INTRODUCTION
Depression is a condition affecting approximately 268 million individuals, worldwide.1 This makes such a condition highly prevalent, and worthy of review. Major depressive disorder (MDD) is characterized by persistent feelings of sadness, often accompanied by a lack of interest/pleasure participating in activities. Many of you reading are likely to know somebody in your circle, be it friends or family members, who have experienced depression. You might have also noticed that individuals with depression often have other comorbidities (having more than one health condition at the same time) like cardiovascular disease or diabetes; this makes matters worse of course.
STANDARD TREATMENT OPTIONS
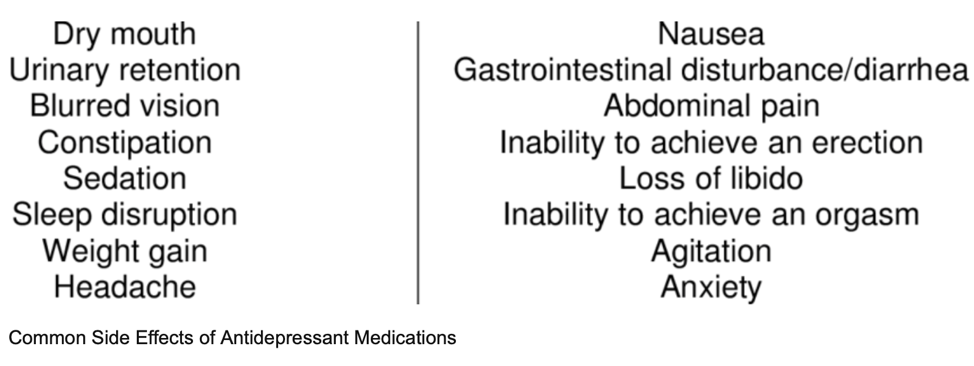
Many individuals with MDD often use some form of medication (i.e., antidepressants) and/or psychological therapy, which can be effective. However, 40% of those individuals respond inadequately to such stand-alone interventions.1(2) Furthermore, recurrence of MDD is rather high often exceeding 60%.1(2) Such interventions can have substantial inadequacies in effectiveness, and high rates of relapse are further complicated by excessive costs and unpleasant side effects (from medications).1(2)

SUPPORTIVE INTEREVTIONS: EXERCISE
Fortunately, there are interventions which support management of depression to include physical activity.2 Exercise has been shown to be effective in treating MDD and reducing comorbidities (mentioned previously).2(1) Surprisingly, recommending exercise as a complementary intervention or stand-alone protocol remains underutilized in clinical settings.2(1) Considering MDD is strongly linked to shorter lifespans and lowered quality of life, it is exceedingly important that individuals are provided with safe and supportive interventions to help liberate them from the shackles of depression.

WHAT THE RESEARCH SAYS
Many studies have explored different exercise interventions and their impacts upon MDD to include (but not limited to) yoga, Pilates, step aerobics, jumping rope, jogging, swimming, bicycling, free weight training, and stretching.3 As one can see, it could be difficult to make a general recommendation as to which protocol might be the most effective. However, Xie et al3(2) did note that aerobic exercise was the most studied/selected intervention.
Intensity (difficulty) of exercise is also relevant and can be measured several ways such as metabolic equivalent (the amount of oxygen consumed while sitting at rest and is equal to 3.5 ml O2 per kg body weight x min), VO2 Max (the maximum amount of oxygen used in exercise), maximum power output, Borg Scale (you rate your perceived exertion along a scale), and calories burned per kilogram of bodyweight per week.3(3) Generally, the systematic review of Xie et al3(3) suggested that most individuals preferred aerobic exercise (stated previously) with moderate intensity at 3-5 days per week.
Summary:
Aerobic exercise
Moderate intensity (50-70% maximum heart rate)
3-5 days per week

DIGGING A LITTLE DEEPER
Although most of individuals reading this article are likely aware that people “feel better” when exercising, less is known as to “why” depressed individuals experience decreased symptoms when engaging in physical activity. The following will explore possible mechanisms behind the effectiveness of exercise against MDD to help uncover why and how exercise matters to mental health.
