INTRODUCTION
Ever heard of diverticulosis or diverticulitis? Maybe you had a friend who had this problem…I did. In fact, over 130,000 hospitalizations per year are attributed to this disease in the USA alone.1 And Canada is estimated to have over 130,000 citizens with diverticular disease, costing over 88 million per year to treat.2
WHAT IS DIVERTICULOSIS AND DIVERTICULITIS?
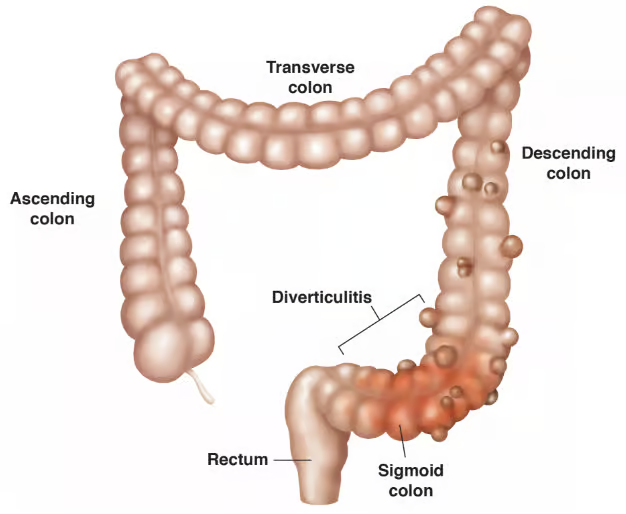
First, we should understand where the problem is on your body. There is a spot in the lower left/bottom portion of your belly, and this is where your descending colon is (a storage tank for stool before you go to the bathroom). At the very bottom is the sigmoid colon…this is where diverticulosis/diverticulitis mostly exists.
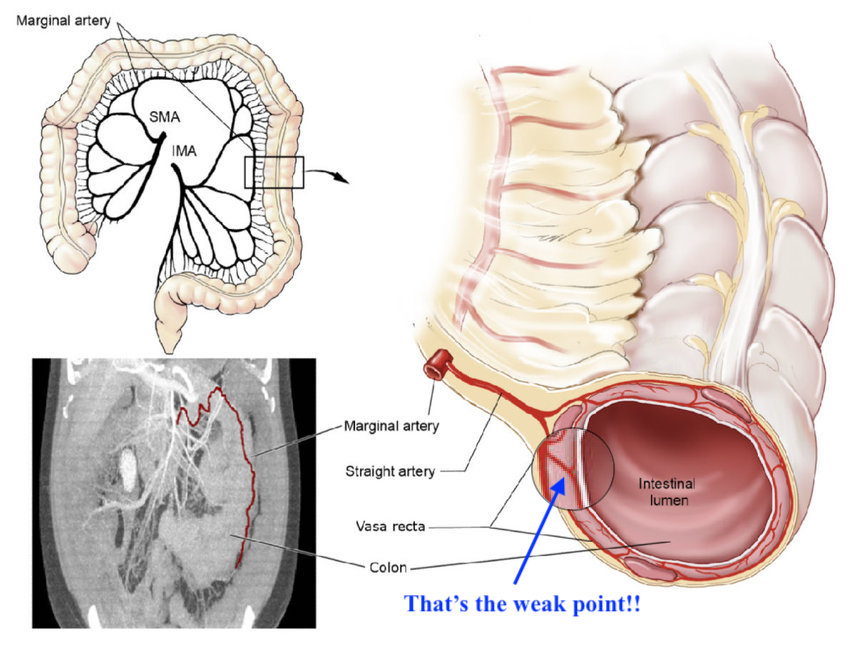
Image: ResearchGate
A DEEPER LOOK AT YOUR SIGMOID COLON
First, let’s talk about those little “bubbles” you saw in the images above. You probably know they don’t look right, and are not normal. Those little bubbles are the problem. Your gut lining is made of multiple layers, like your skin, and those layers need a good blood supply to work right. Little blood vessels (arteries) have to penetrate the lining of your gut in multiple places.1(210) Those places where the artery pierces the gut are a weak point.
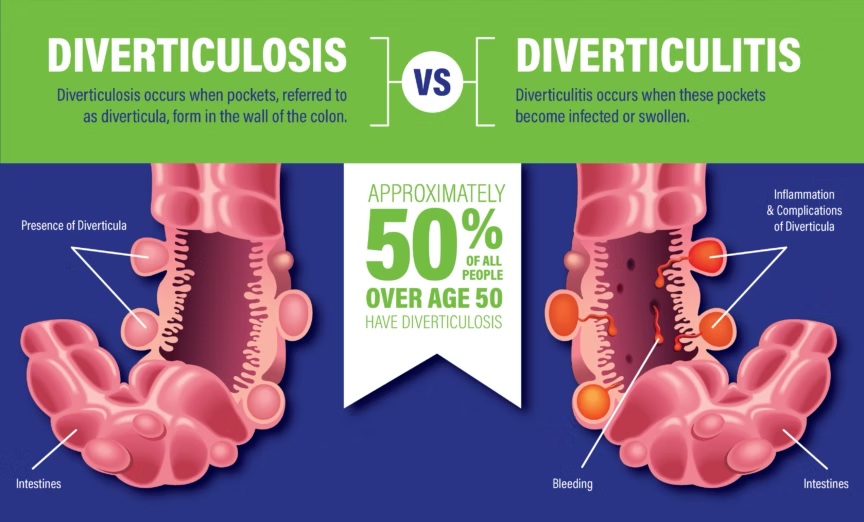
Image: AvantBKG Hospitals
Have you ever packed a garbage bag with so much stuff in it, that a little part of the bag stretched, got a little thin, then bulged? Well, that’s what happens near these weak points of the colon (where little arteries enter). The little bubbles are called diverticula, and they are like having a pile of mini hernias.1(210)
When you have those bubbles/pockets/diverticula (whatever YOU want to call them), but they are not bothering you, it is termed diverticulosis.3 However, when the diverticula become infected, inflamed, and angry, it is called diverticulitis.3 Keep reading.
