fecal impaction, rectal prolapse, anal fissures, and hemorrhoids.2(60) Plants and plant extracts have been implemented for therapeutic purposes for centuries, and many pharmacological drugs are predicated off of the oils and extracts from herbs.2(60) Of particular interest is flaxseed, also known as Linum usitatisimum; a functional food whose mucilage, oil, and seeds have been used for a multitude of purposes to include gut motility.2(61) Most research has suggested flaxseed improves transit time due to its ability to add bulk to stools. However, researchers are also questioning whether flaxseed confers benefits to the user by its oils, and mucilaginous components binding with water, causing stool to swell and become lubricated (aka lubricant laxative).2(61)

As a means of exploring the other proposed benefits of the aforementioned flaxseed constituents, the researchers chemically/mechanically separated flaxseed oils and mucilage.2(61)Furthermore, BALB-C mice, guinea pigs, and local breed rabbits were used to carry out the study; animals were fed regularly but were fasted 6 hours before determining the laxative activity.2(62) Regarding the flaxseed oil study, animals were split into 10 groups (10 animals per group).2(62)Group 1 was a negative control which received DMSO and Tween-80 (both used for solubilization) in distilled water at 10 ml/kg.2(62)Group 2 received carbachol at 1 mg/kg serving as a positive control.2(62) Groups 3,4,5 received flaxseed oil orally at 30, 70, 100 mg/kg doses.2(62) Groups 6, 7, 8, 9, 10 were treated with atropine (induces constipation) before being administered the vehicle, carbachol, or flaxseed oil.2(62) After 24 hours, the researchers analyzed feces production (dry and wet) of all animals and the percentage increase in wet feces compared to total fecal output was accounted for, which was considered the laxative effect.2(62)
Palla et al2(62) explored the mucilage effects of flaxseed by implementing a similar approach as mentioned above. However, the animals were divided into 8 groups (6 animals per group) where group 1 was the negative control group receiving a vehicle of 10 ml/kg while group 2 received carbachol at 1 mg/kg serving as the positive control group.2(62) Groups 3 and 4 received flaxseed mucilage doses of 1 g/kg and 2.5 g/kg while groups 5, 6, 7, 8 received atropine before oral dosing of flaxseed mucilage.2(62) The laxative effect was analyzed by monitoring the percentage of wet feces.2(62) The researchers also indicated that they categorized wet stool quantitatively based on stool frequency and consistency and also considered diarrheal stool as the highest score (3) while soft but formed stools were scored lower (1).2(62) Having considered the design of flaxseed oil and flaxseed mucilage studies, the following will consider the results of the same in greater detail.
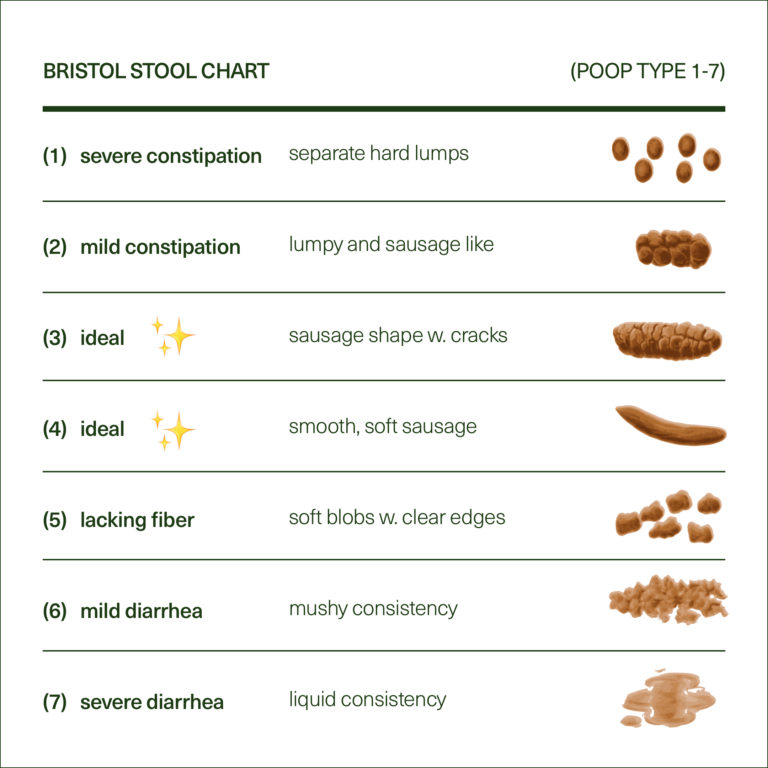
Flaxseed oil treatments produced a dose-dependent increase in wet stool when 30 mg/kg and 70 mg/kg was used; higher doses of 100 mg/kg declined said effect.2(63) In the positive control group, carbachol produced approximately a 75% increase in wet feces while pre-treatment of animals with atropine at 10 mg/kg partially blocked the laxative effects of the flaxseed oil.2(63) Flaxseed mucilage studies also produced laxative effects at higher doses of 1 g/kg and 2.5 g/kg and created an increase of approximately 65% and 89% in wet feces compared to normal values.2(63) However, the effects of flaxseed mucilage were reduced in the presence of atropine suggesting that atropine blocks muscarinic receptor activation, and that the effects of mucilage is of a chemical nature and not an exclusive bulk-forming effect.2(65) Palla et al2(67) also suggested that flaxseed mucilage and oil exhibited cholinergic (increase contractions) and histaminergic (modulates gastrointestinal motility) effects which are likely to play a role in heightened gut motility.3,4
In conclusion, FC) is a condition in which a complete understanding of its pathophysiology remains unclear. Conventional thoughts behind FC involves slow transit time and/or pelvic floor impairment, however, there are wide variations behind the precise identification of the dysfunction. Left unmitigated, FC can lower individuals’ quality of lives and increase risk of bowel perforations, fecal impaction, rectal prolapse, anal fissures, and hemorrhoids. Despite such a seemingly undesirable prognosis, natural interventions do exist which can help improve gut motility, such as flaxseed oil and flaxseed mucilage. When combined with proper hydration, a high fiber diet, and exercise, it is likely that such lifestyle changes would induce a synergistic effect supporting improved gastrointestinal function, in addition to overall health, performance, and longevity.
References
1. Cirillo C, Capasso R. Constipation and botanical medicines: An Overview. Phytother Res. 2015;29:1488-1493. doi:10.1002/ptr.5410.
2. Palla AH, Gilani AH. Dual effectiveness of flaxseed in constipation and diarrhea: Possible mechanism. J Ethnopharmacol. 2015:169:60-68. doi:10.1016/j.jep.2015.03.064.
3. Parkman HP, Trate DM, Knight LC, et al. Cholinergic effects on human gastric motility. Gut. 1999;45:346-354. doi:10.1136/gut.45.3.346.
4. Fabisiak A, Wlodarczyk J, Fichna J. Targeting histamine receptors in irritable bowel syndrome: A critical appraisal. J Neurogastroenterol Motil.
2017;23(3):341-348. doi: https://doi.org/10.5056/jnm16203.
-Michael McIsaac
