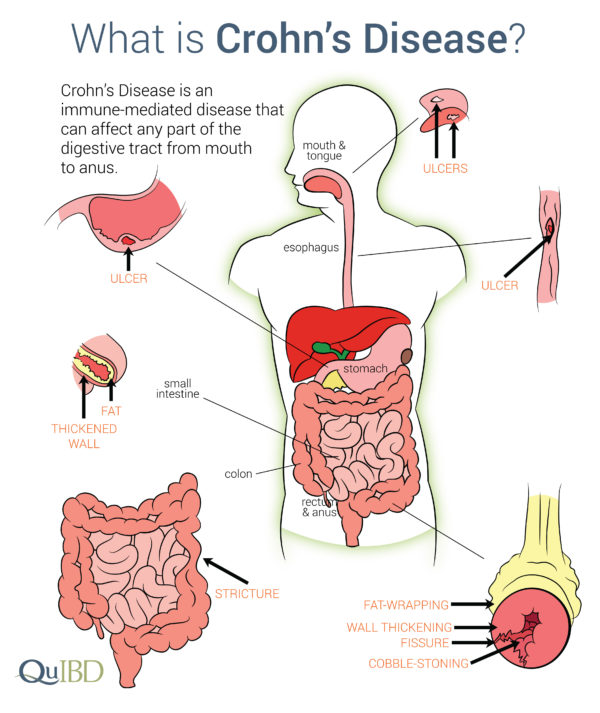
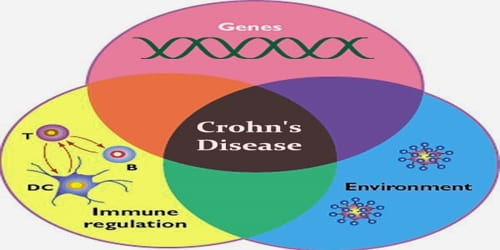
Crohn’s disease (CD) is a condition characterized by chronic and inflammatory episodes, which can affect any section of the digestive tract.1 Furthermore, 30-65% of CD patients exhibit a secondary condition known as intestinal permeability (IP); a pathophysiological aberration in tight junction (TJ) integrity.1(1000) TJs represent the space between intestinal cells (enterocytes) that, in normal and healthy individuals, are relatively small impermeable regions of the gut. Ultimately, both characteristics of CD negatively affect the health and quality of life amongst individuals with said disease. In the following sections, CD will be explored in greater detail in addition to diagnostic tests, and nutritional interventions to improve underlying causes and symptoms.
When considering options to improve CD, the first step would be identification of triggers (i.e., food, past use of antibiotics), which may exacerbate/irritate said condition. As such, if clients report intestinal pain/discomfort after eating particular foods, this author would suggest abstinence of said foods in the diet. Furthermore, this author would also recommend a formal food allergy test to determine moderate and severe reactions (measured by the concentrations of IgG antibodies) to common foods in the diet.2 If such strong immune reactions to foods are elucidated, removal of the same from the diet would be recommended. Such steps would represent phase one of the Four R (Remove, Reintroduce, Reinoculate, Repair) program, also known as FRP.2(454) Having considered food triggers and their affects upon CD and inflammation, the following will explore particular microbes and their relationship to intestinal inflammation.
SUMMARY:
Conduct a food allergy test
Remove allergenic foods, if present