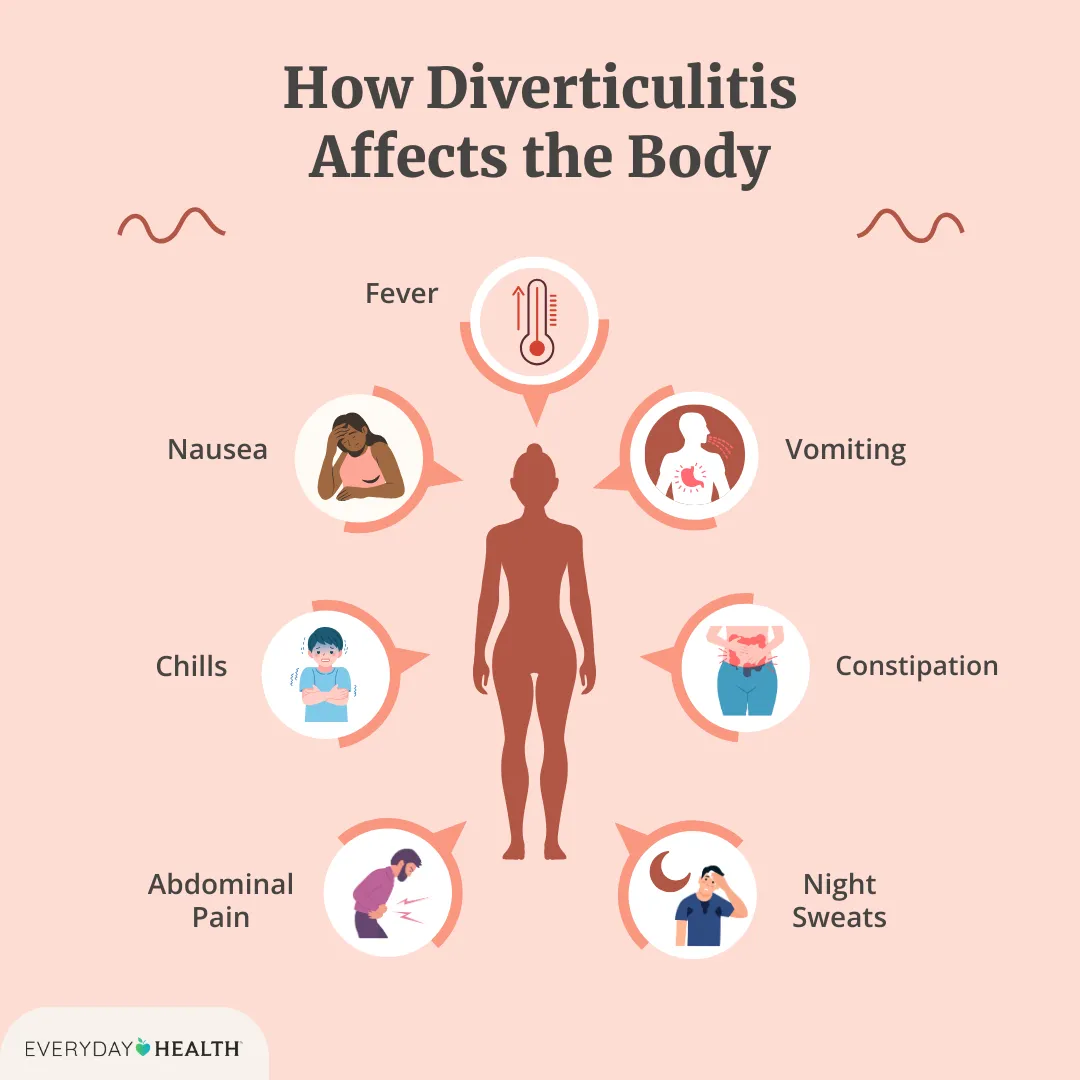
Image: Everyday Health
COOL. WHAT ARE THE SYMPTOMS OF DIVERTICULITIS?
Now, if you have diverticulitis, you will know it! Symptoms can include any combination of:
- Nausea5
- Flatulence5
- Abdominal Pain5
- Vomiting5
- Constipation5
- Diarrhea14
- Fever5
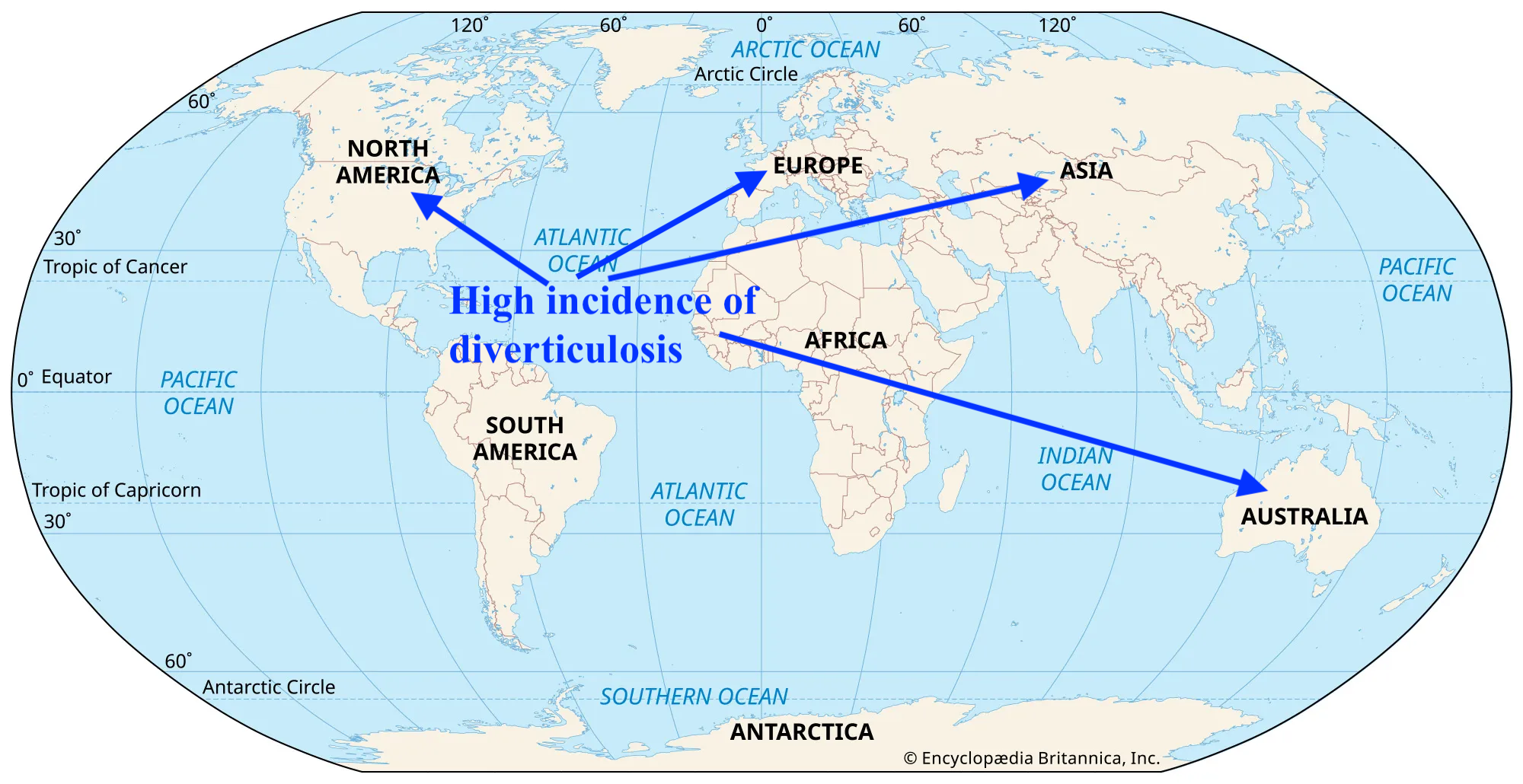
Image: Britannica
IS DIVERTICULOSIS A GLOBAL THING?
