
Gastroesophageal reflux disease (GERD) is a common condition affecting as much as 48% of Westernized countries (Ebrahimi-Mameghani, Sabour, Khoshbaten, Arefhosseini, & Saghafi-Asl, 2017). Such a health problem, left unmanaged, can lead to and produce other conditions such as gastrointestinal bleeding and esophageal stricture (narrowing). Thus, detection and management of said condition is paramount. As a means of appreciating GERD, the following will explore the disease further, in addition to factors associated with the condition as well as potential nutritional interventions to manage and mitigate symptoms.
Typical symptoms of GERD include reflux, a burning sensation, and acid regurgitation in the mouth (Ebrahimi-Mameghani et al., 2017). Furthermore, GERD is a strong rick factor for Barret’s esophagus (a change in mucosal lining of the esophagus) and esophageal adenocarcinoma (EA) (Ebrahimi-Mameghani et al., 2017). Such symptoms negatively impact individuals’ quality of lives at home, and at work. As such, it is imperative to not only appreciate the signs, symptoms, and pathophysiology; it is essential that individuals understand nutritional factors which might exacerbate the condition. Such an approach will allow those suffering from GERD to appropriately identify and remove such irritants from their diets. The following will consider such factors which exacerbate GERD.
Ebrahimi-Mameghani et al. (2017) recruited 250 patients (217 completed the study) experiencing GERD, which was determined by a checklist. The list included questions regarding the frequency (at least weekly or monthly) and type of symptoms as well as confirmation of heartburn and regurgitation; two defining characteristics of the disease. Each participant was also provided with a 3-day dietary record and instructed to record the type and amount of dietary macronutrients consumed, to include two weekdays and one weekend (Ebrahimi-Mameghani et al., 2017). Finally, subjects were instructed by a trained dietitian to consume their usual diet. Of the 250 participants who filled out the GERD checklist, 217 also filled out and returned their 3-day dietary records with 106 reporting GERD symptoms. 65.1% (69 cases) of the 106 individuals had weekly symptoms and 34% (37 cases) had monthly symptoms (Ebrahimi-Mameghani et al., 2017). The remaining subjects who did not report GERD were allocated to the control group.
When comparing the case and control groups, both consumed similar total amounts of carbs, protein, and fat with similar frequencies of meals during the day. Furthermore, caloric density and total frequency and meal volume were similar.What was statistically significant and different between both groups were the composition of the lunch and evening snacks (Ebrahimi-Mameghani et al., 2017). Specifically, the researchers determined significant associations between GERD symptoms and the percentage of energy from protein in total diet, amount of fat at lunch, amount of sugar and energy intake at evening snacks (Ebrahimi-Mameghani et al., 2017).

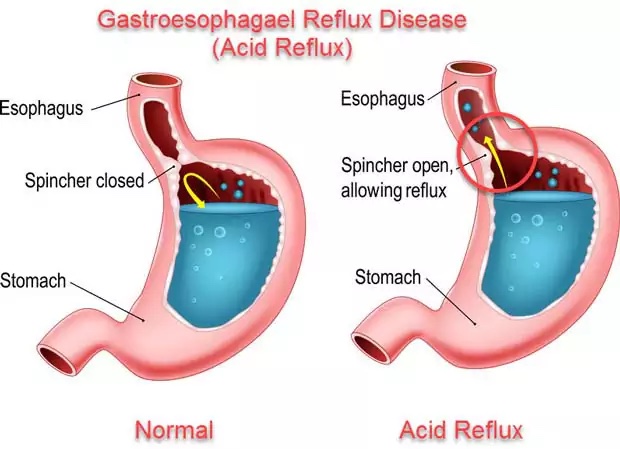
Of particular interest was a possible influence of fat consumed during lunch and GERD symptoms; fats consumed during lunch seemed to worsen symptoms while the percentage of energy from total protein/amount of protein at evening snack appeared to reduce symptoms (as long as meal volume was low) (Ebrahimi-Mameghani et al., 2017). The researchers postulated higher protein in the evening stimulated gastric emptying via increasing the lower esophageal sphincter (LES) pressure and stimulating gastric secretions. Ebrahimi-Mameghani et al. (2017) also suggested that GERD symptoms might have risen during lunch because of fat content and the trend of said meal generally being the largest meal of the day; higher volume increase gastric distension and likelihood of reflux by transient relaxion of the LES; a defining characteristic of GERD (Ebrahimi-Mameghani et al., 2017).
In conclusion, GERD is a condition affecting a considerable proportion of Westernized countries. Left unmanaged, GERD can lead to and produce other conditions such as gastrointestinal bleeding, esophageal stricture, and cancer. Food type and amount can exacerbate such symptoms. Conversely, managing food choices and volumes with particular focus on lower fat foods during lunch and higher percentage of protein relative to total energy in the evening meal is associated with decreased symptoms amongst individuals with GERD symptoms. Such knowledge might prove useful in helping control acid reflux.
References
Ebrahimi-Mameghani, M., Sabour, S., Khoshbaten, M., Arefhosseini, S. E., & Saghafi-Asl, M. (2017). Total diet, individual meals, and their association with gastroesophageal reflux disease. Health Promotion Perspectives, 7(3), 155-162.
-Michael McIsaac
