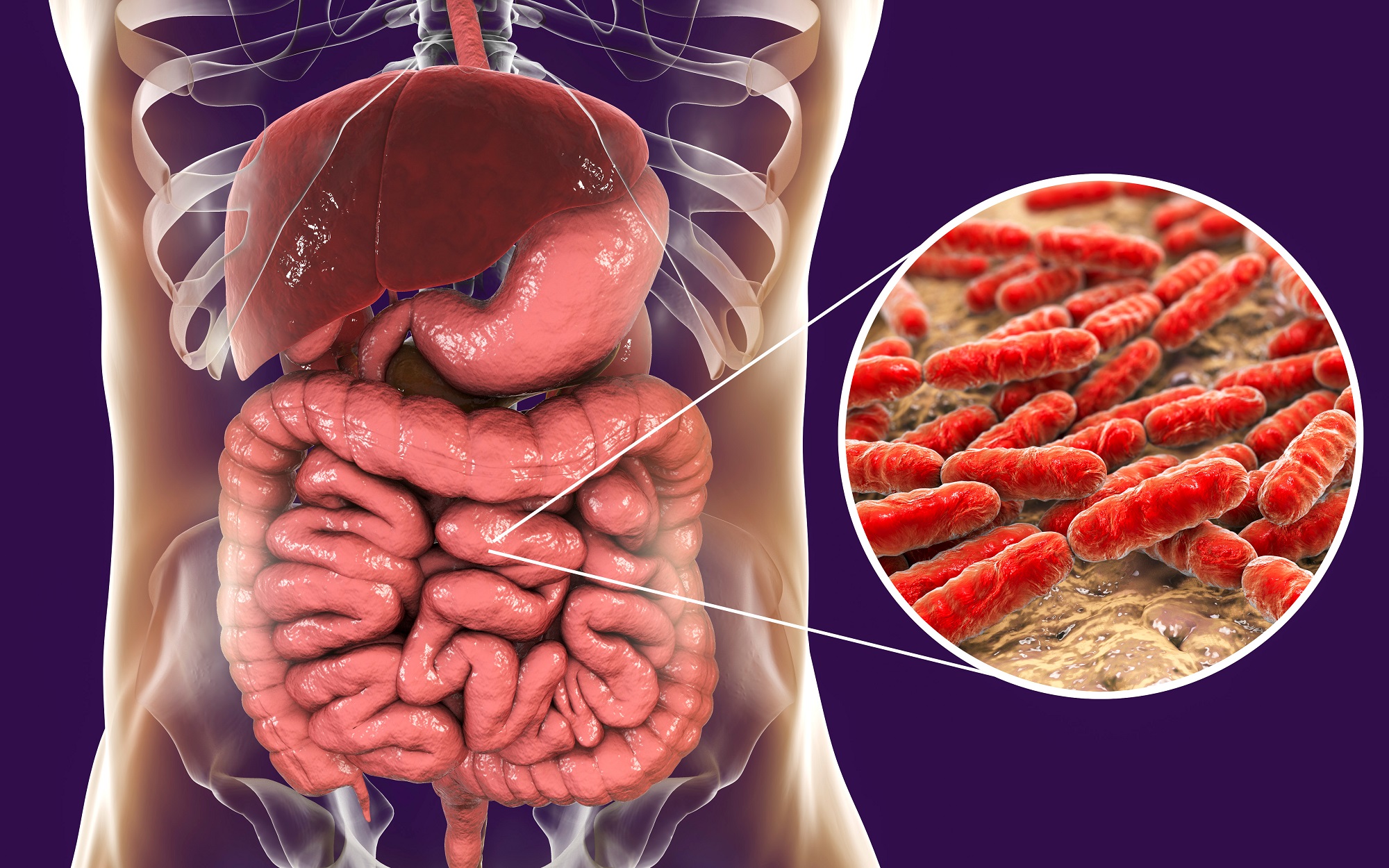
Small intestinal bacterial overgrowth (SIBO) is characterized by an overpopulation (in excess of 105– 106) of bacteria in the small intestine and stomach (Khalighi et al., 2014; Nabanan & Fauzi, 2015). Several urinary organic acid biomarkers are available which help determine the presence and overpopulation of such bacterial species. Such knowledge is critical as it aids in determining appropriate nutritional and medical interventions. As a means of appreciating SIBO and its detection/management, the following will explore the same.