I didn’t know this before, but the distribution of diverticulosis actually varies by geographic region, and the location of the condition in the colon changes too!
- In Westernized nations, diverticulosis occurs mostly in the sigmoid colon1(209)
- In Asian regions, diverticulosis mostly occurs in the right side of the colon1(209)
- Prevalence is similar between males and females1(209)
- Risk of diverticulosis increases significantly with age1(209)
- About 20% of individuals with diverticulosis will develop diverticulitis4
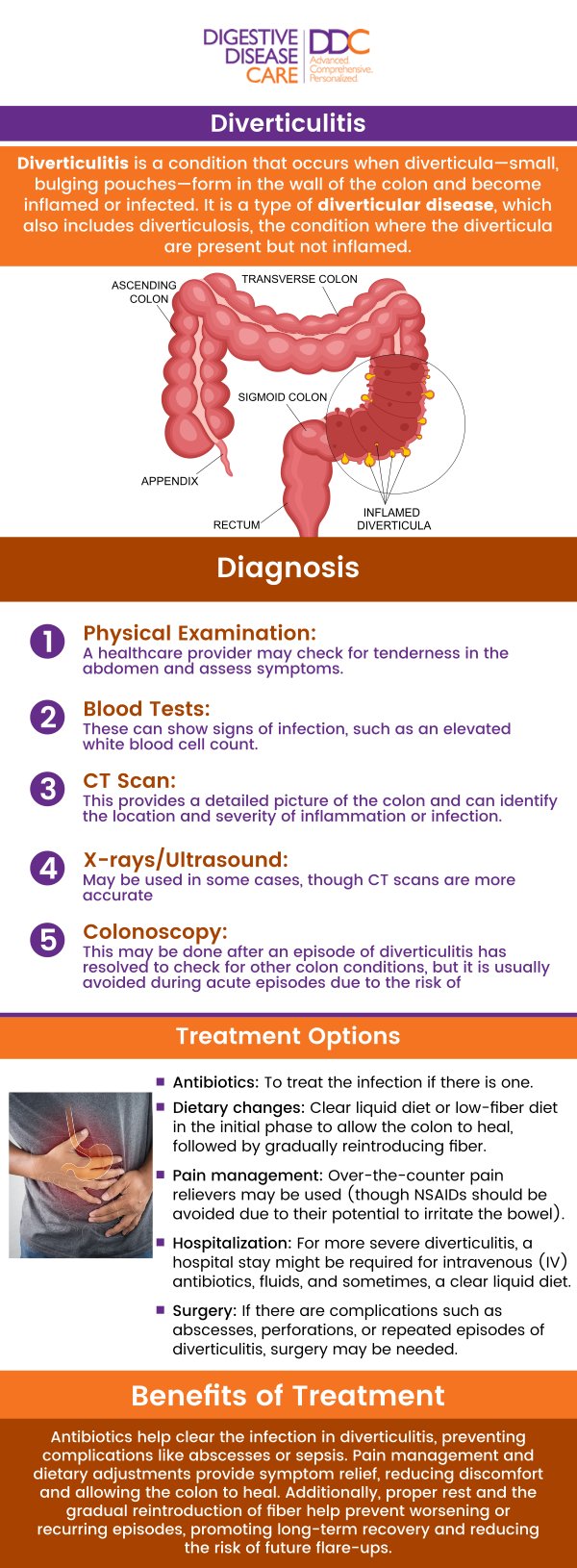
Image: Digestive Disease Care
OK. WHAT ARE THE RISK FACTORS?
There are a couple so get ready. Munie and Nalamati1(210) as well as Strate and Morris12 stated that there are several risk factors associated with diverticulosis:
- Lack of fiber: there are epidemiologic studies that have noted individuals in Westernized regions (higher rate of diverticulosis) tended to eat much less fiber than in regions that ate more fiber (lower incidence of diverticulosis).
- Red meat: again, there is a correlation (does not mean cause) with red meat intake and diverticulosis, and there seems to be a 1.5 to 2.0 times increase in risk.
- Obesity/lack of physical activity: physical activity seems to have a protective effect against the development of diverticulosis, while obesity is associated with both the development of diverticulitis, and bleeding.
- Non-Steroidal Anti-Inflammatory Drugs: i.e., ibuprofen, naproxen, aspirin have been associated with diverticular bleeding, and increased risk of developing diverticulosis.
- Nuts, Corn, Grains, Popcorn: this used to be considered a common risk factor. However, a robust study including over 47,000 subjects between the ages of 40-75 that were tracked between 1986 and 2004 and found an INVERSE relationship between nuts/seeds/popcorn consumption and the development of diverticulosis or increasing the risk of diverticulitis…Food for thought. Literally.
- Low Vitamin D: case–control studies comparing vitamin D levels (they call it 25OHD when testing your blood) and the likelihood of getting diverticulitis, indicated that low vitamin D levels is indeed a risk factor for diverticulitis.
Image: Slideshare.net
A DEEPER DIVE ON DIVERTICULITIS
Tracking the bad changes that happen in your colon, and the causes (or mechanisms if you want to sound fancy) of those changes that make diverticulosis, is known as pathophysiology. It’s a fancy way of describing how and why you get sick. You see, when you understand the little things that are festering away in your body to cause diverticulosis/diverticulitis, you begin to figure out HOW to fix it.
Here is a list of things that are known to cause and drive diverticulitis:
- Low Grade Chronic Inflammation (LGCI): Munie and Nalamati1(211) noted that 75% of individuals assessed for diverticulitis (resected colonic specimens) had the presence of inflammatory cells (neutrophils and lymphocytes). What does this mean in English?LGCI like a heating pad that you turned on to sooth stiff muscles. It is really helpful in the beginning. But imagine this heating pad does not turn off. Suddenly, that helpful heat is now beginning to cause discomfort. More time passes and it is STILL on, and now it’s beginning to hurt. Eventually, that wonderful heat you needed is starting to burn and damage you…things are getting serious. That is the tale of LGCI. Inflammation is a normal, natural, and necessary process where your immune system cells address and resolve that problem (fixing tissue damage, getting rid of a virus, or bacterial infection). BUT, when that process sticks around and outstays its welcome, it’s like that heating pad that you sat on for way too long.
