Hyperglycemia is a condition whereby glucose is poorly managed and stored throughout cells of the body. The degree of severity can be defined by multiple measures including fasting glucose tests (FGTs); less than 100 mg/dL is normal, ranges from 100 to 125 mg/dL is considered prediabetes.1 If two separate tests produce 126 mg/dL, or higher, a diabetic state is present.1 Additionally, hemoglobin A1C (HBA1C) tests can help support findings from an FGT; a HBA1C between 5.7 and 6.4 percent indicates prediabetes.1Finally, a HBA1C level of 6.5 percent, or higher on two separate tests, indicates diabetes.1 If pre-diabetes or diabetes is present, it is critical that nutritional interventions are employed to help improve blood glucose levels. As such, the following will consider the same using magnesium supplementation as nutritional support.

In previous posts, this author has covered causes of hyperglycemia/diabetes (H/D) and food strategies to improve/support the same. However, when nutritional and lifestyle interventions do not completely mitigate signs and symptoms of H/D, this author would suggest supplementation as a means of delivering therapeutic doses of micronutrients necessary to overcome deficiencies and/or associated pathophysiological conditions. One such supplement, when and where identified as appropriate, could be magnesium (MG). The following will consider MG in greater detail.
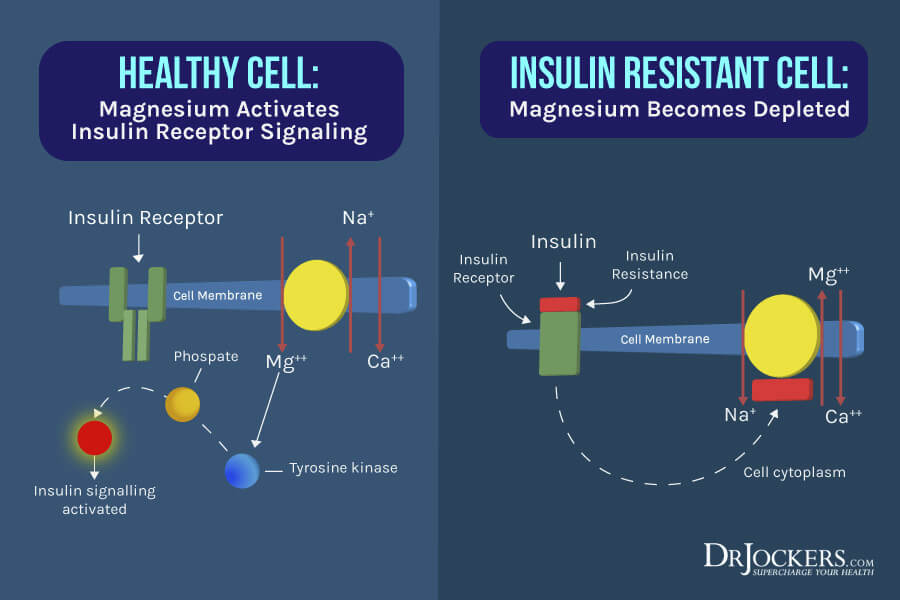
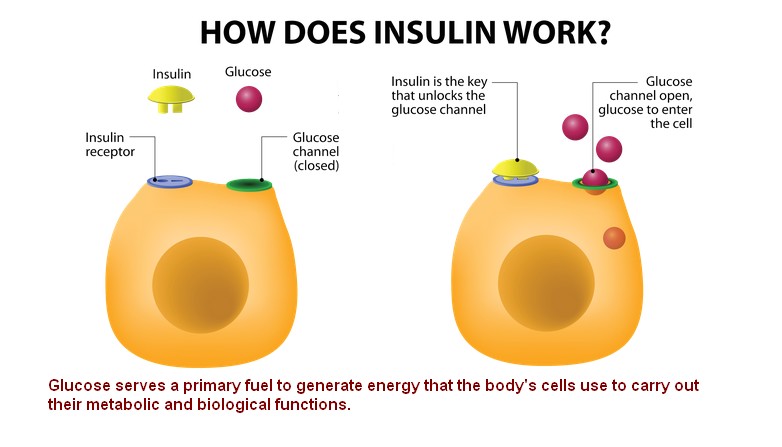
Blood sugar regulation is another process that MG is involved in. Although this author has identified and outlined (in previous articles) that adequate sleep, exercise, and consumption of low glycemic foods facilitate blood sugar regulation, MG also assists by facilitating synthesis of insulin (and insulin receptor sensitivity); an anabolic hormone which facilitates storage/deposition of glucose in cells of the body (primarily adipose tissue, brain, and muscle).2,3 Moreover, MG is involved in bone mineralization, nucleic acid production, platelet activity, hormone receptor binding, calcium regulation, and 300 enzymatic reactions, signifying its near ubiquitous involvement in physiological processes.2(447-448)
