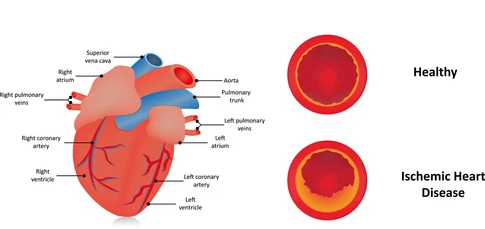
Ischemic heart disease (IHD) is the leading cause of death worldwide, making it a considerable global health problem with far reaching consequences in terms of morbidity, and mortality and healthcare costs. However, cardiovascular health can be assessed via analysis of blood biomarkers to include (but not limited to) total cholesterol, homocysteine, alkaline phosphatase, and high-density lipoproteins (HDLs). As such, the following will consider said biomarkers in greater detail, their relationship to well-being, and nutritional/supplemental interventions to support cardiovascular health.
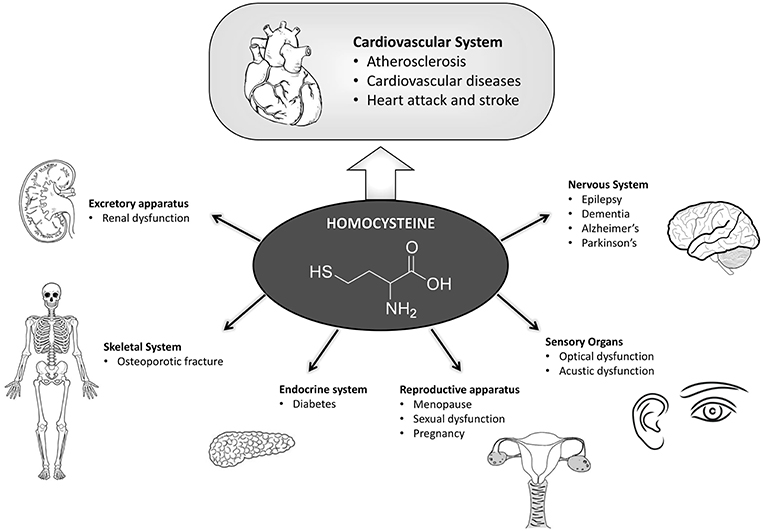
As discussed in this author’s last post, homocysteine is an amino acid that, at high concentrations, can increase oxidative stress, damage blood vessel linings, and potentially induce inflammation.1 If B12, B6, and/or folate (B9) levels are inadequate, homocysteine concentrations can rise.2 As such, this author would suggest an additional panel including B12, methylmalonic acid, B6, and folate measures. If levels were determined as low, this author would suggest foods rich in said micronutrients (please refer to previous post covering the same) that were considered deficient. If panels continued to be low despite nutritional interventions, supplementation could be indicated.

