Optimal vitamin D levels, as measured by 25-hydroxyvitamin D, remains to be somewhat equivocal, thereby affecting recommended oral doses of vitamin D3. Since research indicates the critical relationship of vitamin D to optimal health, it behooves one to consider the nuances and implications of recommending supplemental vitamin D to individuals. The following will explore the same.
Gaby (2008) noted that evidence has suggested a relationship of vitamin D3to prevention of cancers (certain types), osteoporosis, improvement of insulin levels/mood, possible prevention of multiple sclerosis, in addition to mitigation of certain infections. As such, there is a strong interest in uncovering optimal doses of vitamin D3.

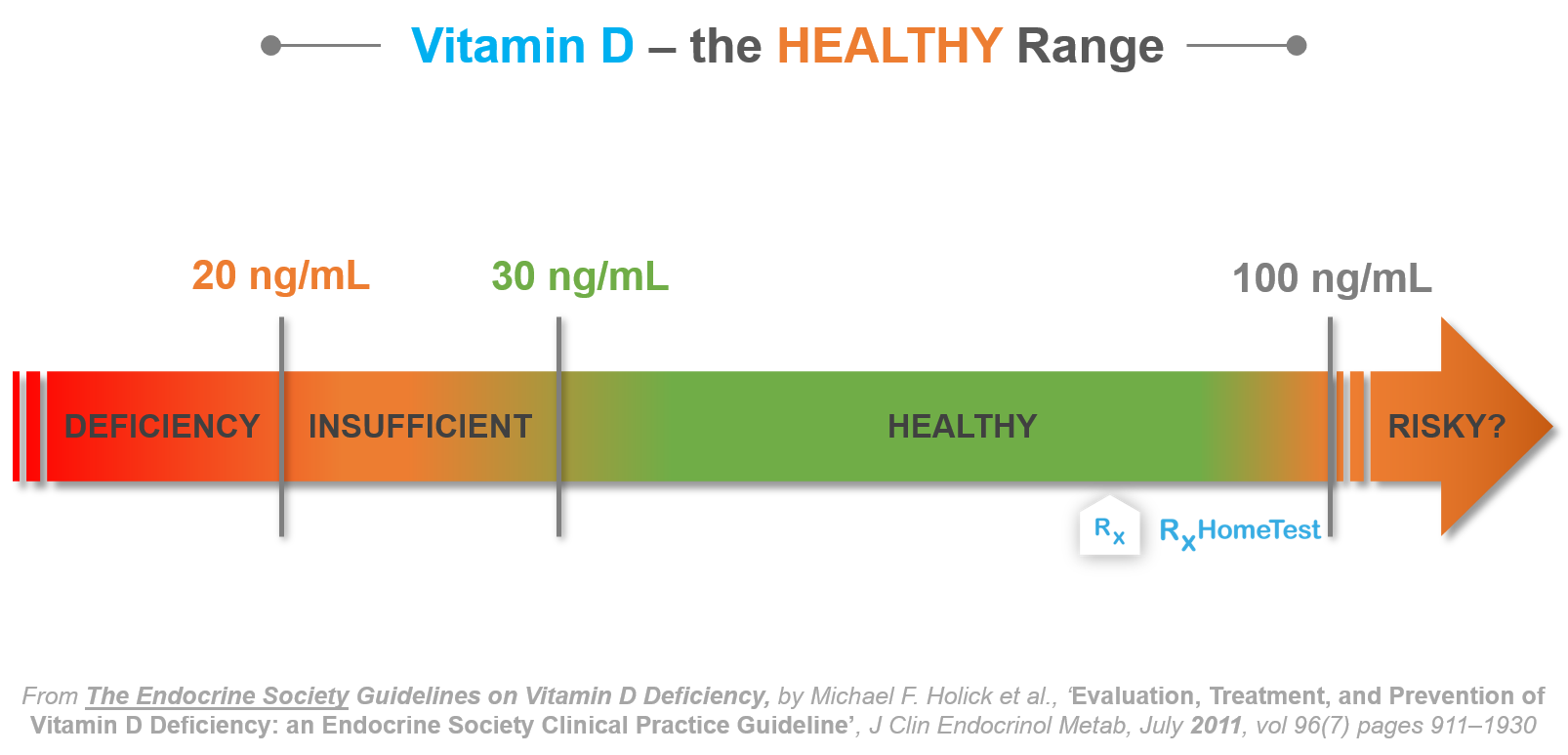
Conventional recommendations of 200-600 IU/day of D3 has been reported as insufficient in prevention of conditions listed in the previous sections (Gaby, 2008). As such, 1000-4000 IU/day of D3is commonly advised by clinicians to reach 40 ng/ml of 25-hydroxyvitamin D; a level considered optimal. However, some researchers feel that 25-hydroxyvitamin D levels of 40 ng/ml or 4000 IU/day of D3is still conservative and inadequate in nature (Gaby, 2008).
Gaby (2008) stated that some researchers have indicated that 10,000 IU/day of D3 is safe without any evidence of hypercalcemia; a cluster of symptoms indicative of vitamin D3 toxicity to include 25-hydroxyvitamin D levels of 80 ng/ml or higher, calcification of tissues (kidneys, heart, lungs), serum calcium levels above 5.7 mg/dL, in addition to symptoms such as headache, nausea, renal dysfunction, and hypertension (Gropper, Smith, & Carr, 2018).
Interestingly, Hathcock, Shao, Vieth, and Heaney (2007) noted that studies monitoring 10,000 IU/day of D3 found no indication of hypercalcemia. However, Gaby (2008) did correctly state that said research did not conduct long-term trials with the aforementioned daily doses of D3; Hathcock et al. (2007) conducted their studies for a 20-week period. Such time frames might not be long enough for calcium levels to be detected in key organs (kidneys, heart, lungs). Gaby (2008) also noted that measurement of serum calcium levels, for hypercalcemia, might not be an representative of toxicity.
Hypercalcemia may not be evident in the presence of super-therapeutic doses of D3; since the body tightly regulates serum calcium levels, it is possible that vitamin D toxicity might still exist in the presence of normal serum calcium levels (Gaby, 2008). Such blood levels are regulated by redirecting excessive calcium towards the kidneys for excretion. However, it is possible that calcium levels may slowly rise after such regulatory mechanisms are overwhelmed. Such a process might occur beyond the 20-week period in the study of Hathcock et al. (2007).
In conclusion, research indicates the need of vitamin D3 in the diet due to its relationship prevention of cancers (certain types), osteoporosis, improvement of insulin levels/mood, possible prevention of multiple sclerosis, in addition to mitigation of certain infections. However, vigilance must be implemented when considering the benefits of D3 against possible consequences of higher doses.
References
Gaby, A. (2008). What is the safe upper limit for vitamin D supplementation? Opposing Views in Context,(300), 104.
Gropper, S. S., Smith, J. L., & Carr, T. P. (2018). Advanced nutrition and human metabolism (7thed.). Boston, MA: Cengage Learning.
Hathcock, J. N., Shao, A, Vieth, R., & Heaney, R. (2007). Risk assessment for vitamin D. American Journal of Clinical Nutrition. 85(1), 6-18.
-Michael McIsaac