- Abnormal Colonic Motility: in other words, your guts are not moving the freight train (stool) along like they should.1(211) There are a few reasons this happens. Munie and Nalamati1(211) noted that there might be a dysregulation of the enteric nervous system causing intestinal dysmotility; in other words, the wiring and communication to the guts is not working right. Another possible cause is dysregulation of serotonin around the diverticula.1(211) Serotonin is a neuropeptide (a chemical messenger) that “talks” to your colon helping make smooth contractions, intestinal secretions, and move stool along.6 Munie and Nalamati1(211) stated that diseased colons had high local levels of serotonin/serotonin producing cells (enterochromaffin cells). Generally, serotonin is made, used, and then removed from the area using little conveyor belts known as serotonin transporters (SERTs). It looks like these SERTS are not very high in numbers (i.e., not being expressed in nerd talk) in those with diverticulitis.7 This leads to a back-up of serotonin.
- High Colon Pressure: this one seems a little more intuitive. The colon, especially the sigmoid colon, is smaller in diameter compared to other parts of the colon. When you are blocked up/constipated, there is a lot of pressure pushing against the walls of your colon. Remember the garbage bag analogy previously? It is thought that this pressure drives the formation of diverticula.1(211)
Image: Healthy MEPA
HOW DO I SUPPORT HEALING MY DIGESTIVE SYSTEM?
The number one step to take if you suspect you have diverticulitis: go your family doctor, because diverticulitis is potentially harmful. There are different types of diverticulitis. One type is called uncomplicated (i.e., angry, inflamed, infected diverticula), and the other one is complicated (angry, inflamed, infected, and spreading beyond the diverticula- not good).8
When you have sought medical attention, and complicated diverticulitis has been ruled out (hopefully), you can start taking small steps to address different drivers of diverticulitis, and begin your healing process.
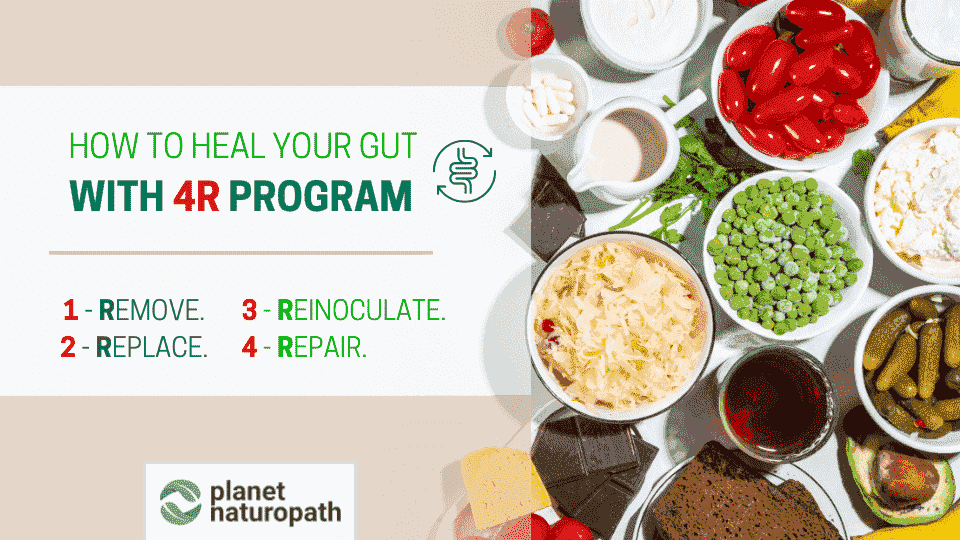
Image: Planet Naturopath
THE FOUR R PROGRAM
When your digestive system is not working right, you need an approach that calms things down and allows your colon to heal. If you don’t, your colon will be in a continuous state of inflammation… like having a scab on your arm that you are constantly picking at; it is impossible to heal well. We will use four helpful steps (Remove, Reintroduce, Re-inoculate, Repair) that gently reduces inflammation, while healing the gut and improving motility (moving your stool along/keeping you regular).9 See below:

Image: CBC
- REMOVE: this is a very sensible first step. Imagine if you had a towel thrown on your red-hot kitchen stove element…there is a clear risk of a fire and damage there (inflammation). You intuitively know that removing the towel is by far the best first step. When you have diverticulitis, you have to get rid of foods that bind you up and cause fires (inflammation). You also want to cut down on NSAIDS and smoking (speak to your family doctor).
Constipation, as you know, is implicated in diverticulitis. Processed foods are low in fiber, and high in omega-6 fats (drive inflammation).This is a combination that you don’t want. Here are a few articles that I wrote on the health problems related to processed foods:
ARTICLE LINK: Processed Food: Definition and Health Consequences
ARTICLE LINK: Processed Foods, Cardiovascular Disease, and Insulin Resistance
ARTICLE LINK: Processed Food, Poor Sleep, and Low-Grade Chronic Inflammation

Image: The Seasoned Mom
- REINTRODUCE: asking you to remove processed food makes sense, but you still need to eat! You may require particular foods during your flare-up (diverticulitis), and other foods when it has calmed down (diverticulosis).
During a flare-up (up to the first 7 days), your colon is going to be very sensitive and inflamed.10 You also might think your colon does not want to deal with hard-to-digest foods, and would prefer easily digestible/liquid-like food, for a little bit at least. Interestingly, a systematic review scoured past research implementing liquid diets and liberalised (therapeutic diet with less restrictions) diets; there found no meaningful difference (how quickly patients recovered) between them.11
However, the studies were low quality (individual studies were hard to compare to each other), which means we should also be cautious about drawing strong conclusions.11(12) Currently, official recommendations suggest liquid diets during the first 3-5 days, especially because patients report greater comfort.12
What makes up a liquid diet you ask? Well, flare-ups can cause vomiting and diarrhea; this can cause a big loss of water (and electrolytes). You can go a while without protein/carbs/fats, but cannot get by too long without water and electrolytes. So, the most important step during a flare-up is to get fluids, AND it is easy to digest.
ARTICLE LINK: Mild Chronic Dehydration and Implications
ARTICLE LINK: Neuromuscular Dysregulation and Electrolyte Deficiencies
ARTICLE LINK: Antioxidants and Tracking Antioxidant StressConsider beef/chicken/vegetable broths with salt, and herbal teas for the first few days.15 Feel free to have squeezed fruit (without pulp) juice as well.15 After you notice your pain and discomfort decreasing (up to a week), then you can consider getting in other foods. When a few days have passed, slowly start introducing fiber-rich foods.15
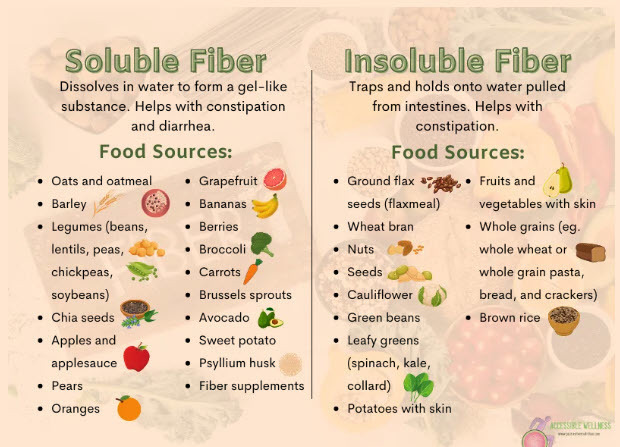
Image: My Chiro Med
Your goal is to slowly increase your fiber up to about 30 grams or more a day.16 You can certainly spread this over a typical 3-meal-per-day frequency as well. And it’s not really difficult to figure out how much fiber is in a food either. Grab your smartphone and Google!
