
In this author’s last post, prostate cancer (PC) growth and proliferation was explored as well as its relationship to low vitamin D (measured as 25-hydroxyvitamin D, or 25OHD) levels. In the following sections, this author would like to continue elucidating other conditions and mechanisms behind malignant tumor growth within the prostate, to include hypogonadism; a disease characterized by low testosterone levels.1 As such, the following will explore hypogonadism in greater detail, its relationship to PC, and solutions to mitigate low testosterone.
Hypogonadism can be defined as a syndrome characterized by androgen deficiency classified as primary or secondary according to the genesis of testosterone deficiency.2 Primary hypogonadism emanates from an inability of the testicles to secrete testosterone in amounts required to maintain normal physiological circulating concentrations, while secondary hypogonadism is from reduced or inappropriately normal gonadotropin release and subsequent disruption of hypothalamic‐pituitary‐testicular (HPT) axis normal functioning.2(1149)

The hypothalamus is responsible for releasing hypothalamic gonadotropin-releasing hormone (GNRH), through the hypothalamic-pituitary portal which stimulates gonadotropins, follicle stimulating hormone (FSH) and luteinizing hormone (LH).2(1149) Once the testes are stimulated by GNRH, testosterone enters the bloodstream mostly bound (i.e., up to 44%-65%) to sex hormone binding globulin (SHBG), while a smaller portion travels free from SHBG, otherwise known as bioavailable testosterone; forms include free testosterone (i.e., 2%-3%) and testosterone + albumin (33-54%).2(1149)3,4
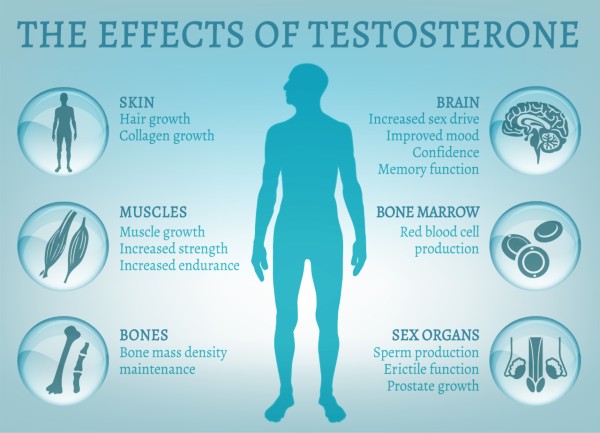
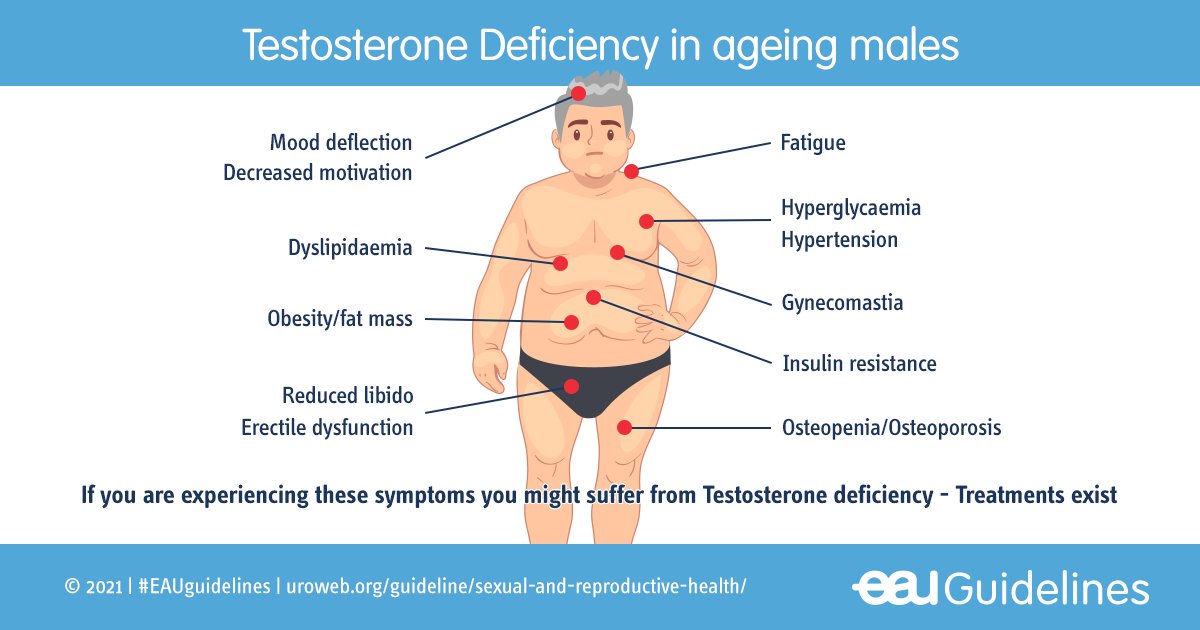
In addition to signs of hypogonadism/low testosterone in the previous section, symptoms include low libido, erectile dysfunction, loss of body hair, hot flashes, insomnia, poor memory, decreased energy, decreased physical performance, depression, increased bodyfat, and increased muscle loss.3 Thus, hypogonadism exhibits a wide range of both biomarkers and symptoms and can be defined as total testosterone < 300 ng/dL, with a corresponding bioavailable testosterone level of < 80 ng/dL.1(37)

Such knowledge of symptoms and testosterone levels is highly relevant because there is growing evidence that testosterone deficiency is independently associated with higher tumor aggressiveness.1(42) Knowledge of testosterone levels and its relationship to PC might serve as an early warning amongst hypogonadal males; such awareness of symptoms and signs could serve as an impetus to not only monitor the prostate, but also develop strategies to improve testosterone levels.
