Diabetes mellitus (DM) is a general term used to describe a group of diseases characterized by an aberration in insulin secretion and/or cellular resistance to said hormone. Such discordance between insulin and the cell can drive elevated plasma glucose levels, inhibit proper metabolism of carbohydrates/fats, induce pathologic changes in nerves/small blood vessels, and aggravate atherosclerosis (Lee & Nieman, 2013). Moreover, DM is one of the top 10 leading causes of death in North America; 26 million individuals (8% of population) have diabetes (Lee & Nieman, 2013). Thus, strategies which include early detection and monitoring, are critical first steps in prevention and management of said disease. As a means of appreciating such a process, the following will consider insulin levels and its implications in identifying prediabetes.
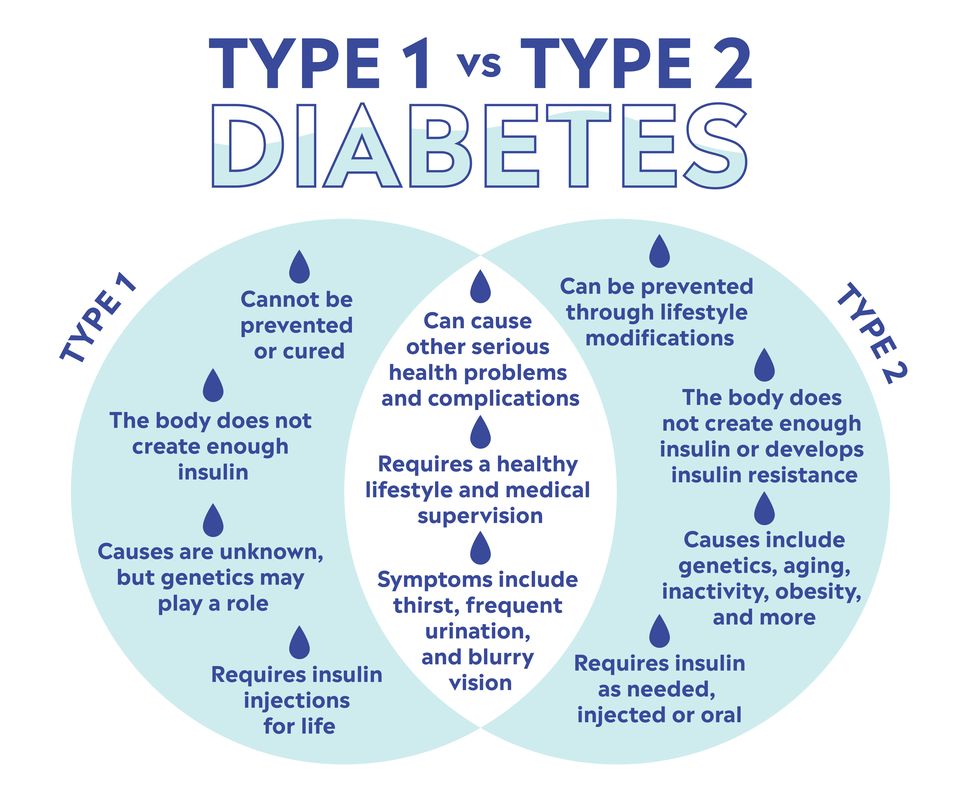
DM can be broken down into 2 main categories; type 1 diabetes (T1D) and type 2 diabetes (T2D). T1D is characterized by an autoimmune reaction whereby beta cells of the pancreas are destroyed over time, eventually disrupting the production and secretion of insulin; a key hormone in regulating blood glucose levels and storage in other tissues (Lee & Nieman, 2013). T2D is characterized not by a lack of insulin production, by rather, by a lack of sensitivity to insulin within target cells and tissues; insulin resistance (IR). Cell membranes tend to express less insulin receptors and/or the ability to transport and metabolize glucose into the cell (Lee & Nieman, 2013).