EXERCISE AND PSYCHOLOGICAL FACTORS
Exercise has the ability to enhance self-worth (i.e., the sense of one’s own value) in addition to supporting self-confidence, life satisfaction, and sleep quality when combined with therapy.3(6) Physical activity was also found to improve self-perception (i.e., the self-judgements and views we have of our physical, mental, and social characteristics), and self-efficacy (i.e., the degree of belief in our ability to take action to reach goals).3(6) Physical activity also upregulates the production of dopamine (increases feeling of pleasure and motivation), 5- hydroxytryptamine (a precursor to serotonin; a molecule that regulates mood and sleep), and noradrenaline (helps manage attention and focus).3(7)

EXERCISE AND INFLAMMATION
Neuroinflammation has been a well-documented phenomenon that is involved in the pathogenesis (development of a disease) of MDD.3(6) Inflammation within the brain can emanate from viral infection, mental stress, metabolic disorders, and inflammation from other organs.4 These pathological conditions can activate immune cells of the brain (i.e., microglia), which release chemical messengers (i.e., interleukin-19, interleukin-1B, interleukin-6, tumor necrosis factor-alpha) that drive neuroinflammation and depression/anxiety.3(6)
Exercise, such as moderately intense aerobic activity (40 minutes x 4 sessions/week), over a 16- week period helped increase the production of anti-inflammatory cytokines (chemical messengers, which reduce inflammation) and reduction of inflammatory markers like C-reactive protein and interleukin-6 (IL-6) amongst individuals with MDD.3(6) Other studies noted by Xie et al3(6) which involved moderately intense aerobic activity combined with high intensity strength training (45 minutes x 2 sessions/week) also indicated reduced IL-6 and depressive symptoms. Such outcomes suggest that aerobic activity (and possibly strength training) helps reduce inflammatory markers and depression-related symptoms.
EXERCISE AND OXIDATIVE STRESS
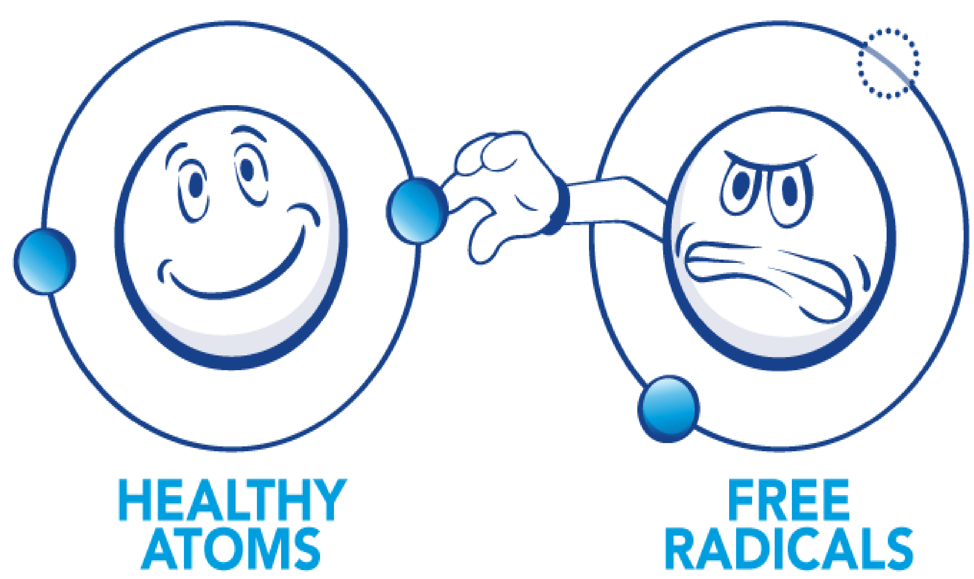
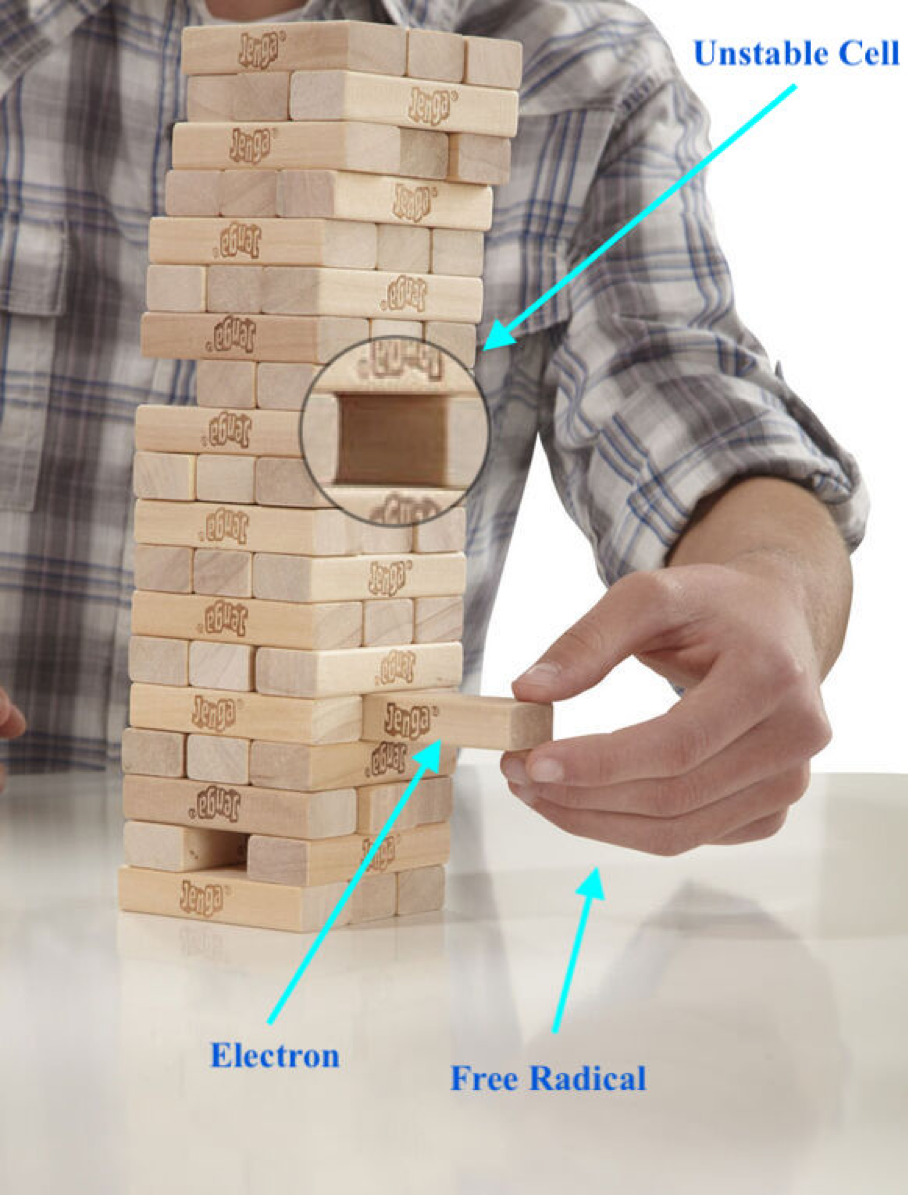
There are molecules in the body, which can damage cell membranes, tissues, and organs by “pulling” electrons away that make cells unstable (remember the game Jenga? Same thing) .5 Such molecules are known as free radicals (FRs…see link below). FRs are generated by normal processes in the body such as energy production (from mitochondria…see link below) as well as from pathophysiological states (i.e., chronic disease) and environmental conditions (i.e., smoke, air pollution). Left unchecked, FRs have the capacity to induce severe damage from the level of DNA to the individual as a whole, including the development of depression.3(6) Such a process is known as oxidative stress (OS).
