
Hashimoto’s thyroiditis (HT) is a thyroid disease whereby antithyroid antibodies and T-lymphocytes (part of the adaptive immune response) infiltrate and destroy cell components of the thyroid gland.1 Eventually, the thyroid gland loses its capacity to produce sufficient amounts of hormones necessary for normal function; an inevitable process which leads to hypothyroidism.1(661-662) As a means of appreciating HT, the following sections will cover HT in greater detail, as well as exploring interventions to support down-regulation of autoimmunity and chronic inflammation.
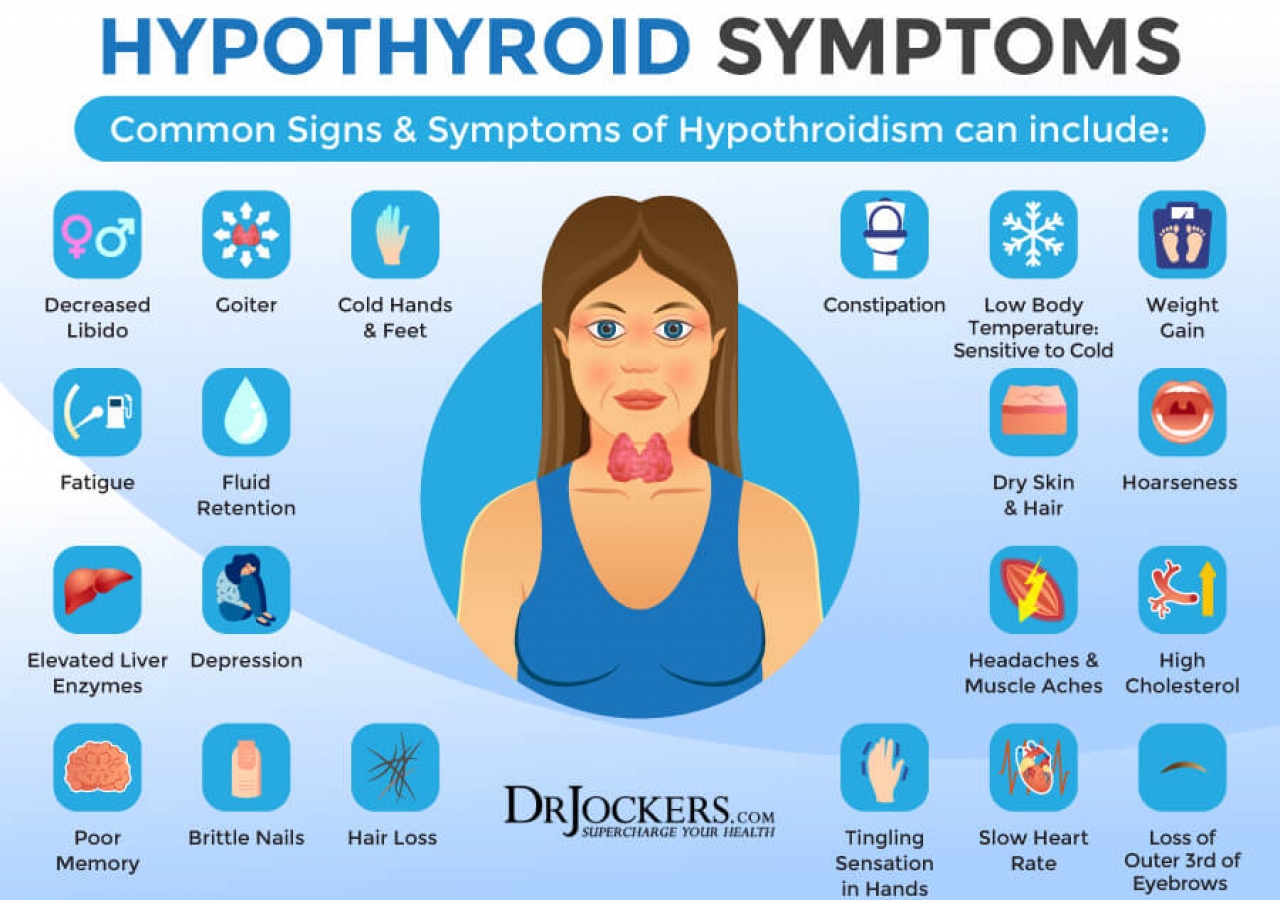
HT is the most common cause of hypothyroidism; a condition where the thyroid gland underproduces hormones known as T3 (triiodothyronine) and T4 (thyroxine).1(661),2 HT occurs predominantly in middle aged women while the primary pathogenic mechanism is destruction of thyroid stimulating hormone receptors (TSHR) by autoantibodies.1(661) TSHR’s are the interface between thyroid stimulating hormone (TSH) and the thyroid gland; a gateway allowing TSH to stimulate the thyroid cells to produce T3 and T4.1(661)Autoantibodies effectively destroy the communication link (TSHR) between TSH and the thyroid gland.
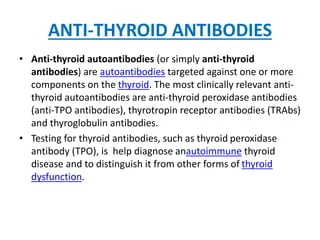
As autoantibodies continue to mount an attack upon the thyroid gland, more TSHRs become destroyed, deepening the degree of thyroid dysregulation. An individual with advanced HT will have a characteristically enlarged thyroid gland along the anterior portion of the neck.1(661) Such a change is induced by the infiltration of T-lymphocytes and plasma cells which relentlessly seek out and destroy glandular tissue.1(662) Although there is no known means to stop the attack and breakdown of the thyroid gland, there does exist both pharmacological and nutritional interventions to support hypothyroidism once it manifests.