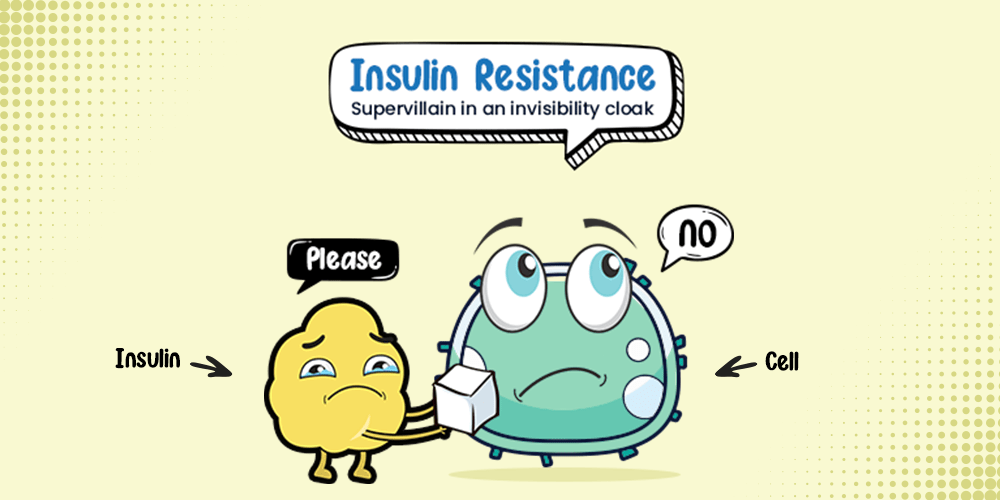
Although it is desirable to maintain optimal glucose levels in the blood to avoid hyperglycemia and hypoglycemia, monitoring glucose levels alone might not reveal all biomarkers relevant to assessing health status of an individual. In T2D, more insulin is required to maintain optimal glucose levels (<97mg/dL) (Lee & Nieman, 2013). Initially, glucose levels might be kept in said optimal ranges. However, as time passes, higher amounts of insulin production (hyperinsulinemia) and secretion are required to keep individuals out of hyperglycemia (“Diagnosis and Classification” 2012).
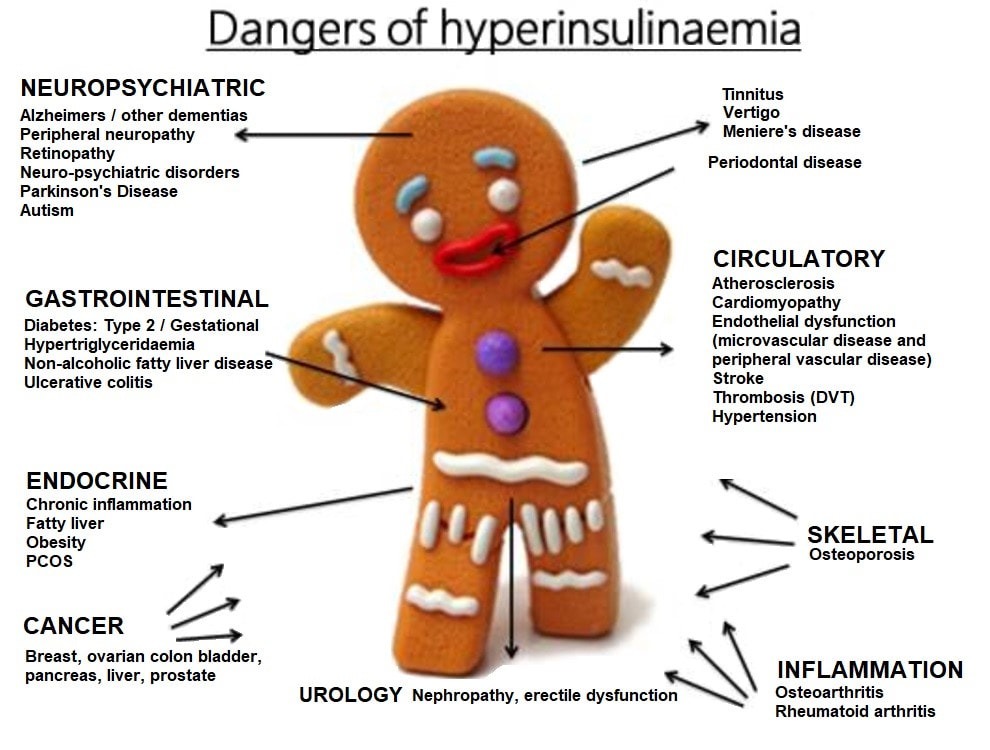
Over time, the pancreas becomes unable to provide enough insulin to resistant cells and tissues, making T2D progression slow and insidious (“Diagnosis and Classification” 2012). Progression of the disease is overlooked/missed if one only considers and monitors glucose, which necessitates the requirement to track insulin secretion in the presence of normal/rising blood glucose levels. Such increases of insulin production are associated with many diseases and contributes to weight gain; insulin drives glucose into fat cells (triglycerides), prevents fats from contributing to energy production, and induces hunger (Faloon, 2013). In effect, a vicious cycle of fat storage, excessive hunger, and weight gain ensues; a prominent (though not complete) set of characteristics of individuals with pre-diabetes/diabetes (Faloon, 2013).

