
Rheumatoid arthritis (RA) is a systemic autoimmune disease, which effects the connective tissues of the body with a particular locus about the joints.1 RA is characterized as a chronic, disabling, and deforming condition affecting multiple joints, especially along the hands and feet.1(731) The onset of RA is known to be driven by environmental and genetic factors. However, the microbiome is now considered a third impetus behind the development of RA.2 As a means of appreciating the RA/gut relationship, the following will consider biomarkers indicating disruptions in gastrointestinal homeostasis and its downstream effects on the body, to include inflammatory joint conditions.
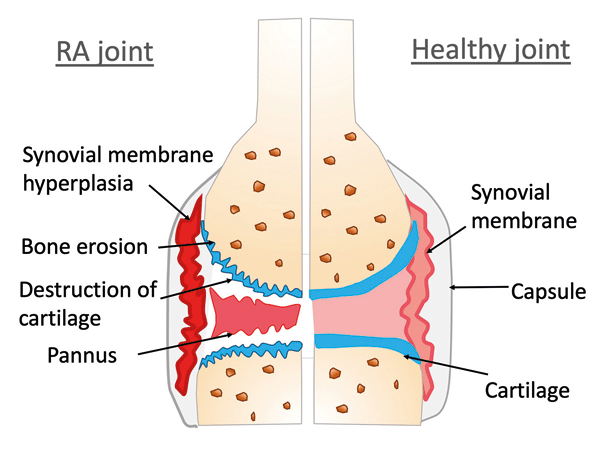
RA is encountered most frequently among young and middle-aged females. Once the inflammatory effects of RA reach the joints, a steady degradation and thickening of the synovial membrane of the joint occurs.1(731) The inflammatory cascade continues its reach across the surface of articular cartilage, eventually destroying the contact points between bones. As RA continues to manifest, the severe breakdown of cartilage makes the joint surface unstable leading to deviation/displacement of bones.1(731) Ultimately, painful and restricted range of motion ensues. As such, it is imperative that all major contributors to the etiology of RA are addressed, including optimization of gut health and function.
SUMMARY:
RA is a progressive condition
RA can limit activities of daily living and quality of life
Early interventions are paramount
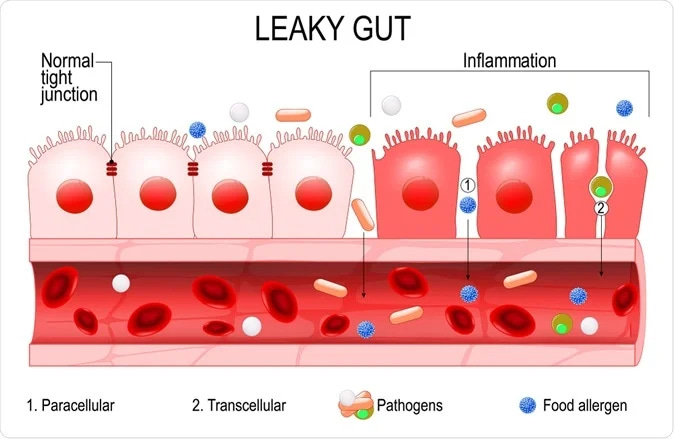
As discussed in previous posts, the intestinal tract lining not only blocks pathogens from entering and interacting with the immune system; the mucosal barrier must also manage chemical and physiological impositions from pancreatic enzymes and gastric juices.3 Therefore, the epithelial cells of the outermost cellular barrier must be constantly replaced due to degradation, and must form tight junctions (TJs) to maintain integrity.3(425) It is the tight junction structure that, when dysregulated, can allow pathogens and food particles to become undesirably close to components of the immune system.3 One set of factors known to disrupt TJs are inflammatory processes which emanate from food allergies.4
SUMMARY
The gastrointestinal lining (GIL) is selectively permeable (when working optimally)
The GIL TJs can become dysregulated = leaky gut
Leaky gut can drive autoimmunity and GIL inflammation
Leaky gut can be (but is not limited to) caused by food allergies
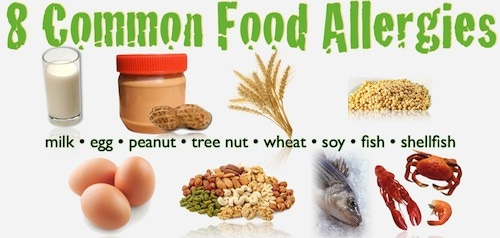
If an individual reports joint stiffness and swelling, this author would recommend a food allergy test (FAT). If, for example, an individual’s food allergy test result indicated a moderate to high sensitivity to gluten, eggs, dairy, soy, peanuts (common allergens), this author would recommend removal of the same.5 If FAT is not available, this author would assume an individual is allergic to the same and still remove as a matter of caution in the absence of lab results. Such a process would represent phase one of the Four R Program (Remove, Reintroduce, Reinnoculate, Repair), also known as FRP.3(454) In the following section, the second step of phase one FRP will be considered; the identification and control of pathogenic microbes.