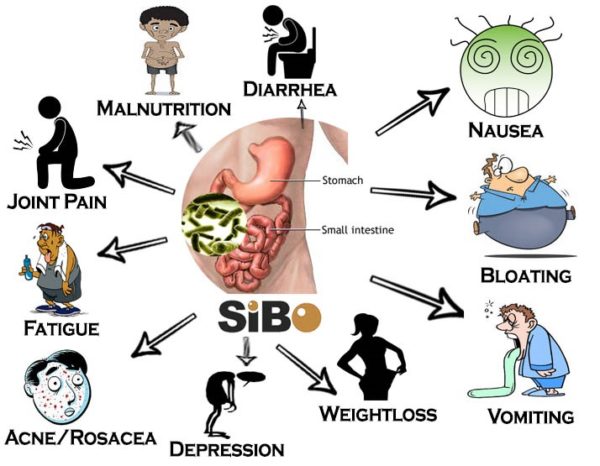
SIBO has several clinical presentations to include nutrient malabsorption, weight loss, severe diarrhea, osteoporosis, and neuropathy (Nabanan & Fauzi, 2015). Such symptoms are thought to derive from excessive aerobic and anaerobic bacterial overgrowth with particularly high concentrations within the small intestine. Bacterial populations also inhabit the colon to include Escherichia coli, Enterococcus spp, klebsiella pneumonia, and Proteus mirabils(Nabanan & Fauzi, 2015). Researchers such as Nabanan and Fauzi (2015) hypothesized that said species migrate towards the small intestine eventually manifesting as SIBO. The following will consider two risk factors which contribute to said condition.
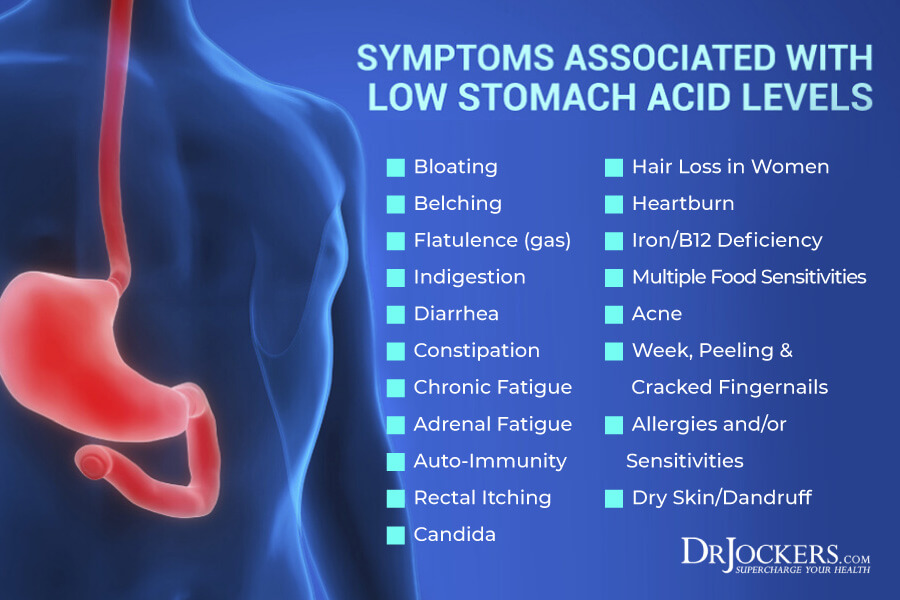
The likelihood of developing SIBO is increased when there is a presence of one, or both, pathophysiological conditions: low stomach acid (i.e., high pH) and poor small intestinal motility (Nabanan & Fauzi, 2015). Gastric acid (when at normal concentrations) tends to suppress bacterial growth along the small intestinal region. Hypochlorhydria (low stomach acid) can occur as a result of aging, using acid reflux/proton pump inhibitors, as well as from helicobacter pyloricolonization (Nabanan & Fauzi, 2015). Compromised gut motility also increases risk of SIBO and is a consequence of uncontrolled diabetes, connective tissue disorders, viral infections, and ischemia. Despite the cause of reduced motility, researchers stated that existing bacterial colonies are unable to pass along to the large intestine for timely excretion, thereby increasing concentrations within the small intestine (Nabanan & Fauzi, 2015).

