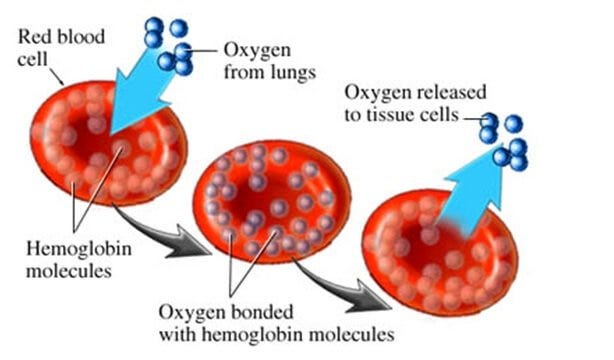
Iron deficiency anemia (IDA) can be defined as a condition frequently marked by a low hemoglobin level (Brown, 2014). It is characterized by the signs of iron deficiency (depleted iron stores, weakness, fatigue, short attention span, poor appetite, weak immune system) in addition to paleness, exhaustion, and a rapid heart rate (Brown, 2014).
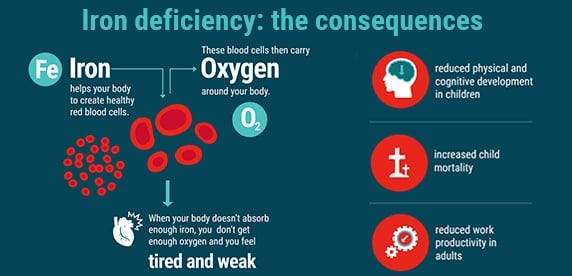
Women with IDA during pregnancy are likely to pass on less iron to the fetus, which may increase the risk of anemia during infancy (Brown, 2014). Infants who develop IDA could be subjected to other risk factors that may negatively affect their overall development including low birth weight, elevated lead levels, and poor nutrition (Brown, 2014). Brown (2014) also noted that long term IDA might contribute to learning delays due to iron’s role in central nervous system development.
Among children worldwide, iron deficiency (ID) is the most common micronutrient deficiency (Baker & Greer, 2010). 80% of the iron present within a newborn coalesces during the third trimester of pregnancy. Therefore, infants born prematurely are at risk of ID (Baker & Greer, 2010). Other risk factors of ID include maternal anemia, maternal hypertension, and diabetes; all of which can result in low fetal iron stores upon birth (Baker & Baker, 2010). Having considered ID/IDA, its characteristics and symptoms, the following will explore methods of attenuating said deficiency.
Screening for ID/IDA is recommended after one year of age, which would include an assessment of risk factors: history of premature birth, low birth weight, exposure to lead, exclusive breastfeeding after 4 months of age without iron supplementation, and introducing solid foods not fortified with iron (Baker & Greer, 2010). Baker and Greer (2010) also indicated analysis of eating patterns, poor growth, and inadequate nutrition as risk factors for ID/IDA. Prior to one year of age, however, supplementation of iron is generally indicated (Baker & Greer, 2010).

Baker and Greer (2010) generally recommended 0.27mg/day of iron for infants up to 6 months of age, and as high as 11mg/day 7-12 months of age. Such recommendations were predicated on sampling and averaging iron content in human breast milk through the Institute of Medicine (Baker & Greer, 2010). Specific recommendations include preterm infants (<37 weeks); iron supplementation of 2mg/kg/day starting at one month of age up to 12 months of age has been indicated. Additionally, term breastfed infants should begin iron supplementation after 4 months of age as breast milk has very little iron concentrations and infant stores begin to deplete after the 4 month period. As such, Baker and Greer (2010) recommended 1mg/kg/day of oral iron until iron fortified foods are introduced.
In conclusion, ID and IDA can be prevented if one remains aware of trends from birth to 12 months of age. General and specific iron supplementation is recommended in addition to a follow-up blood profile and assessment after 12 months of age. Such an approach ascertains if risk factors remain present and/or if iron supplementation has been effective. Ultimately, such a pragmatic method would help mothers prevent and track ID/IDA closely and quantitatively.
References
Baker, R., & Greer, F. R. (2010). Clinical report-Diagnosis and prevention of iron deficiency and iron deficiency anemia in infants and young children (0-3 years of age). American Academy of Pediatrics, 126(5), 1040-1050.
Brown, J. E. (2014). Nutrition through the life cycle (5th ed.). Stamford, CT: Cengage Learning.
-Michael McIsaac