ARTICLE LINK: Constipation and Benefits of Fiber
Interestingly, it seems that insoluble fiber has stronger effects on minimizing future episodes of diverticulitis.17 Wegermann, Kara et al17(1) cited a prospective, observational cohort study of over 50,000 subjects that were tracked from 1990-2014. They found that the higher the insoluble fiber intake, the lower the rate of diverticulitis among participants.
Insoluble fiber might be helpful for preventing diverticulitis because it absorbs water.18 This helps form stool and quickly move it past the sigmoid colon; it helps reduce chances of constipation.17
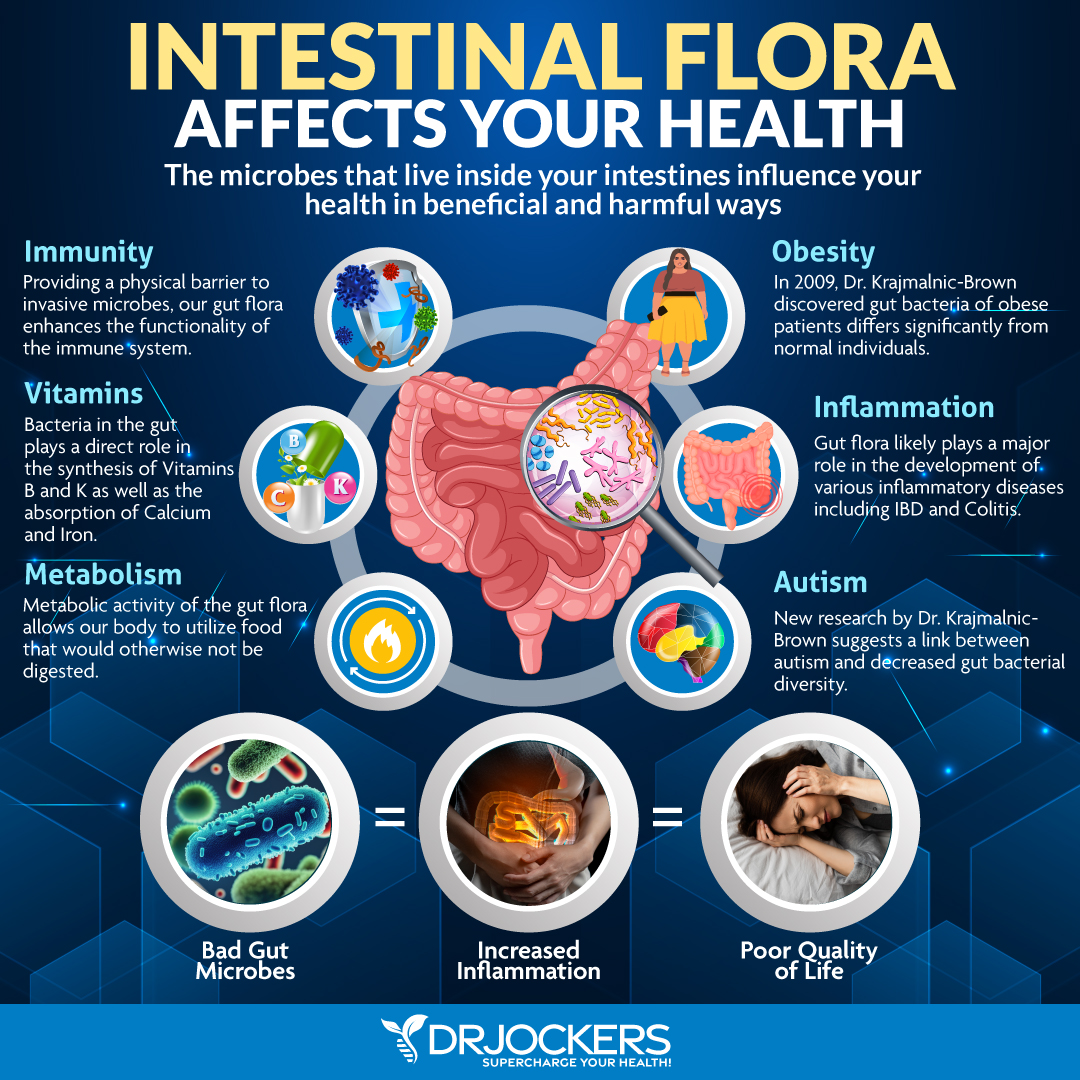
Image: Dr. Jockers
- REINNOCULATE:
Increasing your fiber intake to help motor your digestion/bowel movements along is a great step. But, you might not have been aware that there is a jungle of bacteria in your digestive tract that also plays a CRITICAL role in maintaining your digestive health. Did you know there are bacteria involved in helping your immune system avoid allergic reactions, while also helping defend against real pathogens?19 That’s just one example.
There are other “good” bacteria that help reduce and control inflammation, improve gut motility, and reduce inflammation markers (for the nerds: C-reactive protein, Interleukin-6, tumor necrosis factor alpha).19(3) These include Lactobacillus, Bifidobacterium adolescentis, Phascolarctobacterium, Akkermansia muciniphila, and they are present in well-working gut, but very low among individuals with diverticulitis19(3) Furthermore, the presence of Enterobacteriaceae, Streptococcus and Bacteroides are all higher in the digestive tracts of individuals with diverticulitis.19(10)
The point is, when you have a good balance of bacteria in your digestive tract, it helps keep your gut lining strong and protected, while allowing the right things in (i.e., nutrients), keeping the wrong things out (pathogens, large chunks of food), moving stool along, and keeping your immune system in tip-top shape.