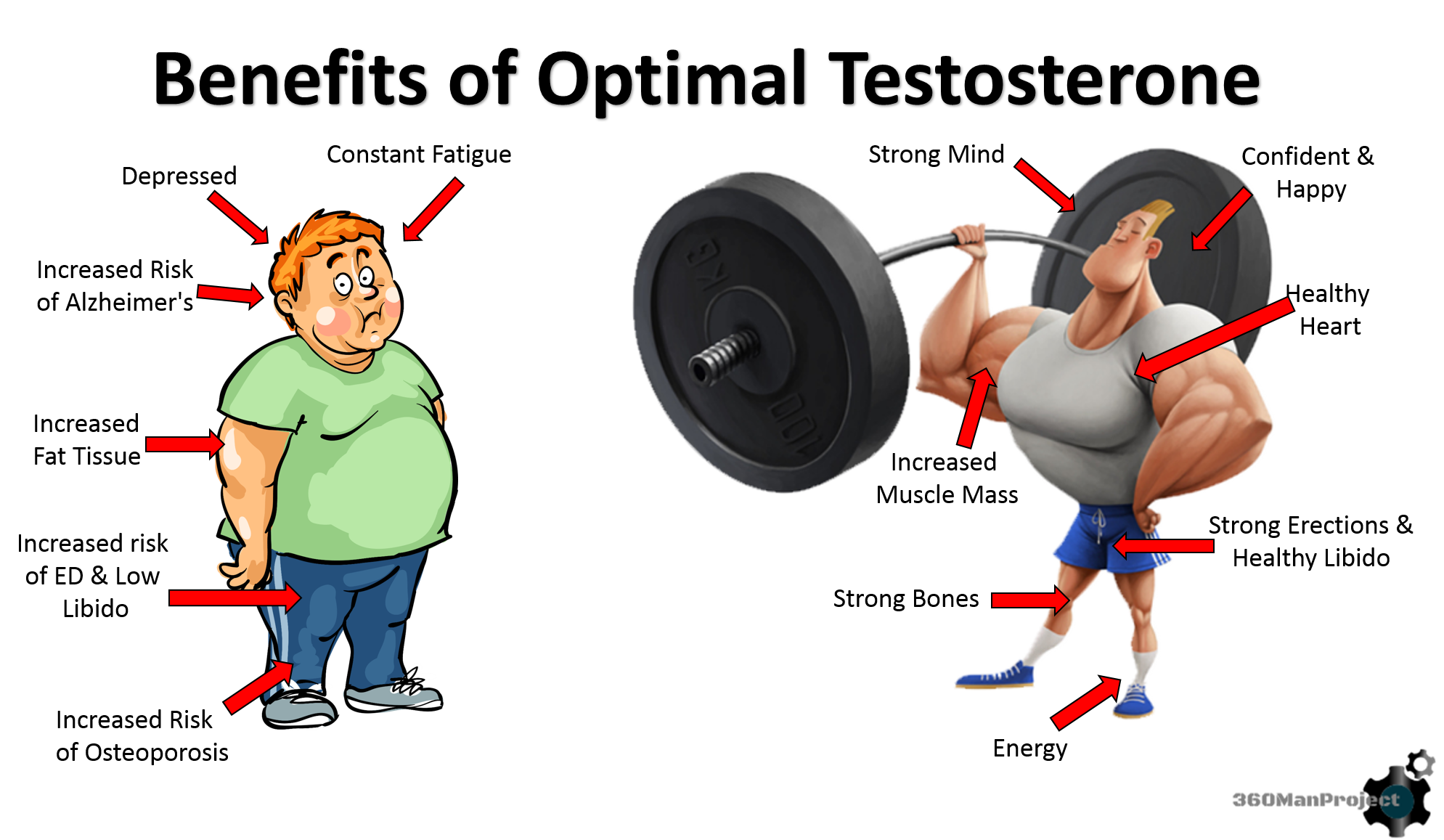
There exists a degree of concern regarding increasing testosterone concentrations with some researchers citing the possibility of worsening cancer risk and progression.4(574) However, Lord and Bralley4(574) stated that cancer risk increases when testosterone falls out of normal ranges; too high and too little testosterone has been implicated in cancer risk and progression.4(574) Thus, the goal is to restore optimal ranges of testosterone, defined by Harvard Health Publishing5 as:
| Age | Total testosterone (ng/dL) | Free testosterone (ng/dL) | Bioavailable testosterone (ng/dL) |
| 40–49 | 252–916 | 5.3–26.3 | 101–499 |
| 50–59 | 215–878 | 4.2–22.2 | 80–420 |
| 60–69 | 196–859 | 3.7–18.9 | 69–356 |
| 70–79 | 156–819 | 2.2–14.7 | 41–279 |
Nutritional interventions to improve testosterone levels includes a wide array of amino acids, which can be derived from meats, pork, poultry, and dairy.4(574) Additionally, ensuring optimal levels of zinc is paramount as deficiencies can cause several maladies such as increased risk of infections, infertility, impaired brain development, alopecia, dermatitis, impaired smell/taste, and low testosterone.6 Furthermore, zinc has been shown to contribute to male reproduction processes to include testicular development, sperm quality, in addition to improving testosterone levels.7 Rich sources of zinc include red meats (organ meats), seafood (oysters), pork, and dairy.8
In conclusion, PC is the most common malignancy found among males, worldwide, and has strong associations with hypogonadism. Awareness, and close monitoring, of signs and symptoms of PC should serve as a vital first step in managing said condition, followed by steps to help move testosterone levels into normal ranges depending on