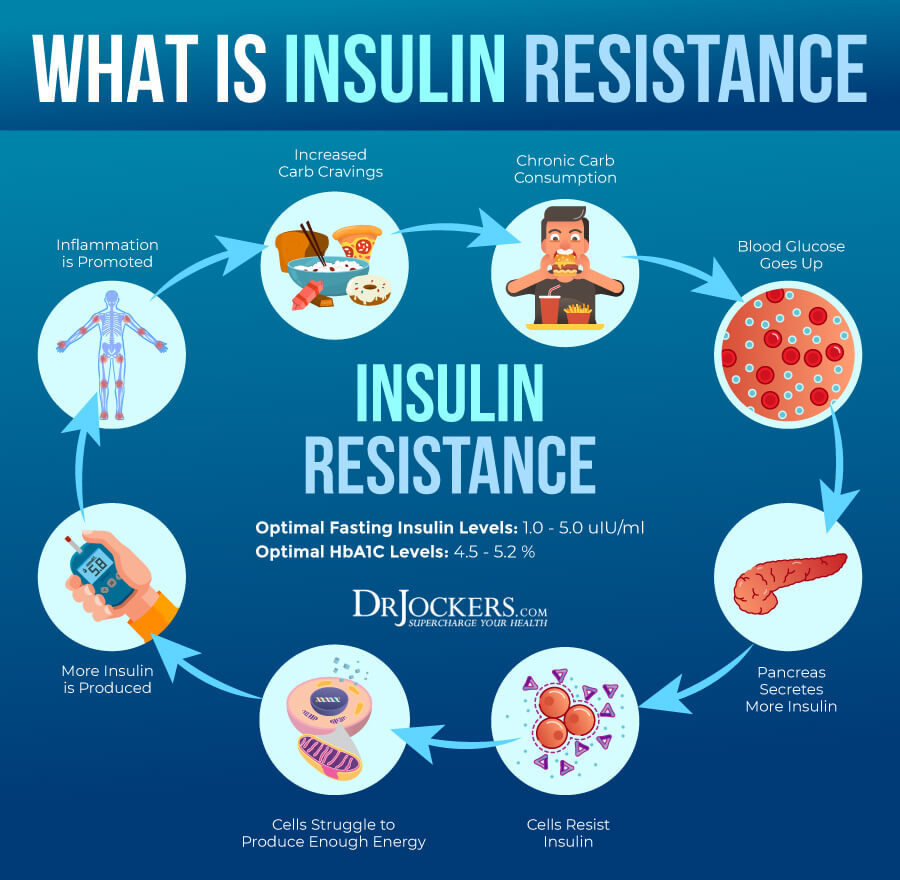
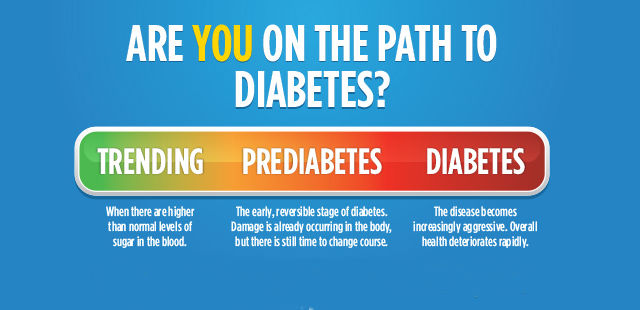
Insulin resistance (IR) can be thought of as an early biomarker in the development type 2 diabetes (T2D). Such a condition presents as higher than normal levels of insulin required to dispose of blood glucose (Lord & Bralley, 2012). Generally, if fasting serum insulin levels are above 10IU/mL, such a condition may indicate the beginnings of IR. Additional tests, like the 2-hour glucose tolerance (GTT) test, can also help determine the presence/beginnings of hyperglycemia; another characteristic/early sign of T2D (Lord & Bralley, 2012).
Ultimately, the presence of high fasting insulin and poor outcomes on the GTT indicates physiological challenges in managing blood glucose levels. Emerging evidence, however, suggests that macronutrient modifications can help improve and/or manage IR. One such intervention is the implementation of very low carbohydrate diets (VLCDs). As a means of appreciating said dietary intervention, the following will consider evidence behind such an approach.

Feinman et al. (2015) stated that current dietary approaches, to include low fat diets, have not been effective in treating IR. Furthermore, the researchers stated that when also considering side effects of some drugs to manage IR/T2D, a novel intervention was necessary to circumvent the inadequacy of the aforementioned protocols. Feinman et al. (2015) posited that VLCDs may provide a viable alternative to individuals suffering from poor carbohydrate metabolism. The following sections will consider 12 points of evidence in using VLCDs, in conjunction to pharmacological approaches for T2D.
- Feinman et al. (2015) stated that hyperglycemia is the most prominent characteristic of T2D, and VLCDs have the greatest effect on reducing blood glucose levels, without the action of insulin. Furthermore, restricted carbohydrate intake reduces postprandial and overall blood glucose concentrations, as well as reducing hemoglobin A1C; a marker of glucose levels over 3 months (Feinman et al., 2015).
- Obesity and T2D epidemics have been largely due to overconsumption of carbohydrates (Feinman et al., 2015). Such data was derived from the National Health and Nutrition Examination Surveys (NHANES), which indicated a dramatic increase in caloric consumption mainly from carbohydrate sources between 1974-2000. Furthermore, the incidence of T2D also rose during said period (Feinman et al., 2015).
- Benefits of carbohydrate restriction does not require the need for weight loss (Feinman et al., 2015). Such results were obtained by monitoring individuals who reduced carbohydrate load (20% of total calories from carbs) without losing weight. Said individuals still received improvements in glycemic control though weight was maintained Feinman et al., 2015). Such evidence might increase incentive amongst individuals who have trouble losing bodyweight.
