The origin of inflammatory bowel disease (IBD) remains largely unelucidated, although multiple factors are involved inducing to an array of intestinal and extra-intestinal consequences, to include nutrient maldigestion/malabsorption.1 As such, it is imperative to identify and control underlying drivers of IBD in addition to managing symptoms of the same. One solution, as part of a larger and more robust intervention, can include omega-3 fatty acid (O3FA) supplementation. As a means of appreciating IBD management and remission, the following will consider said condition in greater detail, its relationship to fish oil, and mitigation of inflammatory markers.
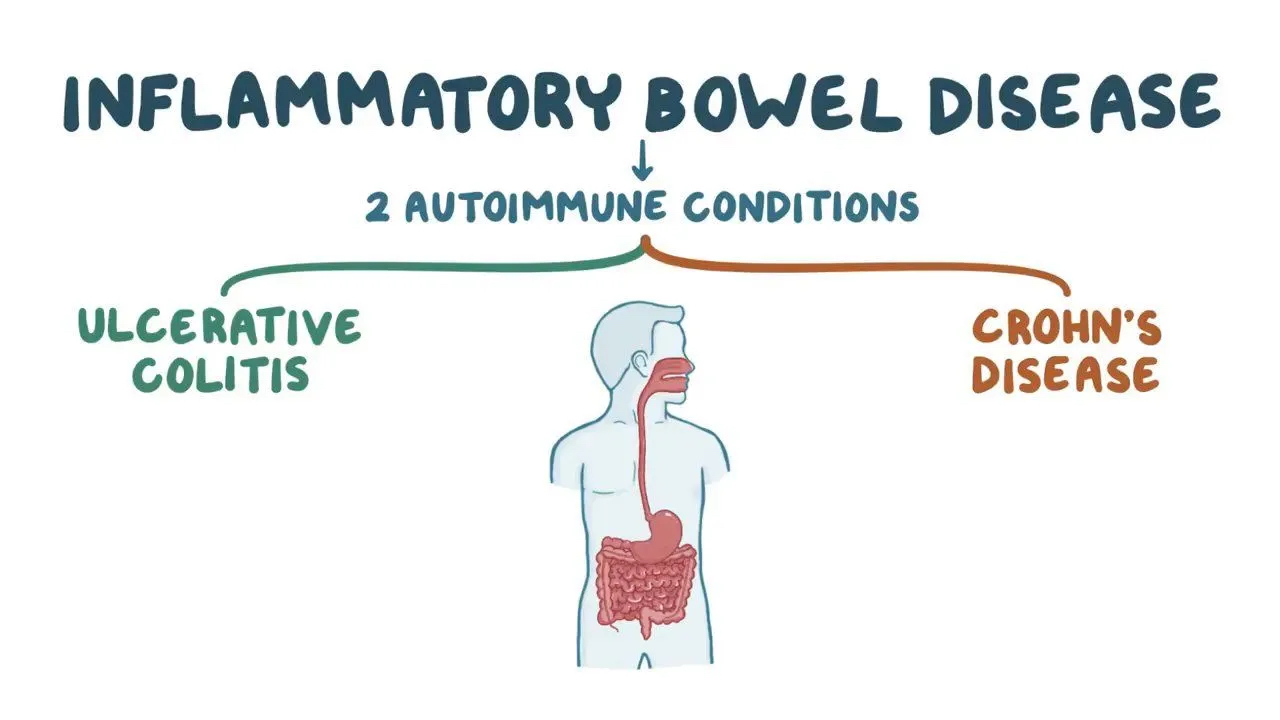
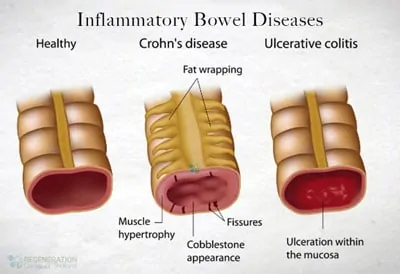
Karavasili et al1(1256) sub-classified IBD into two main diseases; Crohn’ s disease (CD) and ulcerative colitis (UC), while indicating that cases existed whereby individuals could share clinical/radiological/histological traits of both conditions. Multiple factors, as mentioned in the previous section, have been thought to contribute to IBD including genetic, environmental, immunological, and microbial influences. Of particular interest is the immunological element of IBD and its downstream cascade of inflammatory events along the gastrointestinal tract. The following will consider the immune response and its relationship to O3FAs in greater detail.
