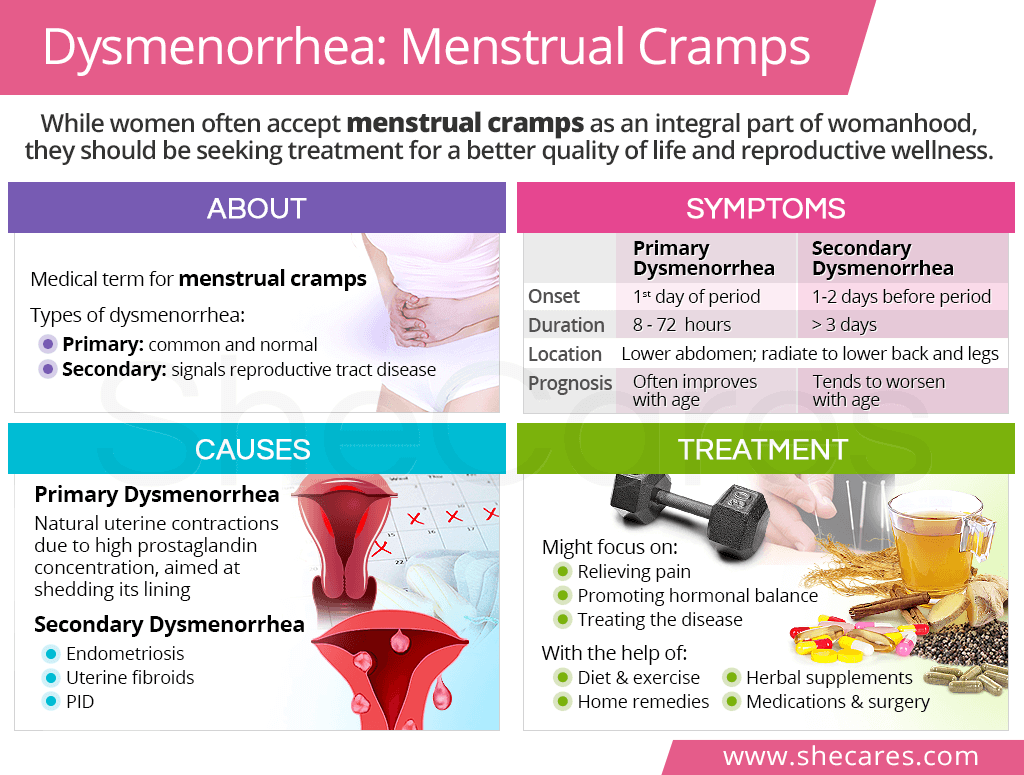
Dysmenorrhea is defined as painful menstruation and is characterized by two types: primary dysmenorrhea characterized by no disease (PD) and secondary dysmenorrhea (SD), which is characterized by diseased organs within the pelvic regions (Reisner & Reisner, 2017). The following sections will explore dysmenorrhea in greater detail, in addition to nutritional interventions to help attenuate pain and discomfort.

PD is the more common type of dysmenorrhea and presents with pain (cramps) before menstruation lasting for approximately 24-48 hours (Reisner & Reisner, 2017). Typically, menstrual periods are painful for the first 1-2 years after initial onset (adolescence), and will not become painful unless ovulation initiates. Cramping during the menstrual cycle is initiated by prostaglandins; fatty acid derivatives, which induce widespread physiological events within the human body (Reisner & Reisner, 2017).

Prostaglandins are created within the endometrium and under the influence of progesterone, an endogenous steroid hormone produced by the ovary. When the endometrium begins breaking down during menstruation, prostaglandins are released causing contractions (spasmodic) within the myometrium (Reisner & Reisner, 2017). Pain can be controlled with pharmacological agents such as ibuprofren or oral contraceptives. However, such agents can present side effects.