LINK: ANTIOXIDANTS AND TRACKING OXIDATIVE STRESS
LINK: MITOCHONDRIA AND RELATIONSHIPS TO HEALTH
Although OS is a destructive process, moderate aerobic exercise has been shown to help reduce its affects, in addition to controlling inflammation (mentioned previously).3(6) Aerobic exercise exerts its effects upon OS by helping the body maintain antioxidant (i.e., glutathione; the “master” antioxidant) levels. Such is achieved through expression (produce) of glutathione reductase (helps produce the “active” form of glutathione), glutathione peroxidase (an enzyme that manages the presence and damage from hydrogen peroxide; a molecule that damages cells), as well as helping reduce inflammatory markers such as IL-6, homocysteine, and tumor necrosis factor-alpha.3(6) To learn more about glutathione (considered the master antioxidant) and glutathione peroxidase, please see the link below.
LINK: SELENIUM AND GLUTATHIONE PEROXIDASE: BATTLING REACTIVE OXYGEN SPECIES
CONCLUSIONS
Depression is a condition affecting approximately 268 million individuals, worldwide. Medications and psychotherapy can sometimes lack complete efficacy in treating MDD. However, research has suggested that moderate aerobic exercise throughout the week does have significant effects upon managing depressive symptoms. Therefore, it is possible that physical activity can be used as a complementary, or replacement, protocol to standard approaches while also addressing comorbidities associated with MDD.
References
1. Schmitter M, Spijker J, Smit F, et al. Exercise enhances: Study protocol of a randomized controlled trial on aerobic exercise as depression treatment augmentation. BMC Psychiatry. 2020;20(1):1-11. doi:https://doi.org/10.1186/s12888-020-02989-z.
2. Murri MB, Ekkekakis P, Magagoli M, et al. Physical exercise in major depression: Reducing the mortality gap while improving clinical outcomes. Front Psychiatry. 2018;9(762):1-10. doi: 10.3389/fpsyt.2018.00762.
3. Xie Y, Wu Z, Sun L, et al. The effects and mechanisms of exercise on the treatment of depression. Front Psychiatry. 2021;12(70559):1-16. doi:10.3389/fpsyt.2021.705559.
4. Sun Y, Koyama Y, Shimada S. Organs to the brain: How does systemic inflammation cause neuroinflammation? Front Aging Neurosci. 2022;14:1-10. doi:10.3389/fnagi.2022.903455.
5. Chen GL, Chen SG, Chen F, et al. Nutraceutical potential and antioxidant benefits of selected fruit seeds subjected to an in vitro digestion. J Funct Foods. doi:10.1016/j.jff.2015.11.003.
-Michael McIsaac