Marton et al2 indicated that the immune system plays a vital role against infectious and inflammatory processes; such is achieved by removing damage to tissues, or reducing and extinguishing the stimuli. Therefore, dysregulation of said system has been associated with several disorders such as cardiovascular disease, rheumatoid arthritis, cancer, and IBD.2(1)IBD is also chronic, relapsing, debilitating, and inflammatory in nature. Furthermore, an excess of 75,000 people are thought to be effected in Australia, 2.5 million in Europe, and 3 million people in the Unites States.2(1)
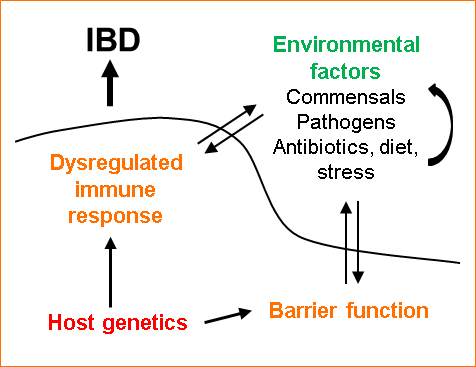
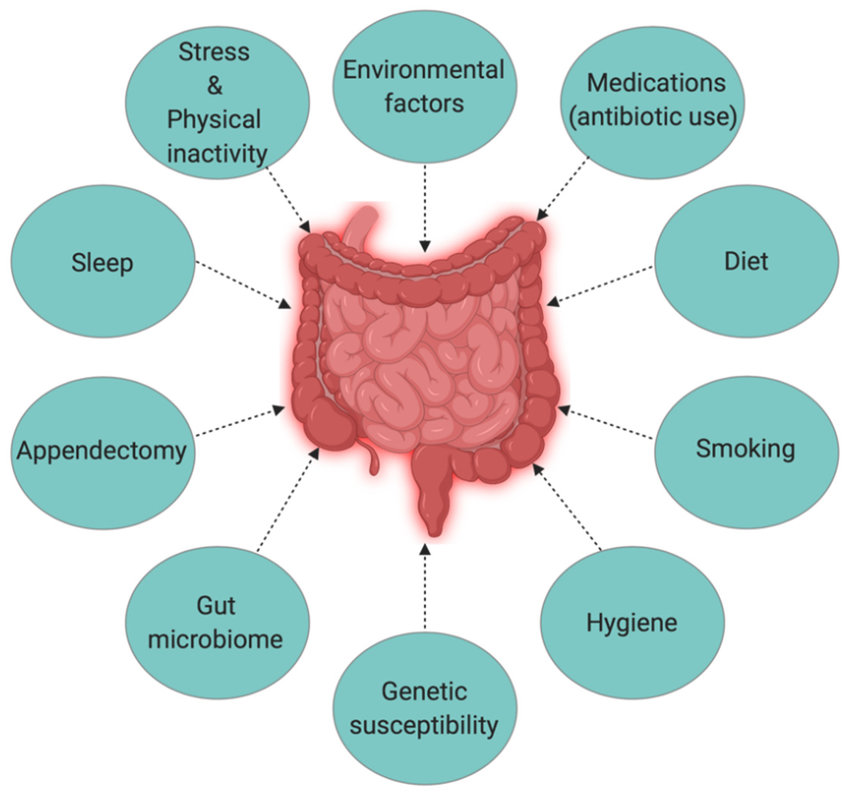
Such inflammatory conditions occur from an imbalance between environmental/microbial conditions and the intestinal immune response, inducing an aberration between anti-inflammatory and pro-inflammatory molecules, in addition to other factors thought to be involved in the chronic inflammatory state of IBS.2(1) Said factors include the intestinal microbiota itself, oxylipins (metabolites of polyunsaturated fatty acids), free radicals, nitric oxide (NO), activated toll-like receptors (TLR), interleukins (ILs), and cytokines.2(1) Considering the chronic nature of IBD and dysregulated inflammatory responses found therein, IBD necessitates interventions that are both cost-effective and simple in nature.