Bello, Kent, Grahn, Rice, and Holt (2014) stated that use of ibuprofren for pain management can increase the risk for gastrointestinal damage, while Reisner & Reisner (2017) noted that oral contraceptives can increase the risk of blood clots. Other alternatives do exist, which attenuates inflammation and pain while having minimal side affects. One such alternative is omega-3 polyunsaturated fatty acids (PUFAs).
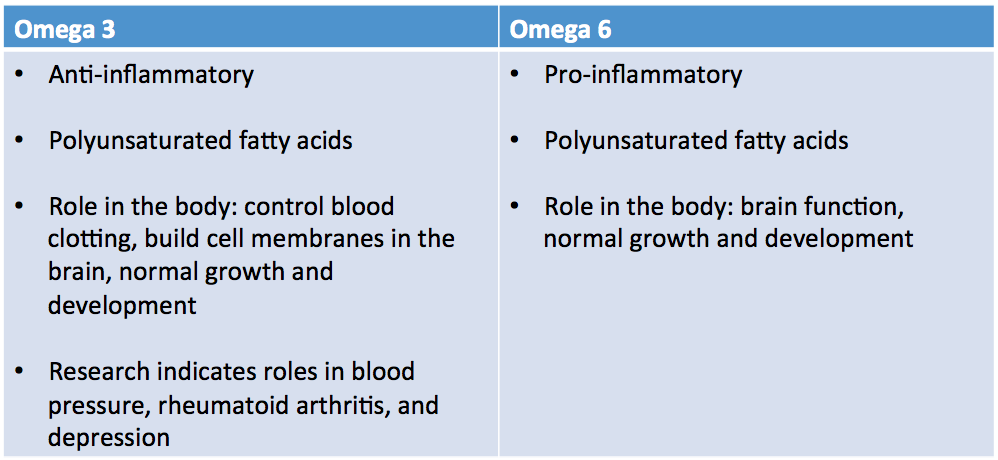
Omega-6 and omega-3 PUFAs undergo a biochemical change once absorbed from food. The metabolic products of both PUFAs include eicosanoids, which are signaling molecules that control immune and inflammatory reactions in the body (Ilich, Kelly, Kim, & Spicer, 2014. Omega-6 (pro-inflammatory) eicosanoids include prostaglandin E2, leukotriene B4, and thromboxane A2. Eicosanoids are synthesized by the enzymes lipoxygenase-5 and cyclooxygenase-2 (Ilich et al., 2014). Omega-3 eicosanoids (anti-inflammatory), include prostaglandin E3, leukotriene B5, resolvins and protectins.
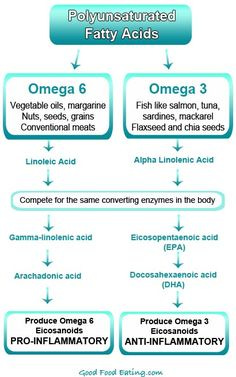
Of particular relevance is that anti-inflammatory eicosanoids also use lipoxygenase-5 and cyclooxygenase-2; both PUFAs compete for use of lipoxygenase-5 and cyclooxygenase-2. Thus, if more omega-6 fatty acids are present in the diet than omega-3 fatty acids, more pro-inflammatory signaling molecules are created, and larger levels of systemic inflammation will occur (Ilich et al., 2014). Low-grade chronic inflammation (LGCI) from overconsumption of omega-6 PUFAs perpetuates the production and levels of the pro-inflammatory signaling molecules. Thus, balancing the ratios of omega-3 and omega-6 PUFAs in the diet is paramount if an individual wishes to control inflammation in the body, including menstrual cramps. Good sources of omega-3 PUFAs include algae, fatty fish, fish oil, flaxseed oil, omega-3 enriched eggs, seal, krill oil, and grass fed animal meats (Tur, Bibiloni, Sureda, & Pons, 2012). Although said list is not exhaustive, incorporation of omega-3 PUFAs into the diet has been shown to reduce menstrual cramp pain (Harel, Biro, Kottenhahn, & Rosenthal, 1996).

Harel, Biro, Kottenhahn, and Rosenthal (1996) recruited 42 adolescents with dysmenorrhea, and participants were randomly assigned to two groups. The first group 21 females received fish oil (1080 mg ecosapentaenoic acid, 720 mg docosahexaenoic acid, and 1.5 mg vitamin E) daily for 2 months followed by a placebo for another 2 months. In the second group, 21 females received a placebo for the first 2 months, followed by fish oil for another 2 months (Harel et al., 1996). Results indicated no difference in the Cox Menstrual Symptom Scale (used to assess response to treatment) between the two groups at baseline after 2 months of placebo administration. However, after 2 months of treatment with fish oil, there was a marked reduction in the Cox Menstrual Symptom Scale.
In conclusion, pharmacological agents have been shown to manage inflammation and pain in individuals with dysmenorrhea. However, evidence supports the efficacy of other natural alternatives such as omega-3 PUFAs. If pain can be attenuated from omega-3 rich sources, such a fatty acid might serve as a compliment to traditional interventions.
References
Bello, A. E., Kent, J. D., Grahn, A. Y., Rice, P., & Holt, R. J. (2014). Risk of upper gastrointestinal ulcers in patients with osteoarthritis receiving single-tablet ibuprofen/famotidine versus ibuprofen alone: Pooled efficacy and safety analyses of two randomized, double-blind, comparison trials. Postgraduate Medicine, 126(4), 82-91.
Harel, Z., Biro, F. M., Kottenhahn, R. K., & Rosenthal, S. L. (1996). Supplementation omega-3 polyunsaturated fatty acids in the management of dysmenorrhea in adolescents. American Journal of Obstetrics and Gynecology, 174(4), 1335-1338.
Ilich, J.Z., Kelly, O.J., Kim, Y., & Spicer, M.T. (2014). Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Archives of Industrial Hygiene and Toxicology, 65(2), 139-148.
Reisner, E. G., & Reisner, H. M. (2017). An introduction to human disease: Pathology and pathophysiology correlations (10th ed.). Burlington, MA: Jones & Bartlett Learning.
Tur, J. A., Bibiloni, M. M., Sureda, A., & Pons, A. (2012). Dietary sources of omega 3 fatty acids: public health risks and benefits. British Journal of Nutrition, 102(S2), 23-52.
-Michael McIsaac