The problem is, Western diets are implicated in messing your intestinal/bacterial ecosystem up. Processed foods create imbalances in the beneficial bacteria and harmful bacteria/viruses/fungus in your guts. This imbalance is known as dysbiosis, and it’s not good for you long-term.19(3)
Here are some articles I wrote on dysbiosis, and the not-so-good effects on the body:
ARTICLE LINK: Hypochlorhydria and Dysbiosis
ARTICLE LINK: Constipation, 5-HT, and Dysbiosis
ARTICLE LINK: Leaky Gut and Probiotics: Exploring the Connection
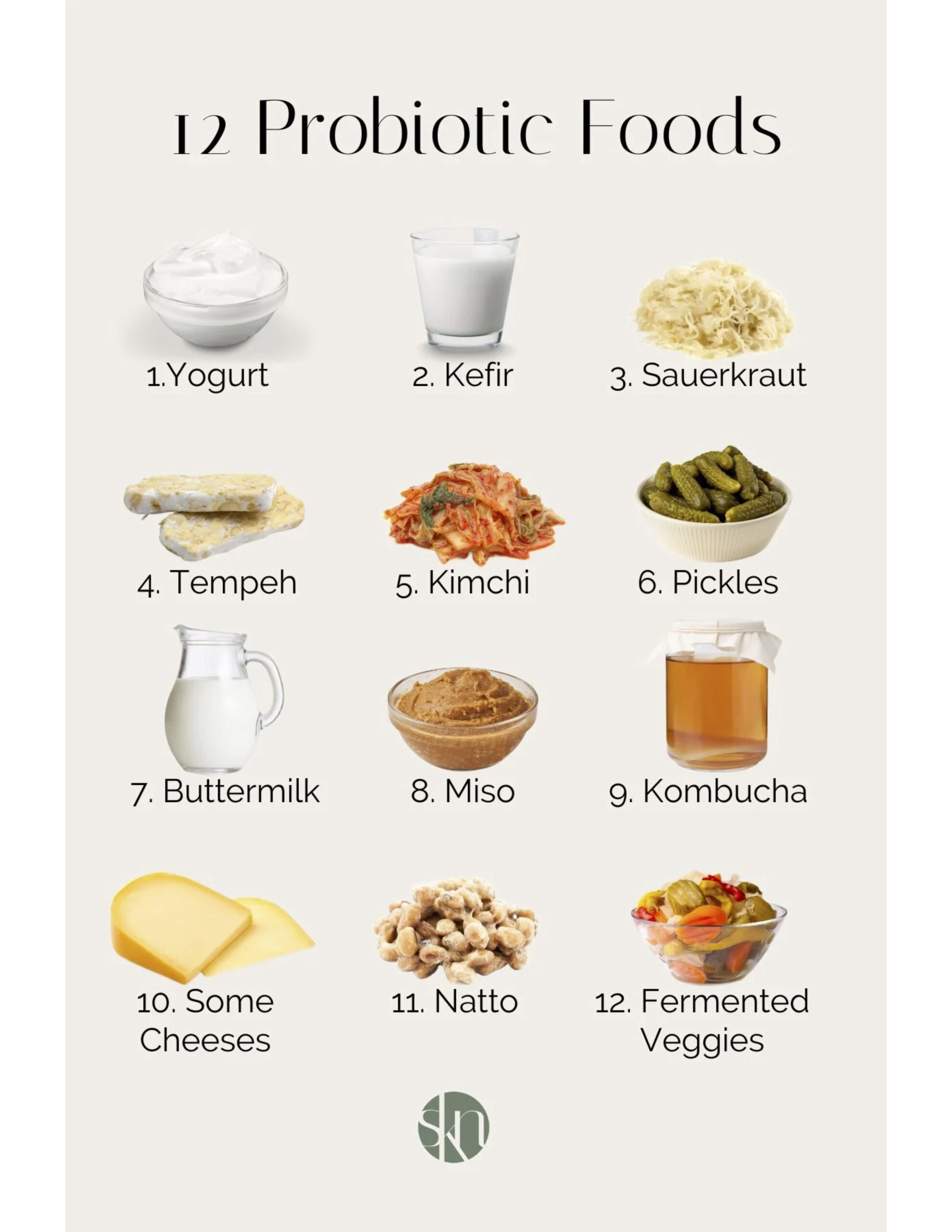
Image: Kay Nutrition
So, introducing foods that are rich in helpful bacteria (aka probiotics-Lactobacillus, Bifidobacterium) every day is another well-advised step (see image above) and has been shown to help control inflammation, bloating, and abdominal pain.19(4) Just remember, it might be best to add these after your guts have calmed down a little from a flare-up (up to 7 days).
In addition to food, you can also consider a probiotic supplement that is rich in Lactobacillus/Bifidobacterium for a 8-12 weeks as well, to help jump start your gut back into shape a little faster. But I would make a food-first approach your priority long-term.
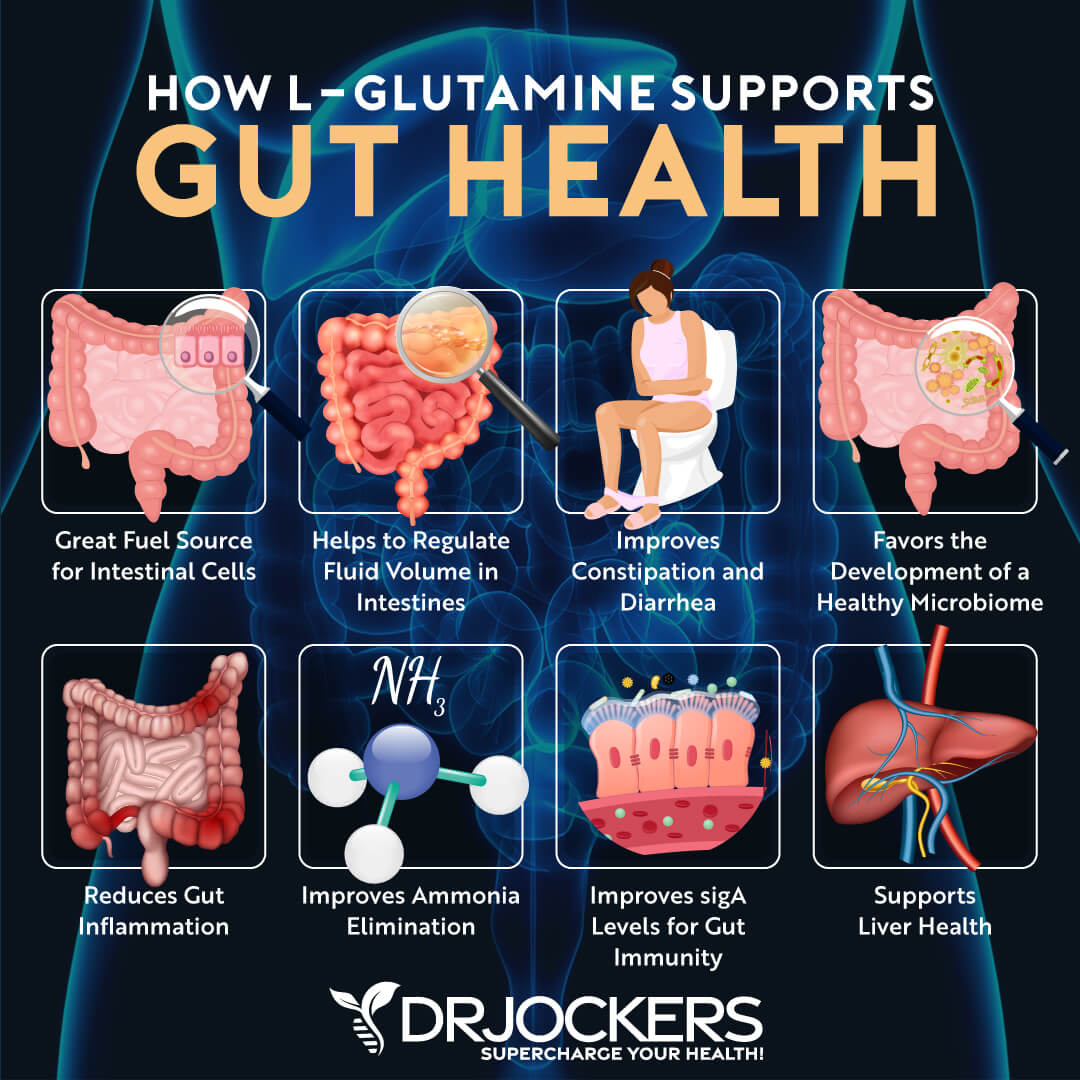
Image: Dr. Jockers
- REPAIR
The is the final phase of your gut restoration journey! So far you have learned about what to avoid eating, what to start eating, the value of probiotic-rich foods, and the targeted use of probiotic supplementation. This last phase is called the repair phase, and as you now know, diverticulitis gives your guts a good beating. This means your intestinal cells are damaged and inflamed. This also means that your intestinal cells (enterocytes) need to be fixed/replaced.
