
Hypertension, defined as resting blood pressure of ≥140/90,impacts over 29% of the adult American population and is a leading cause of renal disease, heart attack, and stroke (Gropper, Smith, and Carr, 2018). Sodium (Na) was one of the first micronutrients mechanistically linked with hypertension, and has since become a commonly understood factor in risk and cause of high blood pressure (Gropper et al., 2018). However, evidence has indicated biochemical and physiological nuances between Na and other micronutrients that also affect blood pressure. Two such nutrients are, but not limited to, magnesium (Mg) and potassium (K). As such, the following will consider the influence of said micronutrients upon blood pressure and ultimately, hypertension.

Research was conducted exploring the cardiac effects of 3 levels of sodium intake: 3.3 g, 2.4 g (adequate intake), and 1.5 g (Bray, Vollmer, Sacks, Obarzanek, Svetkey, & Appel, 2004). 412 participants were randomly assigned to either a Dietary Approaches to Stop Hypertension (DASH), or a standard American Diet (SAD) (Bray et al., 2004). While consuming said diets, each participant was randomly assigned to each sodium load for one month until all 3 sodium loads were completed. Blood pressure was recorded before, during, and after the experiment (Bray et al., 2004). The following sections will consider the results from Bray et al. (2004).

Evidence suggested that lower sodium loads (i.e., 1.5 g/day) yielded the lowest (statistically significant) blood pressure readings when compared to intermediate (2.4 g/day) and highest (3.3 g/day) loads (Bray et al., 2004). Additionally, such changes were most evident among individuals who were hypertensive prior to the experiment and among those moving from 2.4 g/day to 1.5 g/day as opposed to blood pressure readings from participants shifting from Na intake of 3.5 g/day to 2.4 g/day (Bray et al., 2004). Although the research of Bray et al. (2004) supported the recommendations of adequate intakes of 2.4 g/day (perhaps less), Mg and K are also intimately involved in blood pressure regulation. As such, the following will consider Mg and K in greater detail.
Mg is a mineral considered essential to the human body and participates in such processes as calcium regulation, hormone receptor binding, enzymatic reactions, bone mineralization, and cell membrane ion transfer (Grooper et al., 2018). Researchers have postulated that Mg might exert its blood pressure-lowering effects via prostacyclin and nitrox oxide (both are vasodilators) formation affecting endothelium-dependant and endothelium-independent vasodilation (Xhang et al., 2016). As such, Zhang et al. (2016) performed a meta-analysis examining 34 double-blind placebo-controlled trials in which a total of 2028 individuals participated.