SUMMARY
Symptoms such as joint stiffness and swelling might indicate a need for a food allergy test
If food allergies are uncovered, remove said foods
If food allergy test unavailable, consider removal of commonly understood foods: dairy, eggs, tree nuts, peanuts, wheat, soy, fish, shellfish
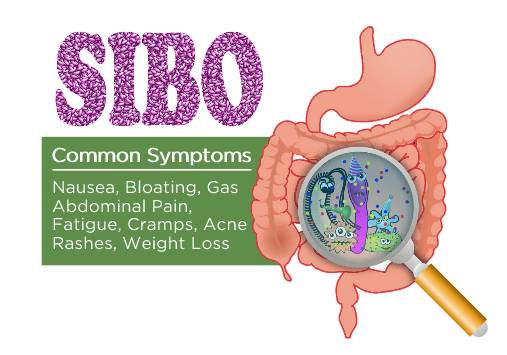
Once allergenic foods have been identified/assumed, the second step of phase one FRP is identification and removal of overpopulated/pathogenic bacteria, fungi, viruses, and parasites. If high levels of phenylacetate (PAA), p-hydroxyphenylacetate (HPA), D-lactate, D-arabinitol are identified as well as the presence of Klebsiella pneumoniae, Pseudomonas aeruginosa, and low Lactobacillus, steps should be taken to address the same. In the following sections, each marker will be considered in greater detail as well as interventions to control growth and proliferation.
SUMMARY
If available, have stool and organic acids tests conducted to see if dysbiosis is present
Organic acids tests: phenylacetate (PAA), p-hydroxyphenylacetate (HPA), D-lactate, D-arabinitol
Microbes in stool: Klebsiella pneumoniae, Pseudomonas aeruginosa, and low Lactobacillus
If markers suggest presence of dysbiosis, seek interventions to manage the same
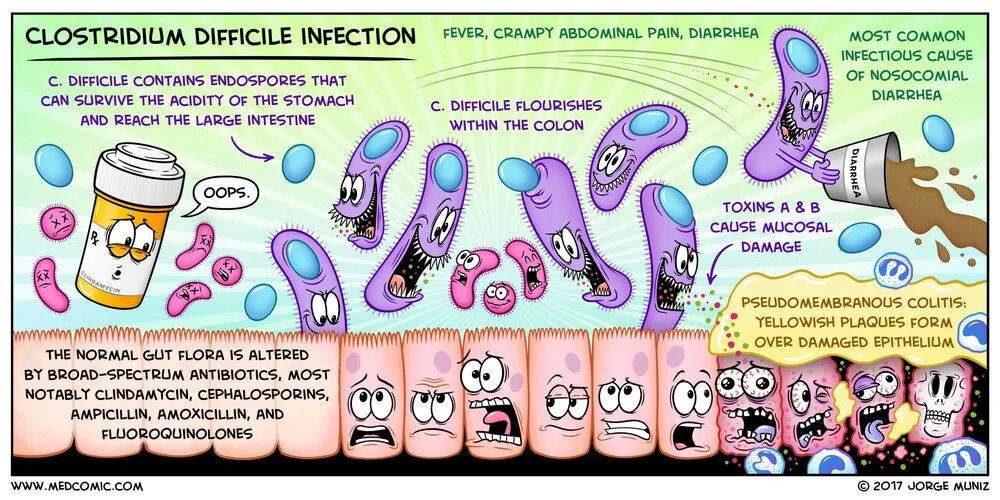
High PAA (an organic acid) is caused by intestinal bacteria, which increase PAA levels when they interact with dietary polyphenols (from plant food).3(376) Ultimately, individuals with normal intestinal function will have only background levels of PAA in the urine. High HPA indicates tyrosine breakdown from Clostridium difficile and P. vulgaris.3(378)Clostridium difficile is responsible for severe diarrhea and life-threatening inflammation of the colon, while P. vulgaris is considered an undesirable microbe in the gut as it is a causative agent of diarrhea.6,7 Implementation of berberine, citrus seed extract, and garlic may help control overgrowth.3(390) However, due to the potential life-threatening possibility of said bacteria (Clostridium difficile), medical intervention should be encouraged if stool tests confirm its presence.
