Celiac disease (CD) can be defined as an inherited autoimmune disease estimated to affect 1 out of every 133 asymptomatic people (Gaillard, 2016). Individuals with CD who consume gluten (a protein found in wheat, rye, barley, and their derivatives) damage absorptive villi of the duodenum, leading to malabsorbtion of important nutrients (Gaill ard, 2016).
Non-celiac gluten sensitivity (NCGS) is characterized by intestinal and extra-intestinal symptoms related to the ingestion of gluten-containing food, in subjects that are not affected by either celiac disease or wheat allergy. NCGS has been reported to affect up to 5– 10% of western population and gluten-free foods among non-celiac patients have grown in popularity. Considering that CD and NCGS exist, should those without the aforementioned conditions pursue a gluten-free (GF) diet?
If an individual does not have CD or NCGS, there is no threat to the irritation and inflammation to the gut lining. However, there does exist a concern that pursuing a gluten free diet may cause a higher insulin response in gluten-free foods (Scazzina, Dall’Asta, Pellegrini, & Brighenti, 2015). Scazzina et al. (2015) examined the glycemic index (GI) of 10 commercial foods aiming to update the GI values of the most common GF products consumed in Italy. The in vivo GI was evaluated for six bakery products and four types of pasta. The postprandial glucose response was obtained in two groups with 10 healthy volunteers each.

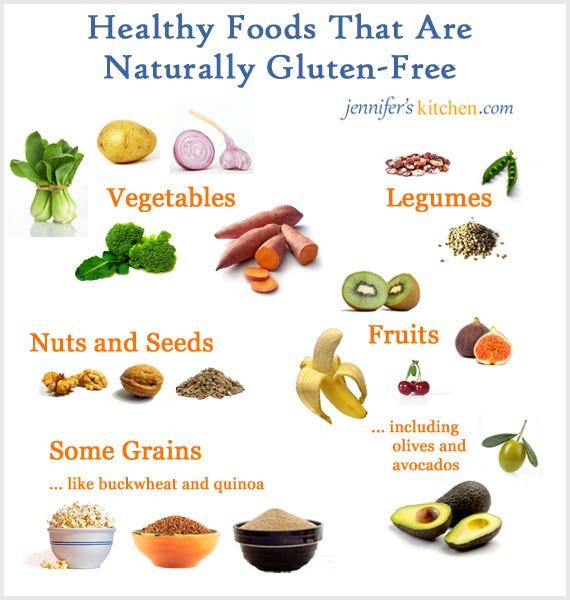