Typically, one unit of insulin released from the pancreas will facilitate movement of 10 mg of glucose into a cell. As previously mentioned, in the presence of IR, more insulin is required to manage glucose (hyperinsulinemia). Such unusually high concentrations of insulin in the bloodstream from IR are also associated with a cluster of diseases: atherosclerosis, hypertension, chronic inflammation, low high-density lipoproteins (HDLs), elevated triglycerides, obesity, and cancer (Faloon, 2013). In essence, tracking insulin levels is as pertinent as monitoring glucose levels and hemoglobin a1c; the average glucose level over the lifespan of a red blood cell (~3 months).
One test to monitor and track hyperinsulinemia is through the insulin assay (Pagna & Pagna, 2014). Such a test is useful as it can evaluate abnormal lipid and carbohydrate metabolism. The assay can help indicate excess insulin production by comparing insulin response to a glucose load, called an oral glucose tolerance test (OGTT) (Pagna & Pagna, 2014). Normal fasting insulin ranges for adults would be 6-26 µU/ml. See below chart for normal insulin levels after an OGTT:
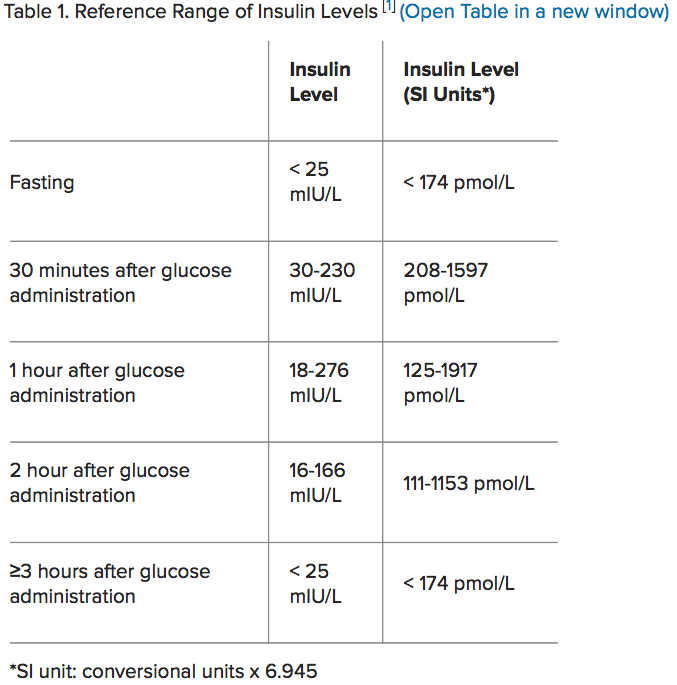
(Medscape, 2014)
If an unusually high insulin spike is present during the glucose tolerance test, such a marker can help individuals take preventative action before the onset of full blown T2D. In addition, other risk factors, in conjunction to insulin monitoring, can help individuals prepare interventions to assist in managing hyperglycemia/hyperinsulinemia:
| Overweight (BMI ≥ 25 kg/m2) | Hypertension (≥140/90 mm Hg adults) |
| Age ≥ 45 | HDL <35mg/dL and triglycerides >250 mg/dL |
| Parent or sibling with diabetes | Polycystic ovary syndrome |
| Inactivity | History of cardiovascular disease |
| Of African/Latino/Asian/Native American/ Pacific Islander race | |
| Previous impaired fasting glucose or impaired glucose tolerance test | |
| HbA1c ≥ 5.7% | |
| History of gestational diabetes |
(Lee & Nieman, 2013)
In conclusion, prediabetes and diabetes can be tracked by assessing glucose levels in the blood. However, as evidenced, such biomarkers may not be very telling of the overexpression of insulin (which can precede hyperglycemia), which is related to a myriad of disease states. By monitoring insulin levels, in conjunction to glucose and other risk factors, individuals are presented with an opportunity to begin circumventing/managing the health consequences of pre-diabetes and diabetes.
References
Diagnosis and classification of diabetes mellitus (2012). American Diabetes Association, 35(1), 564-571.
Faloon, W. (2013). Blood levels of insulin and hemoglobin a1c in foundation members. Retrieved from http://lifeextension.com/magazine/2013/7/blood-levels-of-insulin-and-hemoglobin-a1c-in-foundation-members/page-01
Lee, R. D., & Nieman, D. C. (2013). Nutritional assessment (6thed.). New York, NY: McGraw-Hill.
Medscape (2014). Insulin. Retrieved from https://emedicine.medscape.com/article/2089224-overview
Pagana, K. D., & Pagana, T. J. (2014). Manual of diagnostic and laboratory tests (5thed.). St. Louis, MO: Mosby.
-Michael McIsaac