SUMMARY
Higher levels of PAA may indicate presence of Clostridium difficile and P. vulgaris
Can cause diarrhea
Berberine, citrus seed extract, and garlic can support/lower growth of Clostridium difficile and P. vulgaris
Bottom line: if said microbes are high and diarrhea present, seek medical attention
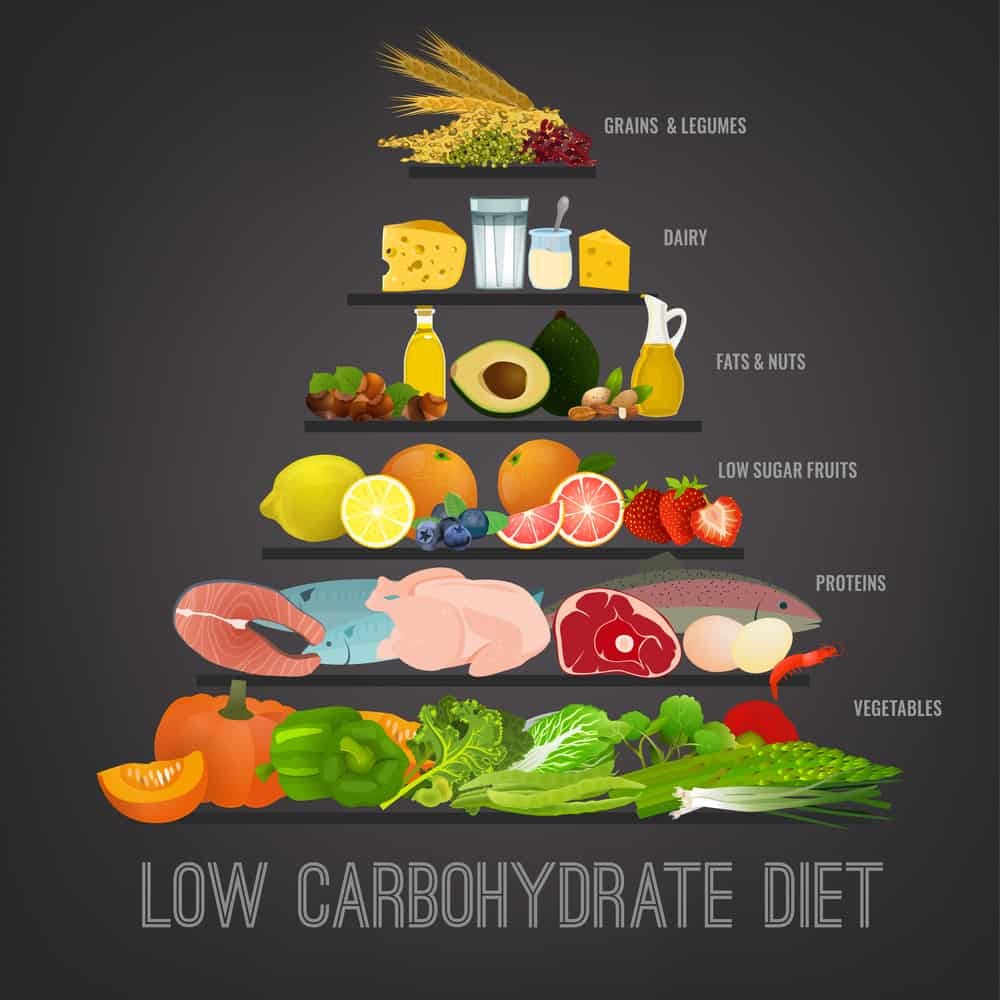
High D-lactate indicates poor digestion and absorption of dietary carbohydrates.3(384) Several strains of bacteria, including Lactobacillus plantarum, that normally populates the human gut have the capacity of converting simple sugars into D-lactate; a metabolite of such a process.3(385) Left unmanaged, it is possible that D-lactate production can exceed clearance leading to lactic acidosis.3(385) Thus, one method of controlling high D-lactate levels is through removal and/or minimization of simple sugars in the diet, which could help control the production of D-lactate and associated symptoms. High D-arabinitol indicates the overgrowth of fungus (Candida) in the gut, which proliferates in the presence of carbohydrate sources.3(387)8 Thus, removal of simple sugars will control growth of both Lactobacillus and Candida. Oil of oregano, caprylic acid, and Saccharmyces boulardii can also be helpful in controlling fungal overgrowth.3(390,455)
SUMMARY
D-lactate (organic acids test), if high, suggests poor management of carbohydrates from overgrowth of Lactobacillus plantarum
If organic acid is high (out of range), consider lowering/removal of starchy carbohydrates and simple sugars
If High D-arabinitol is high (out of range), Candida is present = reduce starchy carbohydrates and simple sugars
Oil of oregano, caprylic acid, and Saccharmyces boulardii help control fungal overgrowth
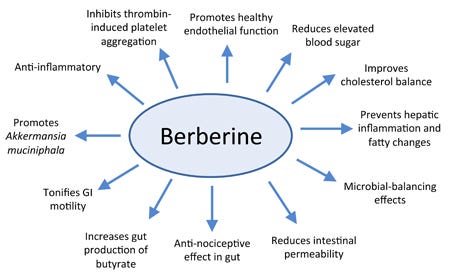