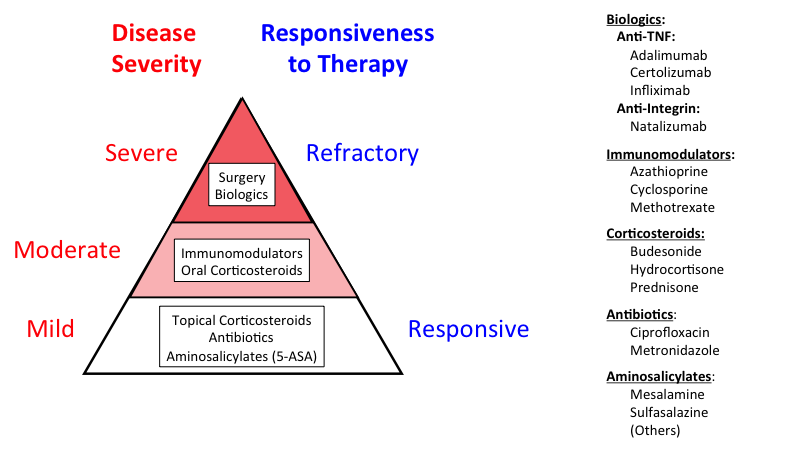
The current treatment of IBS includes symptom management using biological agents, antibiotics, corticosteroids, and immunosuppressants.2(2) However, said medications, according to Marton et al,2(2) may not induce remission and have also been related to many unfavorable side effects. The researchers considered the implications of O3FAS upon markers of inflammation by reviewing the findings of: two prospective cohort studies, two clinical trials, one pilot study, five case-controls, four randomized controlled clinical trials, and one randomized clinical trial. The studies included 334 individuals with CD, 488 with UC, and 367 in controls for a total of 1189 patients.2(2) Please see findings:
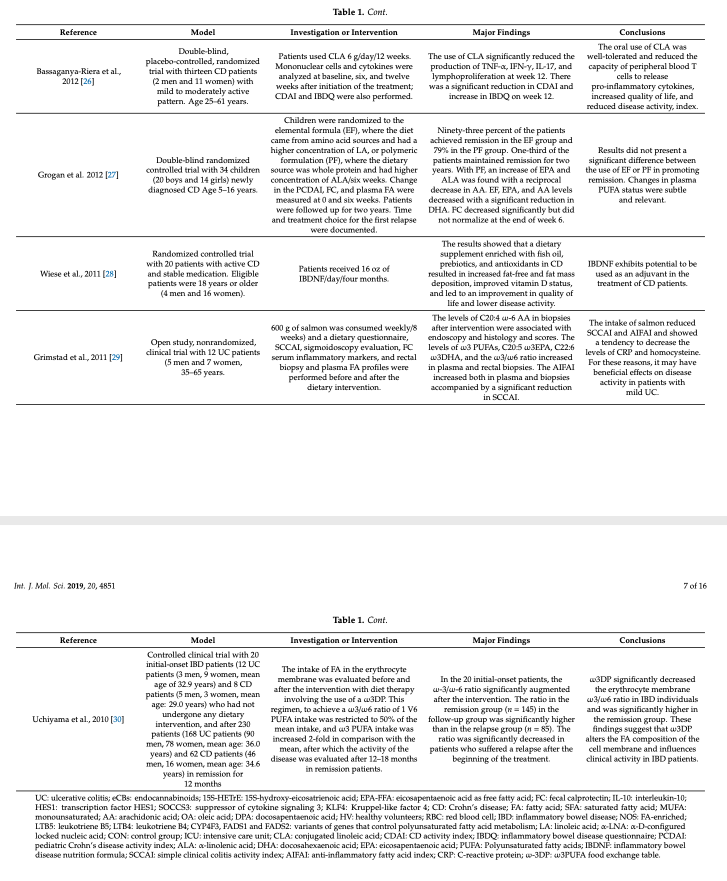
Results from O3FA supplementation generally suggested an improved overall quality of life amongst UC and CD, an increased ability to maintain remission status, reductions in inflammatory markers, and a possible decreased risk of developing IBD.2(16) Although findings are promising, cautious optimism should be employed due to the variability of sample sizes, O3FA doses, methods of delivery, and biases found within different clinical trials.2(13) Notwithstanding said limitations, O3FAs serve a myriad of physiological roles in the body covered in this author’s previous posts, which builds an argument for their inclusion despite the magnitude of effect upon IBD.

The origin of IBD remains largely unelucidated, although multiple factors are involved inducing to an array of intestinal and extra-intestinal consequences, to include nutrient maldigestion/malabsorption. Since IBD is chronic, relapsing, debilitating, and inflammatory in nature, it is essential to employ strategies which minimize immunological triggers as well as the downstream inflammatory consequences that inevitably manifest. O3FAs are likely to play a role as part of a larger, and more inclusive, intervention.
References
1. Karavasili NT, Saridi M, Skamnelos A, et al. Inflammatory bowel disease and infectious factors. J Caring Sci. 2019;12(2):1255-1260.
2. Marton LT, Goulart RDA, Carvalho ACAD, et al. Omega fatty acids and inflammatory bowel diseases: An overview. Int J Mol Sci. 2019:20(19);1-16. doi: https://doi.org/10.3390/ijms20194851.
-Michael McIsaac