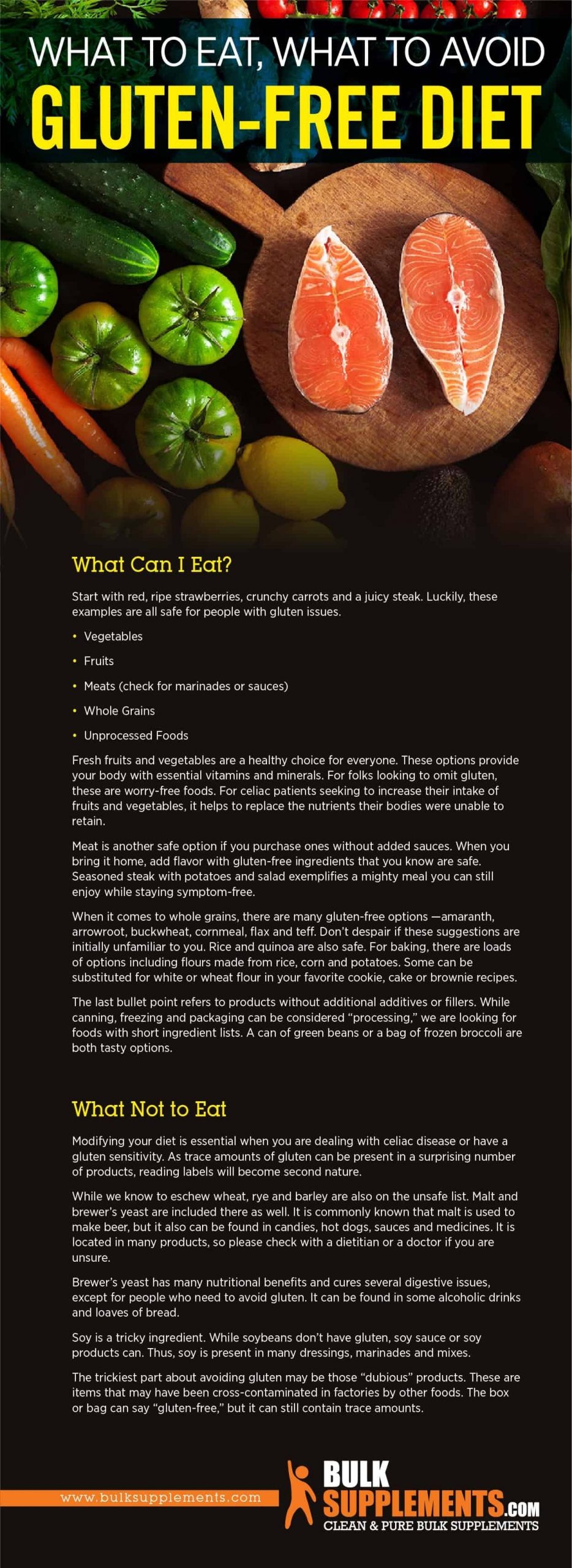
Results indicated that several commercial GF products exhibited low and medium GI values, not confirming the previous observations from older studies on the high GI of GF foods (Scazzina et al., 2015). The researchers cited that enhanced methods of producing foods might have attenuated the GI response. Scazzina et al. (2015) also noted that there exists a plethora of GF foods that still may drive postprandial blood glucose high. The researcher’s intent, however, was to indicate that not all GF foods created high GI responses. Thus, some GF foods provide the opportunity to induce lower GI responses, possibly offering foods beneficial to the general population. However, another question remains; if individuals do not have CD or NCGS, should they eat gluten-containing products anyways?
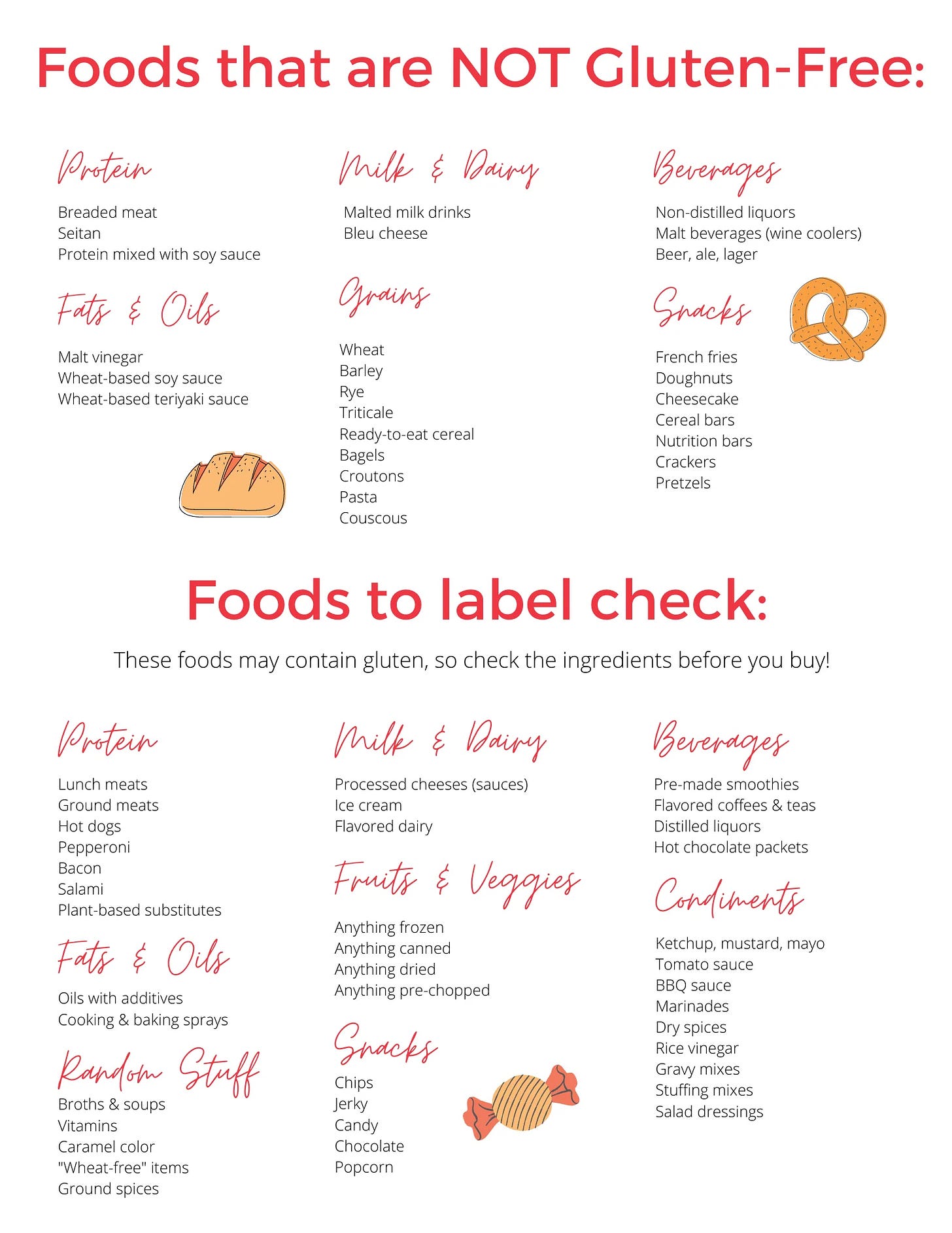
As previously mentioned, gluten is a term used to describe proteins found in grains (i.e., wheat, barley, rye). Gluten is also used in processed foods because it has viscoelastic properties helping provide shape and structure (Diaz-Amigo & Popping, 2012). Of particular interest is the shift in polyunsaturated fatty acid (PUFA) ratios circa early to mid nineteenth century, after the inclusion of the aforementioned grains in animal diets and processed foods. Such a change increased the prevalence of omega-6 fatty acids in both meat and packaged food products (Ilich, Kelly, Kim, & Spicer, 2014).