Klebsiella pneumoniae and Pseudomonas aeruginosa are opportunistic bacteria that can negatively affect an individual’s health if they over-dominate the intestinal tract. Klebsiella pneumoniae is part of the Enterobacteriaceae family and is characterized as a gram-negative bacterium.9 Virulence of said bacteria is provided by many factors which can produce antibiotic resistance and infection to include sepsis, meningitis, and pneumonia.9(1) Pseudomonas aeruginosa is also a pathogenic, gram-negative bacteria which has developed resistance to the majority of antimicrobial/antibiotic interventions due to a protective biofilm that it produces.10 Therefore, such a bacterium is particularly lethal amongst individuals with compromised immune systems. Berberine, citrus seed extract, and garlic may help control overgrowth.3(390) However, this author would strongly recommend medical input and intervention if the aforementioned bacteria are high in stool samples.
SUMMARY
If stool tests indicate high (out of range) Klebsiella pneumoniae and Pseudomonas aeruginosa, consider berberine/citrus seed extract/garlic to help control overgrowth
Bottom line: seek medical attention
The second phase of FRP (Reintroduce) is characterized by reintroduction of digestive enzymes, if found as deficient. This author would suggest checking gastric acidity (pH) as poor stomach acid (hypochlorhydria) has been responsible for reduced vitamin and mineral absorption, reduced protein digestion, small intestinal bacterial/fungal overgrowth, infection, and food allergies.3(419)11,12 If hypochlorhydria is determined (using the Heidelberg test; covered in this author’s previous posts), supplemental betaine hydrochloride can be used with each meal, slowly increasing doses up towards 4500 mg if necessary to return stomach acidity to a pH of 1-2.13If pancreatic digestive enzymes (measured through fecal elastase) are low, this author would also suggest supplementing with the same via pancreatic enzyme replacement therapy.