age bracket. Implementation of dietary interventions, which increase amino acids and zinc levels (in addition to vitamin D covered in this author’s previous post), could help hypogonadal males improve testosterone levels. Ultimately, such steps could serve as an adjunct when treating PC, as well as a preventative measure amongst individuals showing early signs of tumor growth.
References
1. Neuzillet Y, Raynaud JP, Dreyfus JF, et al. Aggressiveness of localized prostate cancer: The key value of testosterone deficiency evaluated by both total and bioavailable testosterone: Androcan study results. Horm Can. 2019;10:36-44. doi:https://doi.org/10.1007/s12672-018-0351-8.
2. Carrageta DF, Oliveria PF, Alves MG, et al. Obesity and male hypogonadism: Tales of a vicious cycle. Obes Rev. 2019;20:1148–1158. doi:10.1111/obr.12863.
3. Harvard Health Publishing. Testing Your Testosterone: It’s Tricky. https://www.health.harvard.edu/mens-health/testing-your-testosterone-its-tricky. Published October, 2012. Accessed November 10, 2019
4. Lord RS, Bralley, JA. Laboratory Evaluations for Integrative and Functional Medicine. 2 nd ed. Duluth, GA: Genova Diagnostics; 2012.
5. Harvard Health Publishing. Testosterone, Aging, and the Mind. https://www.health.harvard.edu/newsletter_article/Testosterone_aging_and_the_mind. Published January, 2008. Accessed November 10, 2019.
6. Crook MA. Zinc deficiency. Nutr. 2011;27(10):1085-1086. doi:10.1016/j.nut.2011.06.001.
7. Liu YL, Zhang MN, Tong GY, et al. The effectiveness of zinc supplementation in men with isolated hypogonadotropic hypogonadism. Asian J Andro. 2017:19(3):280-285. doi:10.4103/1008-682X.189621.
8. Gropper SS, Smith JL, Carr TP. Advanced Nutrition and Human Metabolism. 7 th ed. Boston, MA: Cengage Learning; 2018.
-Michael McIsaac