If an individual continues to have aberrant HBA1C/FGT markers, this author would suggest screening total plasma/serum MG concentrations to determine its range, and establish a baseline.2(449) If MG levels are below 2.1-2.4 mg/dL, this author would suggest supplementing with MG, such as MG glycinate in the amounts of 300-600 mg/day; a form easily absorbed by the intestines.2(450,451) Furthermore, this author would also monitor symptoms of magnesium deficiency to include: muscle weakness, tremors, headache, mental confusion, and restlessness.2(450) Monitoring said symptoms is especially relevant with H/D individuals as they tend to have increased urinary losses of MG.2(450)
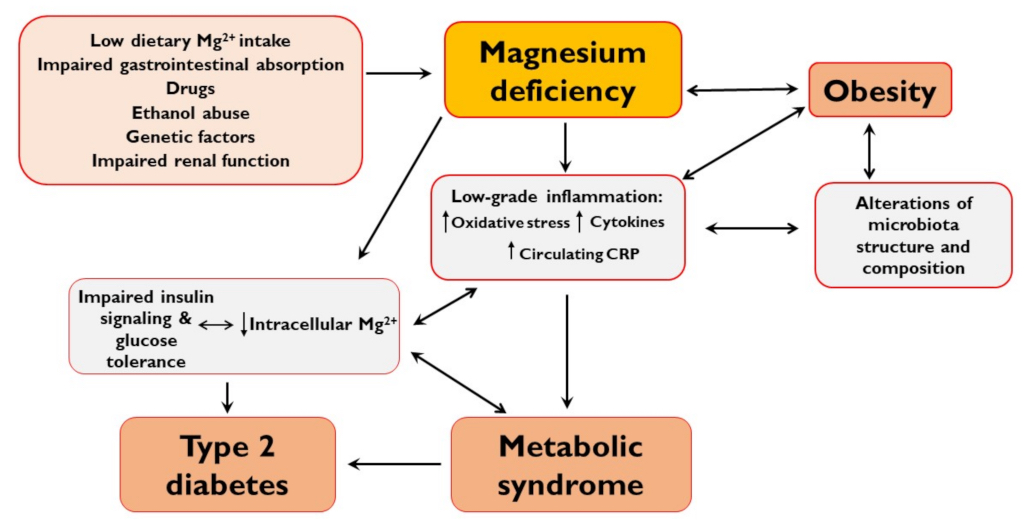
In conclusion, hyperglycemia is a condition whereby glucose is poorly managed and stored throughout cells and tissues of the body. Left unchecked, hyperglycemia can manifest into insulin resistance and type 2 diabetes. Ultimately, early detection, optimal sleep, exercise, and nutritional interventions are paramount in managing hyperglycemia. However, if said interventions do not move H/D biomarkers into optimal ranges, assessment of MG levels may help elucidate another driver behind said conditions. If MG deficiencies are detected despite consumption of MG-rich foods, supplementation is likely to help improve and return blood and cellular MG/glucose levels to optimal ranges.
References
1. Diabetes: Diagnosis and Treatment. Mayo Clinic website. https://www.mayoclinic.org/diseases-conditions/diabetes/diagnosis-treatment/drc-20371451. Updated August 8, 2018. Accessed January 31, 2020.
2. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism. 7th ed. Boston, MA: Cengage Learning; 2018.
3. Zhao B, Deng H, Li B, et al. Association of magnesium consumption with type 2 diabetes and glucose metabolism: A systematic review and pooled study with trial sequential analysis. Diabetes Metab Res Rev. 2019;1-19. doi:10.1002/dmrr.3243.
-Michael McIsaac