SUMMARY
Check stomach pH; if low (poor stomach acidity), consider betaine hydrochloride supplementation with each meal
Check fecal elastase; if low, consider supplementation with digestive enzymes for carbs, fats, proteins
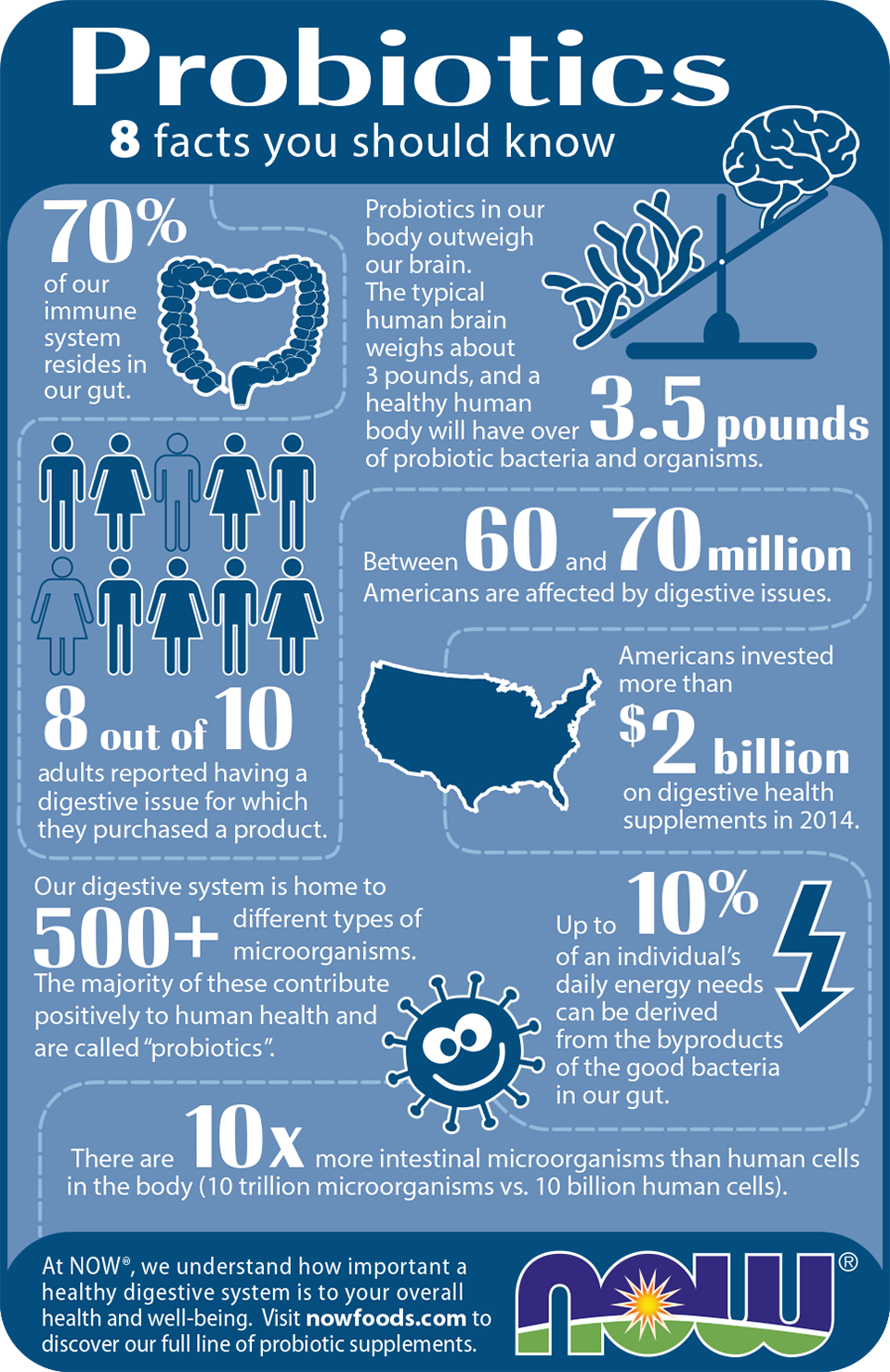
The third phase of FRP (Reinnoculate) is characterized by introducing beneficial microbes. As mentioned previously, probiotics are microorganisms which share a beneficial/harmonious relationship with the digestive system. Such microbes facilitate the prevention of diseases (i.e., inflammatory bowel disease and antibiotic associated diarrhea), modulate immune system function, enhance epithelial barrier function, and control the build-up of toxin-producing bacteria.14 Such beneficial probiotics could include L. acidophilus, L salvarius, L. plantarum, L. casei, and Saccharomyces boulardi.3(455) Having considered removal of foods that trigger immunity, controlling overgrowth of pathogenic bacteria, introducing digestive enzymes, and the reinnoculation of the gut with beneficial microbes, the following will consider steps to further control inflammation, enhance intestinal repair, and mitigate nutritional deficiencies.
SUMMARY
If dysbiosis is present (from organic acids and stool tests), consider implementing L. acidophilus, L salvarius, L. plantarum, L. casei, and Saccharomyces boulardi
The fourth phase of FRP (Repair) concludes with repair of the intestinal wall. Tests such as secretory IgA (SIGA) can help confirm the need of such repair; SIGA is an antibody that is secreted by the gut lymphoid tissue which binds to pathogens and prevents them from penetrating the mucosal layer.3(431) If such a biomarker is low, it is likely that pathogens and allergens are entering and damaging enterocytes. Glutamine is an amino acid that serves as a dominant fuel and nitrogen source for enterocytes; cells which become damaged from allergens and pathogenic bacteria.15 Said amino acid also inhibits IP/bacterial translocation/cell death and maintains mucosal integrity indicating the need for appropriate levels.1(1001) This author would also consider use of zinc, vitamins A/C/E/folic acid (especially if formiminoglutamate biomarker is low), as well as essential fatty acids (Omega-3) and vitamin D3 to repair cell membranes and lower inflammation.3(455)16