Now, your body replaces gut cells every 4-5 days regardless (pretty impressive), but you can imagine this is a much more intensive process when you have a flare-up.20 The problem is, diverticulitis not only involves damaged cells; it also involves those cells losing their connection with each other.21 Your gut cells are pretty much stacked against one another, forming a strong wall/barrier. When these cells are working right, they “permit” good things from your food into your blood, while keeping the “bad” things out (pathogens, large chunks of food).20(15)
Well, diverticulitis messes with this wall of gut cells, and this is a bad thing known as leaky gut, or increased intestinal permeability (fancy speak).21(1) Have a look at my article below where I covered leaky gut in greater detail.
ARTICLE LINK: Leaky Gut and Antibiotics: Exploring the Connection
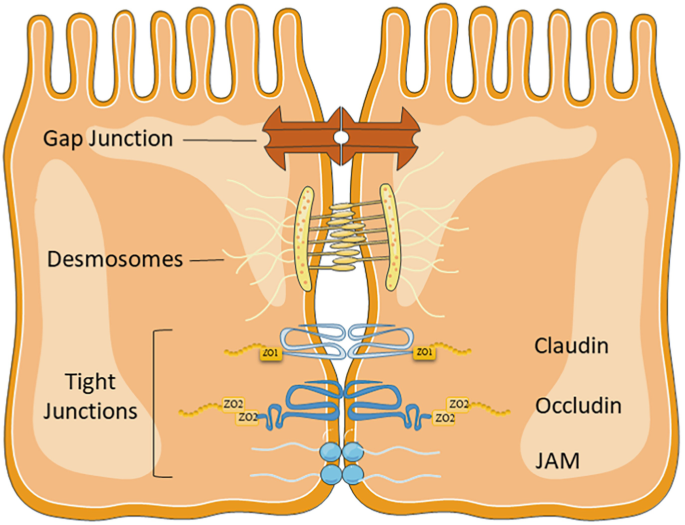
Image: Springer
The good news is there are ways to help heal and restore the connection between your cells, technically known as tight junctions.22 These connections between your gut cells are made of various types of proteins (i.e., occludins, claudins, junctional adhesion molecules, tricellulin) and they are critical to maintaining optimal barrier function.20(2),22(115)
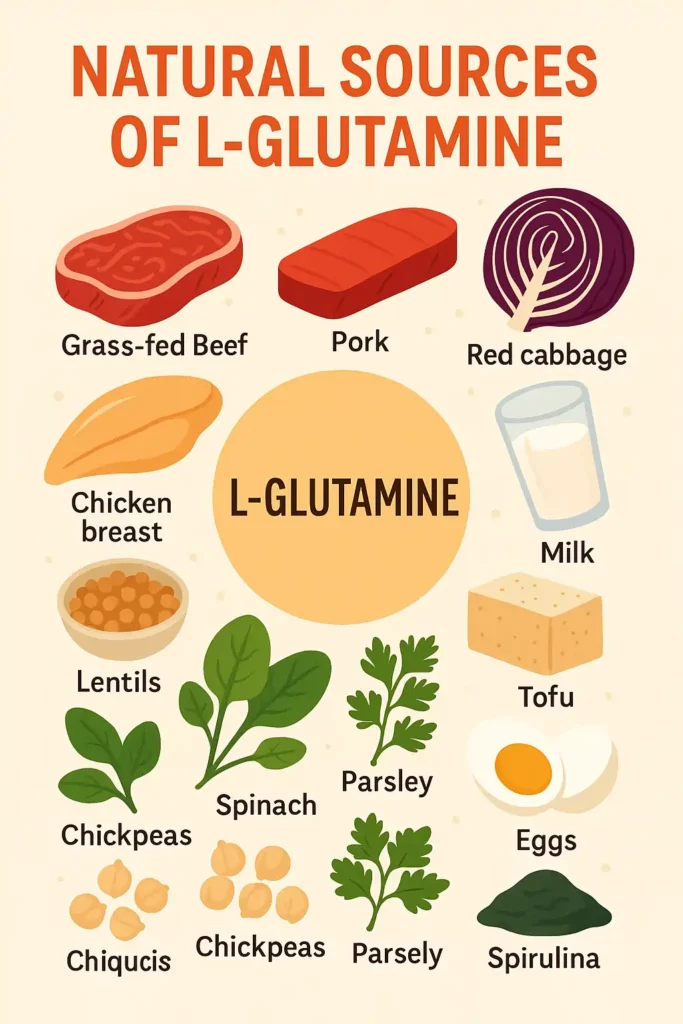
Image: Alternative Health
During normal wear and tear, your enterocytes use a particular amino acid to heal, repair, and replace themselves with fresh cells. This amino acid is known as glutamine, and it is particularly abundant in beef, pork, poultry and dairy products, as well as nuts, cabbage, tofu, and vegetables.23 Be sure to do a deeper dive on glutamine and leaky gut in my articles below to appreciate glutamine just a little more.