Since then, PUFA ratios between omega-6 and omega-3 have shifted from 1-2:1 to as high as 15:1 in modern diets, respectively (Ilich et al., 2014). The aforementioned change in PUFA ratios has increased low-grade chronic inflammation and has been linked to several diseases such as obesity, cardiovascular disease, insulin resistance, and type-2 diabetes (Ilich et al., 2014). Collectively the aforementioned diseases have been termed metabolic syndrome (Kenney, Wilmore, & Costill, 2012).
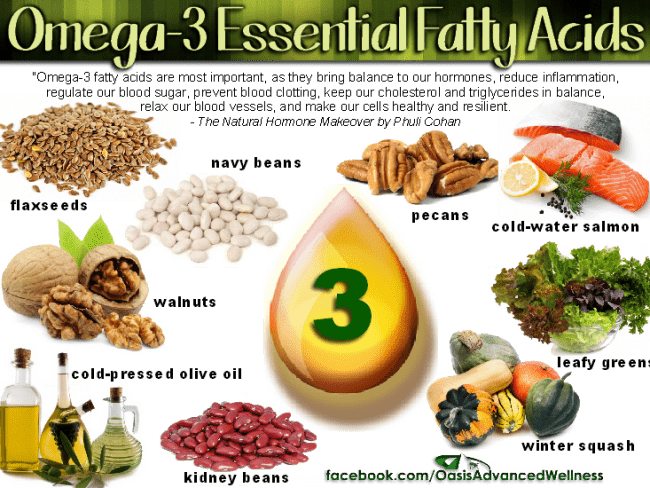
In conclusion, gluten free products are an alternative for those with CD and NCGS, while also providing a lower glycemic response compared to older processing methods. It is also known that gluten does not appear to harm those free of CD and NCGS. However, products that do contain gluten are generally processed, and contain other compounds that can induce low-grade chronic inflammation, which has been correlated to metabolic syndrome. Thus, an argument could be made for individuals to avoid processed foods whether they do or do not have GS or NCGS.
References
Diaz-Amigo, C., & Popping, B. (2012). Gluten and gluten-free: Issues and considerations of labeling regulations, detection methods, and assay validation. Journal of AOAC,95(2), 337-348.
Gaillard, L. A. (2016).Navigating gluten-related health disorders and nutritional considerations of gluten-freediets. North Carolina Medical Journal, 77(3), 180-182.
Ilich, J.Z., Kelly, O.J., Kim, Y., & Spicer, M.T. (2014). Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Archives of Industrial Hygiene and Toxicology, 65(2), 139-148.
Kenney, W.L., Wilmore, J.H., & Costill, D.L. (2012). Physiology of sport and exercise (5th ed.). Champaign, IL: Human Kinetics.
Molina-Infante, J., Santolaria, S., Sanders, D. S., & Fernandez-Banares, F. (2015). Systematic review: Non-celiac glutensensitivity. Alimentary Pharmacology & Therapeutics, 41(9), 807-820.
Scazzina, F., Dall’Asta, M., Pellegrini, N., & Brighenti, F. (2015). Glycaemic index of some commercial gluten-free foods. European Journal of Nutrition, 54(6), 1021-1026.
-Michael McIsaac