SUMMARY
If secretory IgA is low (higher than normal use), it is likely that inflammation is occurring at the gut lining
Implement glutamine to help repair enterocytes (gut cells)
If secretory IgA is low, also consider zinc, vitamins A/C/E/folic acid/omega-3 fatty acids/D3 to control inflammation and support repair of enterocytes

After such an intervention, this author would consider checking for nutritional deficiencies, especially if fatigue remains present after implementation of FRP. Fatty acid metabolism (i.e., low adipate/ethylmalonate), carbohydrate metabolism, and energy production (i.e., low hydroxymethylglutarate) organic acids tests can be reviewed to help ensure optimal metabolism of energy substrates and use of the same. If markers were initially low, improving digestion and absorption from the previous steps in FRP is likely to improve said biomarkers. If markers continue to remain low, this author might suggest carnitine (facilitates fat transport into mitochondria) and riboflavin (helps oxidize fatty acids in mitochondria) to reduce adipate and ethylmalonate levels.3(328-329) If hydroxymethylglutarate remains low, such would indicate low CoQ10; a powerful antioxidant and substance responsible for producing energy in the mirochondria.3(340)Supplementation of the same would help correct low hydroxymethylglutarate/CoQ10 levels and help improve energy production while reducing symptoms of fatigue.
SUMMARY
If experiencing fatigue, and adipate and ethylmalonate levels (organic acids tests) are high, carnitine and riboflavin supplementation can help
If hydroxymethylglutarate levels low, consider supplementation with CoQ10
In conclusion, RA is a systemic autoimmune disease, which effects the connective tissues of the body with a particular locus about the joints. The onset of RA is known to be driven by environmental and genetic factors. However, the microbiome is now considered a third impetus behind the development of said condition. Implementation of FRP can help systematically improve digestion/absorption, reduce inflammation, boost immune system strength, reduce autoimmunity, and repair the gut lining. Ultimately, such steps can help support individuals’ recoveries from such conditions, and their return to improved quality of life.