ARTICLE LINK: Intestinal Permeability: Support With Glutamine
ARTICLE LINK: Irritable Bowel Syndrome: Supporting Intestinal Barrier Function with Glutamine
Glutamine is critical to promote enterocyte proliferation (making more cells), maintain tight junctions, supress inflammatory processes, and protect cells from killing themselves (aka apoptosis) unnecessarily.20(1) So you need to make sure you are getting these foods in each day, and I would suggest getting glutamine-rich foods at each meal as well.
Image: Well.ca
Foods with glutamine is foundational. However, just as I suggested supplementation with probiotics to support foods rich in beneficial bacteria, I would also suggest supplemental glutamine for the first couple of months as well (to help accelerate healing). 15-30 grams a day of supplemental glutamine has been shown to help reduce inflammation, manage dysbiosis, and improve tight junction integrity.24(152)

Image: Owlcation
THAT WAS A TON OF INFO. GIVE ME A SUMMARY!
Yes, that was a LOT of information. Let’s break it down:
- Remove processed foods and alcohol from your diet. If you smoke and/or use NSAIDS, think hard about quitting, and speak with your family doctor first.
- Reintroduce salt, liquids, herbal teas, bone broths, and squeezed fruit juices (pulp removed) during the first 7 days of a flareup.
- After the first week of a flare-up, gently introduce solid foods rich in fiber at each meal, especially insoluble fiber (while staying well hydrated).
- After the first week of a flare-up, also begin adding foods rich in beneficial bacteria, and supplement with probiotics for 8-12 weeks.
- After your flare-up, introduce animal proteins rich in glutamine at each meal, and supplement with glutamine for 8-12 weeks as well.

Image: Nature Made
CONCLUSIONS
Phew! You made it through and unscathed I hope. You now have (hopefully) a better understanding of what diverticulitis is, what causes/worsens it, and little steps to calm your guts down while nurturing the healing process.
The Four R Program above should get you on the right path while you work with your family physician. There are other things that you can certainly do to motor your digestive health along, but I think basics matter most. May you have the happiest digestive system ever!
References
1. Munie ST, Nalamati SPM. Epidemiology and pathophysiology of diverticular disease.Clin Colon Rectal Surg. 2018;31(4):209-213. doi:10.1055/s-0037-1607464.
2. Canadian Digestive Health Foundation. https://cdhf.ca/en/digestive-conditions/diverticular-disease/. Accessed Nov 25, 2025.
3. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/diverticulitis/multimedia/diverticulosis-and-diverticulitis/img-20006098. Accessed Nov 25, 2025.
4. Böhm SK. Risk factors for diverticulosis, diverticulitis, diverticular perforation, and bleeding: A plea for more subtle history taking.Viszeralmedizin. 2015;31(2):84-94. doi:10.1159/000381867.
5. Carr S, Velasco AL. Colon Diverticulitis. Treasure Island (FL): StatPearls Publishing; https://www.ncbi.nlm.nih.gov/books/NBK541110/. Updated July 25, 2024. Accessed Nov 26, 2025.
6. Sikander A, Rana SV, Prasad KK. Role of serotonin in gastrointestinal motility and irritable bowel syndrome.Clin Chim Acta. 2009;403(1-2):47-55. doi:10.1016/j.cca.2009.01.028.
7. Jastrzębski M, Nehring P, Joniec-Maciejak I, Wawer A, Przybyłkowski A. Serotonin metabolism and serotonin receptors expression are altered in colon diverticulosis.Medicina (Kaunas). 2023;59(11):1-10. doi:10.3390/medicina59111945.
8. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/10352-diverticulitis. Accessed November 27, 2025.
9. Lord RS, Bralley JA. Laboratory Evaluations for Integrative and Functional Medicine.2nd ed. Duluth, GA: Genova Diagnostics; 2012.
10. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK506996/. Updated Dec 28, 2021. Accessed Nov 27, 2025.
11. Dahl C, Crichton M, Jenkins J, et al. Evidence for dietary fibre modification in the recovery and prevention of reoccurrence of acute, uncomplicated diverticulitis: A systematic literature review.Nutrients. 2018;10(2):1-18. doi:10.3390/nu10020137.
12. Peery AF, Shaukat A, Strate LL. AGA Clinical practice update on medical management of colonic diverticulitis: Expert review.Gastroenterology. 2021;160(3):1-11. doi:10.1053/j.gastro.2020.09.059.
13. Strate LL, Morris AM. Epidemiology, pathophysiology, and treatment of diverticulitis.Gastroenterology. 2019;156(5):1282-1298. doi:10.1053/j.gastro.2018.12.033.
14. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK507004/#:~:text=Go%20to:-,Symptoms,go%2C%20the%20pain%20gets%20worse. Updated Dec 28, 2021. Accessed Nov 29, 2025
15. Mayo Clinic. https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/diverticulitis-diet/art-20048499. Accessed Nov 29, 2025.
16. Aune D, Sen A, Norat T, Riboli E. Dietary fibre intake and the risk of diverticular disease: a systematic review and meta-analysis of prospective studies.Eur J Nutr. 2020;59(2):421-432. doi:10.1007/s00394-019-01967-w.
17. Wegermann, Kara et al. An Insoluble Mystery: Fiber and Diverticulitis. Gastroenterol.158(4); 1167-1168
Cleveland Clinic. https://health.clevelandclinic.org/whats-the-difference-between-soluble-and-insoluble-fiber. Accessed Dec 2, 2025.
18. Cleveland Clinic. https://health.clevelandclinic.org/whats-the-difference-between-soluble-and-insoluble-fiber. Accessed Dec 2, 2025.
19. Piccioni A, Franza L, Brigida M, et al. Gut microbiota and acute diverticulitis: role of probiotics in management of this delicate pathophysiological balance.J Pers Med. 2021;11(4):1-10. doi:10.3390/jpm11040298.
20. Kim MH, Kim H. The roles of glutamine in the intestine and its implication in intestinal diseases.Int J Mol Sci. 2017;18(5):1051. doi:10.3390/ijms18051051.
21. Pallotta L, Cammisotto V, Castellani V, et al. Diverticular disease worsening is associated with increased oxidative stress and gut permeability: New insights by circulating biomarkers.Antioxidants (Basel). 2023;12(8):1537. doi:10.3390/antiox12081537.
22. Moonwiriyakit A, Pathomthongtaweechai N, Steinhagen PR, Chantawichitwong P, Satianrapapong W, Pongkorpsakol P. Tight junctions: from molecules to gastrointestinal diseases.Tissue Barriers. 2023;11(2):115-146. doi:10.1080/21688370.2022.2077620
23. Cleveland Clinic. https://my.clevelandclinic.org/health/articles/glutamine. Accessed Dec 6, 2025.
24. Deters BJ, Saleem M. The role of glutamine in supporting gut health and neuropsychiatric disorders. Food Sci Hum Wellness. 2021;10(2021):149-154. doi:http://10.1016/j.fshw.2021.02.003.
-Michael McIsaac