The analysis concluded that Mg supplementation elucidated a significant reduction in systolic and diastolic blood pressure (an average reduction of 2.00 / 1.78 mm Hg, respectively) (Xhang et al., 2016). One limitation, however, of said analysis was that only 2 of 34 trials included individuals with deficient Mg levels. It is possible that Mg supplementation might have had more robust changes if more participants were deficient. Despite limitations in analysis of populations with high blood pressure who are also deficient in Mg, research has indicated that a 2 mm Hg reduction in blood pressure reduces mortality secondary to stroke by 6% and secondary to heart disease by 4% (Grooper et al., 2018).
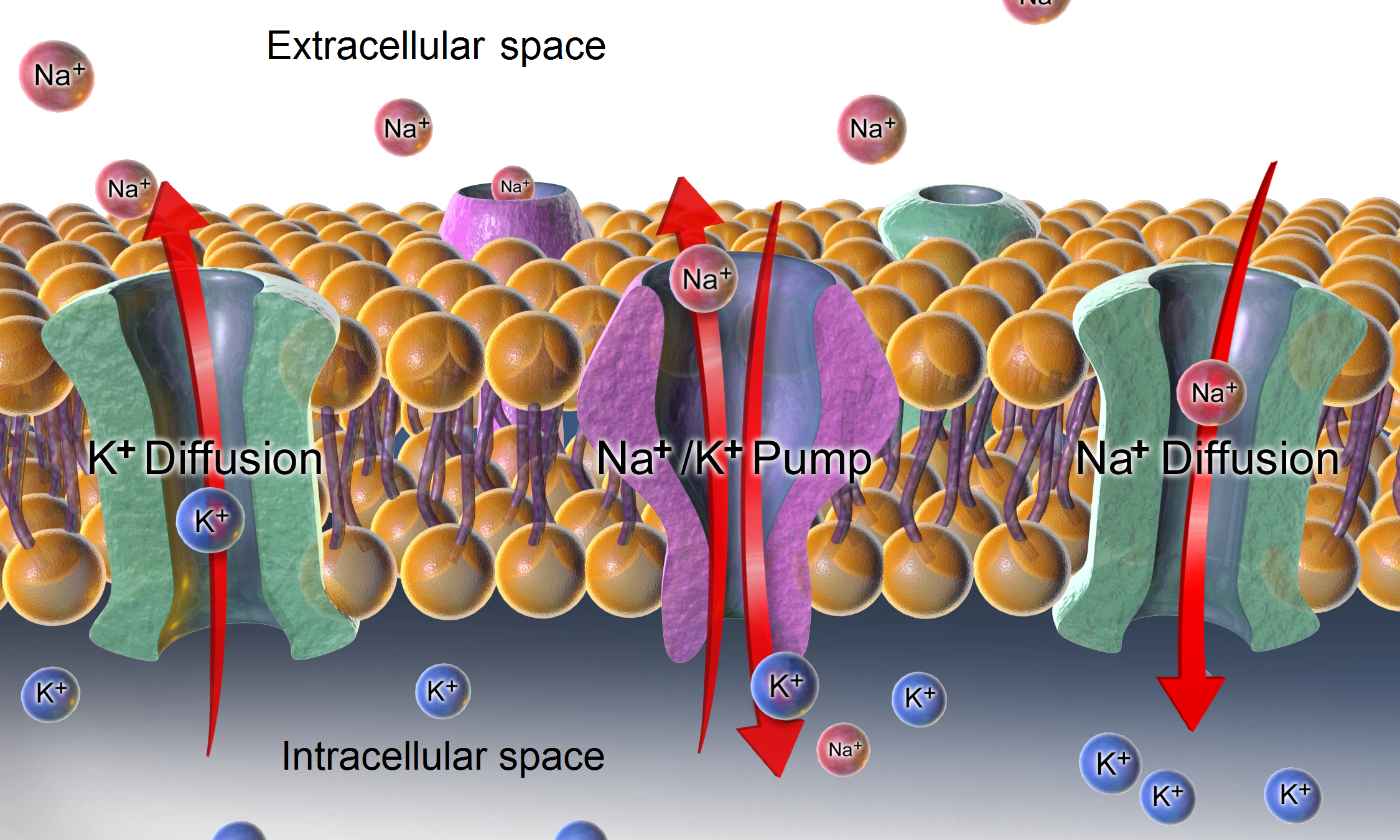
As outlined in this author’s previous posts, K has been associated with increased blood pressure/hypertension, especially when higher dietary intake of Na is occurring (Gropper et al., 2018). K regulates blood pressure upon cardiac muscle via nerve conduction. Specifically, K exerts its influence upon the resting membrane potential of cardiac cells and directly affects the contractility and depolarization of the heart (Gropper et al., 2018). Thus, adequate levels of K can help reduce blood pressure. Furthermore, K also influences blood pressure by modulating blood volume in the body. Such is achieved via interaction with Na; if Na is above recommended levels of 2.4 g/day, the kidneys increase excretion rates to control Na levels. However, K is also excreted in the process. To maintain K concentrations, the kidneys hold back fluids. However, a side-affect is increased blood volume and, hence, increased blood pressure (Grooper et al., 2018).
In conclusion, Na, Mg, and K are electrolytes that have effects on the physiology and function of the cardiac tissue to include regulating blood pressure. Most relevantly, evidence has indicated that although each aforementioned micronutrient can influence the heart singularly, they also have influences upon each other. Awareness of such symbiosis should encourage nutritionists to consider each micronutrient individually, and as a whole, when developing interventions to reduce blood pressure and risk of cardiovascular disease.
References
Bray, G. A., Vollmer, W. M., Sacks, F. M., Obarzanek, E., Svetkey, L. P., & Appel, L. J. (2004). A further subgroup analysis of the effects of the DASH diet and three dietary sodium levels on blood pressure: Results of the dash-sodium trial. The American Journal of Cardiology, 94, 222-227.
Gropper, S. S., Smith, J. L., & Carr, T. P. (2018). Advanced nutrition and human metabolism (7thed.). Boston, MA: Cengage Learning.
Zhang, X., Yufeng, L., Del Gobbo, L. C., Rosanoff, A., Wang, J., Zhang, W., & Song, Y. (2016). Effects of magnesium supplementation on blood pressure a meta-analysis of randomized double-blind placebo-controlled trials.Hypertension, 68(2), 324-333.
-Michael McIsaac