References
1. Reisner EG, Reisner HM. An Introduction to Human Disease: Pathology and Pathophysiology Correlations. 10th ed. Burlington, MA: Jones & Bartlett Learning; 2017.
2. Kishikawa T, Maeda Y, Nii T, et al. Metagenome-wide association study of gut microbiome revealed novel aetiology of rheumatoid arthritis in the Japanese population. Ann Rheum Dis. 2020;79:103-111. doi:10.1136/annrheumdis-2019-215743.
3. Lord RS, Bralley, JA.Laboratory Evaluations for Integrative and Functional Medicine. 2nd ed. Duluth, GA: Genova Diagnostics; 2012.
4. Jurgelewicz M. Natural treatments for autoimmune diseases. Nutritional Perspectives Journal. 2013;36(2):1-7. https://thefunctionalmedicinecenter.com/about-dr-michael-jurgelewicz/. Accessed March 10, 2020.
5. Food Allergy: Symptoms and Causes. Mayo Clinic Website. https://www.mayoclinic.org/diseases-conditions/food-allergy/symptoms-causes/syc-20355095. Accessed March 10, 2020.
6. C. Difficile Infection: Symptoms and Causes. Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/c-difficile/symptoms-causes/syc-20351691. Accessed March 10, 2020.
7. Drzewiecka D. Significance and roles of Proteus spp. Bacteria in natural environments. Microb Ecol. 2016;72(4):741-758. doi:doi:10.1007/s00248-015-0720-6.
8. Jeziorek M, Frej-Mądrzak M, Choroszy-Król I. The influence of diet on gastrointestinalcandidaspp. colonization and the susceptibility of candida spp. to antifungal drugs. Rocz Panstw Zakl Hig. 2019;70(2):195-200. doi: 10.32394/rpzh.2019.0070.
9. Rodriguez-Manzano J, Miscourides N, Malpartida-Cardenas K, et al. Rapid detection of Klebsiella pneumonaie using an auto-calibrated ISFET-array lab-on-chip platform. IEEE. 2019:1-4. doi:10.1109/BIOCAS.2019.8919160.10.
10. Armijo LM, Wawrzyniec SJ, Kopciuch M, et al. Antibacterial activity of iron oxide, iron nitride, and tobramycin conjugated nanoparticles against Pseudomonas aeruginosa biofilms. J Nanobiotechnol . 2020;18(1):1-27. doi:https://doi.org/10.1186/s12951-020-0588-6.
11. Pizzorno J, Katzinger, J.Clinical pathophysiology: A Functional Perspective. Coquitlam, BC: Mind Publishing Inc; 2012.
12. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism. 7th ed. Boston, MA: Cengage Learning; 2018.
13. Surofchy DD, Frasetto LA, Benet LZ. Food, acid supplementation and drug absorption- A complicated gastric mix: A randomized control trial.Pharm Res. 2019;36(155):1-10. doi:https://doi.org/10.1007/s11095-019-2693-5.
14. Khalighi AR, Khalighi MR, Behdani R, et al. Evaluating the efficacy of probiotic treatments in patients with small intestinal bacterial overgrowth (SIBO)- A pilot study. Indian J Med Res. 2014;140(5):604-608.
15. Benjamin J, Makharia G, Ahuja V. Glutamine and whey protein improve intestinal permeability and morphology in patients with Crohn’s disease: A randomized controlled trial.Dig Dis Sci. 2012;57:1000-1012. doi: 10.1007/s10620-011-1947-9.
16. Raman M, Milestone AN, Walters JRF, et al. Vitamin D and gastrointestinal diseases: Inflammatory bowel disease and colorectal cancer. Therap Adv Gastroenterol. 2011;4(1):49-62. doi:10.1177/1756283X10377820.
-Michael McIsaac