- If one does desire weight loss, VLCDs can help with body fat reduction (Feinman et al., 2015). Evidence suggested that low-fat diets did not produce the same degree of weight loss when comparing the effectiveness of VLCDs for the same. When randomly assigning 26 individuals to either a VLCD (<40 grams/day) or a low-fat diet for 3 months, the VLCD group lost an average of 6.9 kg compared to the low-fat group who lost an average of 2.1 kg (Feinman et al., 2015).
- Adherence to VLCDs among individuals with T2D are as good as other dietary interventions, and is often significantly better (Feinman et al., 2015). The researchers continued to note that low carbohydrate interventions were better than other approaches even when caloric intakes were maintained. Feinman et al. (2015) postulated that part of the effectiveness behind VLCDs is the appetite-suppressing effects and satiety. Such an outcome might be from the satiation experienced from protein and fat consumption, which also helps control blood sugar swings often associated with higher carbohydrate diets (Feinman et al., 2015). Research also indicated that individuals who implement VLCDs often reduce exogenous insulin used each day (Feinman et al., 2015).
- Replacement of carbohydrates with protein is considered generally beneficial compared to low fat diets (Feinman et al., 2015). Furthermore, higher protein intake (when using a VLCD) tended to have a favorable outcome on weight loss, resting metabolic rate, body composition, and cardiovascular risk when compared to fat reduced dietary interventions (Feinman et al., 2015).
- Dietary fat and saturated fat do not correlate with cardiovascular risk (Feinman et al., 2015). The researchers referenced several large clinical studies exploring saturated fat intake and risk of cardiovascular disease, which indicated no associations (Feinman et al., 2015). Furthermore, other studies replaced saturated fat intake with either polyunsaturated fats or carbohydrates; neither intervention reduced cardiovascular risk (Feinman et al., 2015).
- Plasma saturated fatty acids are influenced by carbohydrate consumption more than dietary fats (Feinman et al., 2015). The researchers outlined a study where 40 patients with metabolic syndrome were treated with a very low carbohydrate ketogenic diet (VLCKD) or low-fat diet. Interestingly, the VLCKD group had reduced plasma saturated fatty acids concentrations when compared to the low-fat group. Moreover, the VLCKD group were consuming saturated fats that were 3 times higher than the low-fat group diet (Feinman et al., 2015). Although VLCDs do not require large intakes of saturated fats, such evidence does outline a poor correlation to said fat intake and plasma levels of the same.
- A very good predictor of macrovascular damage amongst individuals with T2D is glycemic control (Feinman et al., 2015). HBA1C is a means of measuring average glucose levels over a span of 3 months. For every 1% increase in HBA1C, there is a 14% in the risk for myocardial infarction (MI) among T2D individuals. Furthermore, the researchers indicated that the opposite is also true; for every 1% increase in HBA1C, risk of MI increased. VLCDs were found to reduce HBA1C (Feinman et al., 2015).
- Restricting carbohydrate consumption is the most effective strategy for reducing serum triglycerides (TAGs) and increasing high-density lipoproteins (HDLs) (Feinman et al., 2015). The researchers cited a study where 210 individuals with T2D consumed a low glycemic diet (LGD) or a standard high cereal diet (SHCD). Results indicated the LGD group experienced an average increase in HDLs of 1.7 mg/dL while the SHCD experienced a 0.2 mg/dL decrease in HDLs (Feinman et al., 2015). Another research study assigned 84 T2D individuals to either a VLCKD or a LGD; the VLCKD had even more dramatic decreases in TAGs and increases in HDLs when compared to the LGD or the SHCD from the prior study (Feinman et al., 2015).
- VLCDs tend to reduce and often eliminate medications (for T2D) and lower insulin requirements for individuals with T1D (Feinman et al., 2015). As such, a reduction of medications and a reduction in symptoms is considered a strong and significant sign of efficacy. Feinman et al. (2015) cited studies where VLCDs (between 20-50 grams of carbohydrates/day) compared to moderate carbohydrate diet (MCD) with caloric restriction. Of the 11 subjects who completed the study in the VLCD group, 5 reduced or discontinued medications and 2 subjects discontinued medications completely. The MCD group had 13 subjects; only 1 subject discontinued medication (Feinman et al., 2015).
- Intense glucose lowering via restricted carbohydrate intake has no side effects, as opposed to pharmacological interventions to achieve the same (Feinman et al., 2015). For example, Feinman et al. (2015) noted a study where researchers used intensive drug therapies with high CVD risk patients. The study was halted because there was an excess of 200 deaths. There are no known side effects of VLCD interventions, especially when compared to the above study.
In conclusion, IR and T2D continues to grow as an epidemic. Common underlying aberrations between said conditions is the inability to properly control blood glucose/insulin levels, however, research suggests that VLCDs can help attenuate fasting and post-prandial glucose/insulin levels. Ultimately, such an intervention is likely to provide a simple, safe, and cost-effective means to help liberate individuals from the consequences and downstream manifestations of hyperinsulinemia and hyperglycemia.
References
Lord, R. S., & Bralley, J. A. (2012). Laboratory evaluations for integrative and functional medicine (2nded.). Duluth, GA: Genova Diagnostics.
Feinman, R. D., Pogozelski, W. K., Astrup, A., Bernstein, R. K., Fine, E. J.,
Westman, E. C., … Worm, N. (2015). Dietary carbohydrate restriction as the first approach in diabetes management: Critical review and evidence base. Nutrition, 31(1), 1-13.
-Michael McIsaac