Phase one of FRP also involves identification and control of overpopulated/pathogenic microbes lining the gastrointestinal tract (GIT). Such can be achieved by utilizing a polymerase chain reaction test; a process which identifies DNA/RNA unique to each microbe, like a fingerprint of an individual.2(448) If Pseudoflavonifractor spp. (bacteria), Oxalobacter formigenes (bacteria), Geotrichum species (fungus), or Chilomastix mesnili (parasite) are present and in abundance, steps should be taken to lower/eradicate said microbes. For example, Candida species and Geotrichum species have been implicated in the pathogenesis of inflammatory bowel syndrome, of which CD falls under.3 One technique to reduce colonization of Geotrichum would be a reduction of carbohydrates, as evidence suggests that fungus tends to proliferate in carbohydrate-rich mediums.2(446) Oil of oregano and caprylic acid can be helpful in controlling fungal overgrowth.2(390) Finally, introduction of antibacterial agents such as berberine, citrus seed extract, and garlic can help control overgrowth of the other aforementioned microbes.2(390)
SUMMARY:
Conduct a stool test for dysbiosis
Conduct organic acids test for dysbiosis
Remove foods which drive overpopulated fungal/microbial species
Implement anti-fungal (caprylic acid, oil of oregano) and antibacterial agents (garlic, berberine, citrus seed extract) if such are present
Following identification and control of food triggers and gut microbes, it is essential to reintroduce digestive enzymes, if deficient; such a process represents phase two (Reintroduce) of FRP.2(454) If fecal pancreatic elastase 1 (FE1) is less than 200 mcg/g, such would suggest pancreatic insufficiency and oral supplementation of digestive enzymes would be warranted. However, if FE1 levels are optimal (>200) such steps are unnecessary.4 It should be noted that stool may still present with high levels total fecal fat and high phospholipids despite normal levels of FE1; such a situation is likely to suggest poor absorption rather that compromised digestion.2(422) Such can be supported by inflammatory markers to include high calprotectin and high eosinophil protein X (EPX); markers which indicate intestinal inflammation, which is tightly associated with IP, and can help differentiate CD from functional intestinal disorders like irritable bowel syndrome (IBD).2(427) Once poor digestion and IP/inflammation is determined, steps to improve barrier function and reduce inflammation is warranted.
SUMMARY:
Conduct a fecal elastase test
Consider digestive enzymes for breakdown of carbohydrates, fats, and proteins
Check calprotectin and eosinophil protein x if loose stools persist in presence of adequate fecal elastase / supplemental digestive enzymes
Improving IP and minimizing intestinal inflammation can be achieved by introducing beneficial microbes, which represents phase three (reinnoculate) of FRP.2(454) Probiotics are microorganisms which share a beneficial/harmonious relationship with the GIT. Such microbes facilitate the prevention of diseases (i.e., inflammatory bowel disease and antibiotic associated diarrhea), modulate immune system function, enhance epithelial barrier function, and control the build-up of toxin-producing bacteria.5 Lord et al2(455) suggested implementation of favorable microbes to control general dysbiosis using L. acidophilus, L salvarius, L. plantarum, L. casei, and Saccharomyces boulardi. Furthermore, use of Saccharmyces boulardii can help control fungal overgrowth while soluble and insoluble dietary fibers would help feed said beneficial microbes and increase short chain fatty acid/butyrate production (provides energy for colonic cells).2(451,455)
SUMMARY:
If dysbiosis is determined (from stool and organic acids tests), introduce probiotics
If inflammation is present (from calprotectin and eosinophil protein x tests), introduce omega-3 fatty acids
Implement high fiber foods as precursors to synthesis of short chain fatty acids (food for colonic cells)

Phase four (Repair) of FRP would represent the final step in GIT support. Said phase would include introduction of nutrients designed to facilitate repair of the intestinal epithelial layer, goblet cells (secrete mucus), and immune cells.2(454) Glutamine is an amino acid, which serves as a major fuel and nitrogen source for enterocytes; cells which become damaged from CD.1(1001) Moreover, glutamine prevents IP/bacterial translocation/cell death and maintains mucosal integrity indicating the need for appropriate levels, especially amongst individuals with inflammatory bowel diseases like CD.1(1001) As mentioned in previous posts, essential fatty acids such as docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) could help remodel cell membranes/control inflammation along the intestinal wall in addition to supplementing with vitamin A/C/E, folic acid, zinc pantothenic acid (B5), and free form amino acids to support cell growth and protection.2(455)
SUMMARY:
Introduce supplemental glutamine if inflammation is present (calprotectin and eosinophil protein x tests)
Introduce omega-3 fatty acids if inflammation is present
Introduce vitamins A/C/E/B5, zinc, and free form amino acids if inflammation is present

In conclusion, CD is a condition characterized by chronic and inflammatory episodes, which can affect any section of the digestive tract. Furthermore, 30-65% of CD patients exhibit a secondary condition known as intestinal permeability (IP); a pathophysiological aberration in TJ integrity. Such conditions can negatively affect the health and quality of life amongst individuals with said disease. However, solutions do exist which can support restoration and repair of gut function; once CD been diagnosed, removal of irritating foods and pathogenic microbes is essential in controlling factors that could be contributing to said condition. Introduction of digestive enzymes (when indicated), beneficial microbes, essential fatty acids, amino acids, and other micronutrients is critical to reduce inflammation and support digestion, absorption, and repair of the intestinal tract. Ultimately, such steps when guided by FRP, can help reduce signs, symptoms, and underlying causes of CD.
References
1. Benjamin J, Makharia G, Ahuja V. Glutamine and whey protein improve intestinal permeability and morphology in patients with Crohn’s disease: A randomized controlled trial. Dig Dis Sci. 2012;57:1000-1012. doi: 10.1007/s10620-011-1947-9.
2. Lord RS, Bralley JA. Laboratory Evaluations for Integrative and Functional Medicine. 2nd ed. Duluth, GA: Genova Diagnostics; 2012.
3. Sam QH, Chang MW, Chai LYA. The fungal mycobiome and its interaction with gut bacteria in the host. Int JMol Sci. 2017;18(2):1-11. doi:10.3390/ijms18020330.
4. Amanquah SD, Darko R, Maddy SQ, et al. Fecal pancreatic elastase – 1: A non-invasive measure of exocrine pancreatic function.WAJM. 2004;23(3):240-244. doi: http://dx.doi.org/10.4314/wajm.v23i3.28130.
5. Khalighi AR, Khalighi MR, Behdani R, et al. Evaluating the efficacy of probiotic treatments in patients with small intestinal bacterial overgrowth (SIBO)- A pilot study. Indian J Med Res. 2014;140(5):604-608.
-Michael McIsaac