Several methods exist to determine the presence of SIBO to include direct tests (acquiring a culture of intestinal contents) as well as indirect analysis through organic acid tests (OAT) (Nabanan & Fauzi, 2015; Lord & Bralley, 2012). OAT has particular advantages due to its ease of use (collection of urine) and non-invasive nature when compared to direct testing protocols. Several OAT exist to evaluate SIBO. Such tests include benzoate, hippurate, phenylacetate, phenylpropionate, p-Cresol, p-hydroxyphenylacetate, tricarballyate, D-lactate, and 3,4 dihydroxyphenylpropionate urinary markers (Lord & Bralley, 2012). Upon determining the presence of SIBO (and which bacterial species is unusually dominant), several approaches have been implemented to manage the condition and its complications (i.e., nutrient malabsorption etc). The following will consider such approaches.
Nabanan and Fauzi (2015) noted that despite cause of SIBO, three approaches are always considered: treating underlying disease, eradicating bacterial overgrowth, and resolving nutritional deficiencies that arose from SIBO. If reduced motility (the underlying problem) is an issue, for example, implementation of magnesium citrate, increasing fiber, and improving hydration can be effective strategies to improve gastric and small intestinal emptying (Dupont, Constant, Imbert, Hebert, Zourabichvili, & Kapel, 2019). Managing the overgrowth of species is also relevant since their presence can continue to induce systemic issues (i.e., malabsorption, inflammation).

Depending on the type of bacteria that is dominant, there are particular antibiotics that can be used to include Rifaximin, Amoxicillin/Clavulanate, Metronidazol + trimetophrim/sulfamethoxazole, and Metronidazole + Cephalexin (Nabanan & Fauzi, 2015). Managing nutrient levels is also critical as deficiencies in vitamin B12, A, D, E, and K can occur with SIBO due to poor stomach acid and fat malabsorption (Nabanan & Fauzi, 2015). In addition to monitoring levels of said micronutrients, Lord and Bralley (2012) also noted that glutamine (10-20 mg/day), digestive aids (betaine, enzymes, bile), and free form amino acids are also useful for aiding in digestion and improving absorption. If particular micronutrients remain low, supplementation/increasing food intake may be warranted as an adjunct intervention.
In conclusion, SIBO can induce pathophysiological conditions to include nutrient malabsorption, weight loss, severe diarrhea, osteoporosis, and neuropathy (Nabanan & Fauzi, 2015). Such symptoms derive from excessive aerobic and anaerobic bacterial overgrowth within the stomach and small intestine. If SIBO is suspected, additional organic testing can help delineate which species are likely to be overpopulated while facilitating protocol choice and tracking outcomes in a way that is non-invasive.
References
Dupont, C., Constant, F., Imbert, A., Hebert, G., Zourabichvili, O., & Kapel, N. (2019). Time to treatment response of a magnesium and sulphate-rich natural mineral water in functional constipation. Nutrition, 65, 167-172.
Khalighi, A. R., Khalighi, M. R., Behdani, R., Jamali, J., Khosravi, A., Kouhestani, S., … Khalighi, N. (2014). Evaluating the efficacy of probiotic treatments in patients with small intestinal bacterial overgrowth (SIBO) – A pilot study. Indian Journal of Medical Research, 140(5), 604-608.
Lord, R. S., & Bralley, J. A. (2012). Laboratory evaluations for integrative and functional medicine (2nded.). Duluth, GA: Genova Diagnostics.
Nabanan, T., & Fauzi, A. (2015). Diagnosis and treatment of small intestinal bacterial overgrowth. The Indonesian Journal of Gastroenterology, Hepatology and Digestive Endoscopy, 16(2), 105-111.
-Michael McIsaac