Once an individual is diagnosed with insufficient T3 and T4 levels, thyroid hormones containing the same can be administered to compensate for such losses.1(662) However, attempting to elucidate the underlying cause of HT is equally relevant; one such causative factor could be dysregulated gut function. If digestion and absorption of food becomes compromised (i.e., leaky gut), inflammatory cascades can ensue in addition to entry of food particles and pathogens into the bloodstream.3 Such a process emanates from failure of the gut lining to control food particle/pathogen entry, inducing a powerful and expeditious inflammatory response from gut associated lymphoid tissue (GALT).3(427)
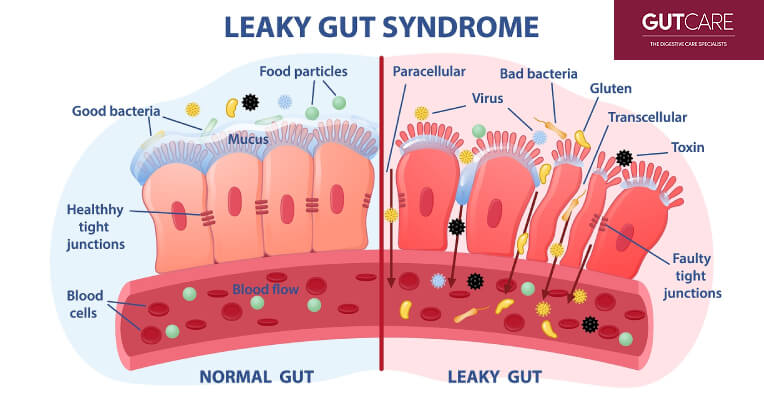
Once such a process has been initiated (leaky gut + inflammatory response), chronic inflammation, nutrient deficiencies, and the manifestation of other diseases begin, to include HT.3(417) The autoimmune response related to HT has been hypothesized to emanate from molecular mimicry; a process where a pathogen (i.e., bacterial or viral) shares structural similarities to normal tissue cells.4 Ultimately, the immune system indiscriminately attacks both pathogen and self-antigen. Though said process is considerably more complex than explained above, a point of emphasis could be consideration of how a pathogen entered the tissues.
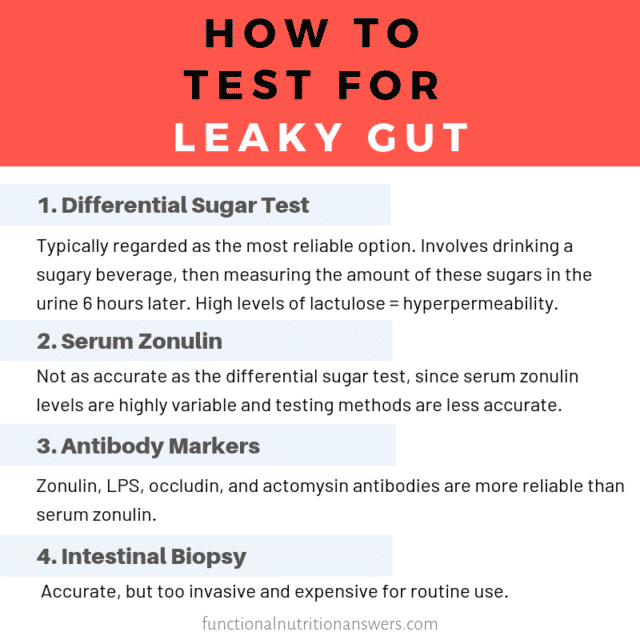
Considering that pathogens (i.e., viral/bacterial) can enter the body through a leaky gut it would be logical to consider both foods which could initiate such a process through allergy testing, as well as testing gut permeability through screening protocols such as the lactulose/mannitol test.3(426) If food allergies are elucidated which could worsen HT and overall inflammation, avoidance of said foods is warranted. If intestinal permeability has been identified, following the 4 R protocol (Remove, Reintroduce, Reinnoculate, Repair) is strongly indicated.3(454)
LINK: Assessing Gut Function
LINK: IBS Support: How The Four R Program Can Help
In conclusion, HT is a thyroid disease whereby antithyroid antibodies and T-lymphocytes (part of the adaptive immune response) infiltrate and destroy cell components of the thyroid gland. Eventually, the thyroid gland loses its capacity to produce sufficient amounts of hormones necessary for normal function; an inevitable process which leads to hypothyroidism. Although destruction of thyroid tissue is inevitable, detection and management of gut health, digestion, and absorption can support down regulation of inflammation. Ultimately, such steps can help improve overall health, energy levels, and quality of life.
References
1. Reisner EG, Reisner HM. An Introduction to Human Disease: Pathology and Pathophysiology Correlations. 10th ed. Burlington, MA: Jones & Bartlett Learning; 2017.
2. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism. 7th ed. Boston, MA: Cengage Learning; 2018.
3. Lord RS, Bralley JA. Laboratory Evaluations for Integrative and Functional Medicine. Duluth, GA: Genova Diagnostics; 2012.
4. Cusick MF, Libbey JE, Fujinami RS. Molecular mimicry as a mechanism of autoimmune disease. Clinic Rev Allerg Immunol. 2012;42:102-111. doi: 10.1007/s12016-011-8294-7.
-Michael McIsaac
