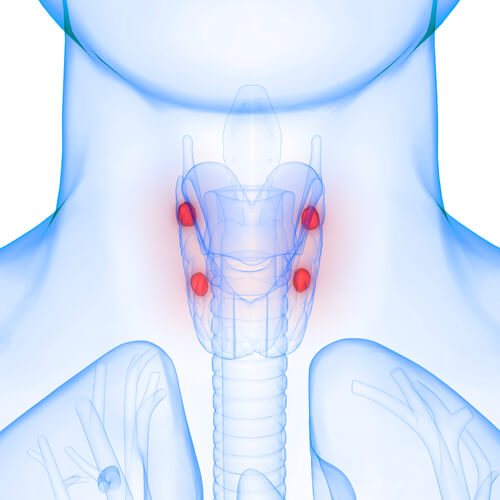
Primary hyperparathyroidism (PHPT) is a common aberration in endocrine function, which negatively impacts calcium homeostasis.1 Due to its commonality, approximately 20-30 new cases, per year, are identified for every 100,000 people in the United States.1(564) Furthermore, PHPT is the leading cause of chronic hypercalcemia and has long term negative effects upon bone, cardiovascular, kidney health, and nephrolithiasis.1(564) As such, it is imperative to identify biomarkers and risk factors which indicate the manifestation of PHPT and kidney stones.
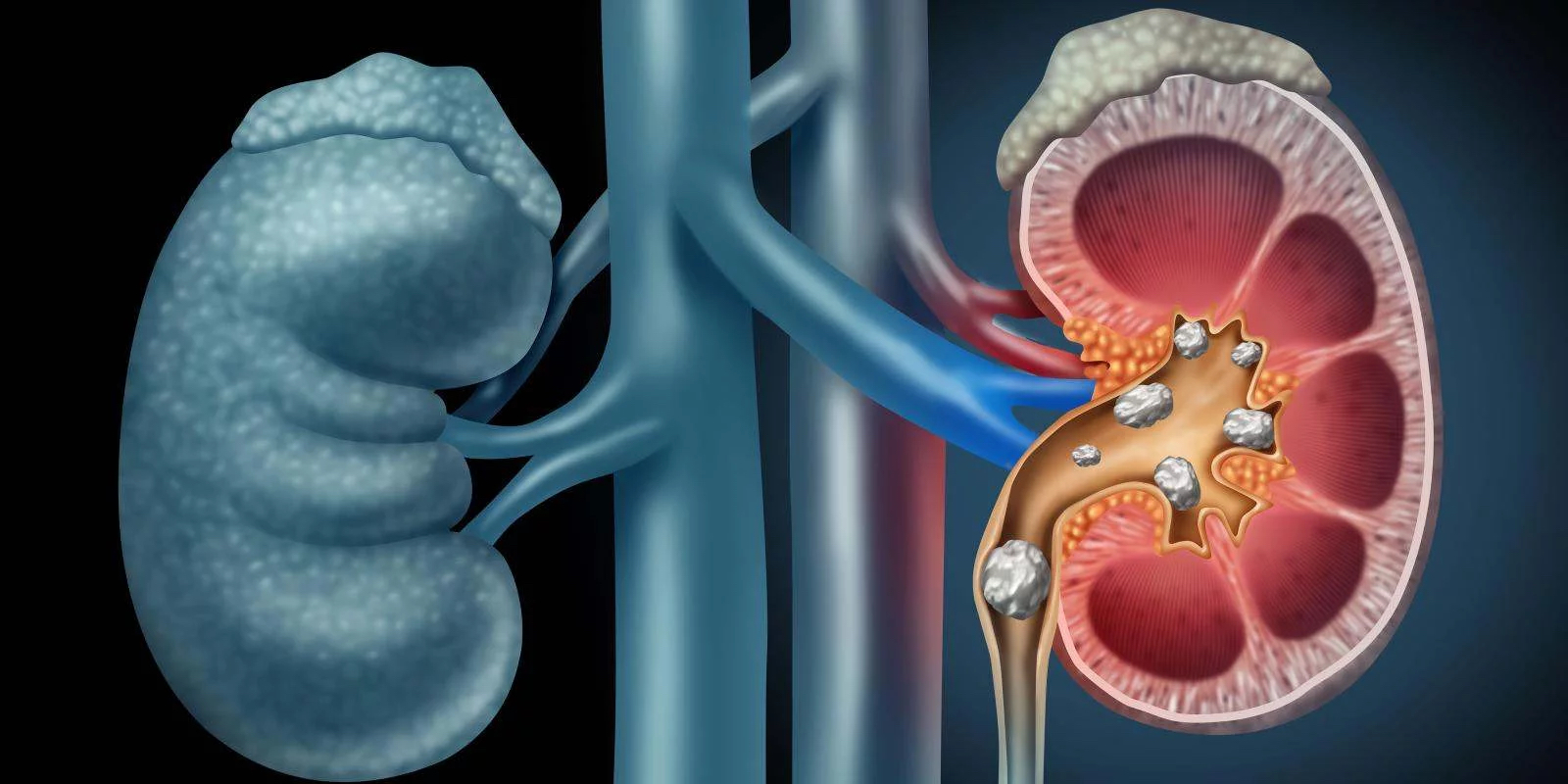
Perez et al1(564) indicated that detection and timely treatment is essential in preventing kidney stones. Otherwise, late detection is likely to necessitate surgical interventions as the only definitive treatment.1(564) As mentioned previously, uncontrolled PHPT can pose considerable risk of not only recurrent stone disease and hypercalcemic crisis but also hypertension, stroke, diabetes, heart failure, depression, cognitive impairment, and suicidal ideation.1(565) Ultimately, early detection is critical.

As a means of attempting to identify predictors of kidney stone formation and finding a means of effectively diagnosing PHPT, Perez et al1(565) performed a single-institution, retrospective analysis of PHPT patients who underwent parathyroid surgery. Furthermore, the researchers compared 246 patients who had a history of kidney stone formation to 1047 patients who did not produce stones.1(565) Of the 246 stone formers, 51 patients were identified as having clinical presentations of PHPT via calcium-containing kidney stones.1(565) Parathyroid hormone levels and calcium labs were also considered within said group.

Perez et al1(567) found associations which indicated that stone formers were more likely to be male and have higher urinary calcium excretion, while male sex was independently associated with stone formation. Other useful data included associations between stone formers and the degree of parathyroid hormone, calcium mobilization, and calcium excretion.1(567) Other markers of stone formers included high alkaline phosphatase, indicating a greater rate of bone turnover, and a potentially greater phenotype of parathyroid disease.1(567) Though such markers were found, the researchers cautioned that the presence of said markers did not help predict which PHPT patients would produce stones.1(568)

In conclusion, PHPT has an association to kidney stones. However, elevated markers (serum chemistries and /or urinary calcium levels) do not necessarily identify the majority of patients at risk of stone formation.1(568) Despite such limitations, the research of Perez et al1(568) did provide useful insights; if PHPT is considered early during the presentation of kidney stones, time to a definitive treatment can be dramatically reduced by more than 3 years.1(568)Furthermore, such an approach would not only help prevent recurrent stone disease and hypercalcemic crisis, but also hypertension, stroke, diabetes, heart failure, depression, cognitive impairment, and suicidal ideation.1(565)
References
1. Perez AA, Schneider DF, Long KL, et al. Timely evaluation and management of primary hyperparathyroidism in patients with kidney stones. J Surg Res. 2018;232:564-569. doi: 10.1016/j.jss.2018.07.028.
-Michael McIsaac