High total cholesterol (TC) can often be present with concomitant low concentration of large HDLs. High total cholesterol above 200 mg/dL has been associated with increased risk of cardiovascular disease (CVD).3 However, said TC concentrations can be reduced by increasing fiber intake. Dietary fiber increases the rate and amount of bile acid excretion helping reduce both total and low-density lipoprotein (LDL) cholesterol.4 Furthermore, once fiber begins to ferment in the colon, said fiber facilitates the production short-chain fatty acids (SCFAs), which down regulate the synthesis of cholesterol.4(3) Finally, fiber may have decrease the presence of pro-inflammatory cytokines; cell signaling molecules known to negatively affect plaque stability.4(3)
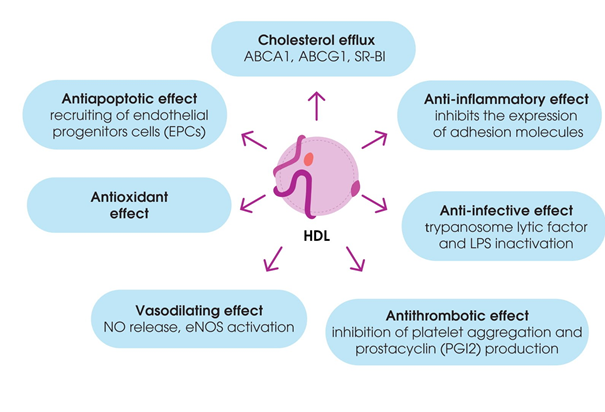
HDLs are responsible for reverse cholesterol transport; a process which refers to the ability of said lipoprotein to gather excess cholesterol from peripheral tissues and deliver to the liver for excretion in bile/bile acids.2(149) Abnormally low levels of large HDL particles suggests impaired HDL metabolism in addition to atherogenic dyslipidemia; conditions that are common, especially among overweight/obese individuals with other cardiovascular risk factors.5 As such, it is imperative to ensure optimal levels of HDLs, especially those of the large HDL subspecies. Nutritional interventions to facilitate increases in the concentrations of large HDLs could include low carbohydrate diets, as evidenced by the research by Finelli et al5 If HDL concentrations continue to remain below optimal levels, supplementation of omega-3 fatty acids can facilitate an increase of said lipoproteins.6
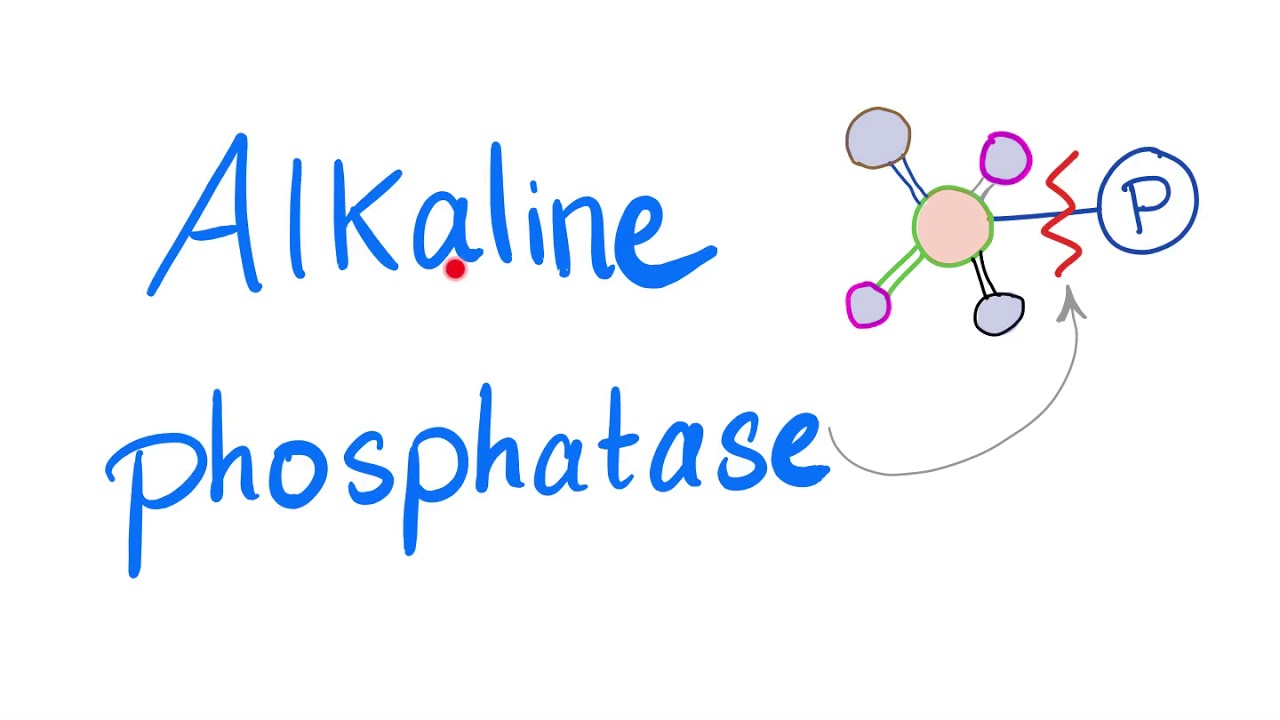
Low alkaline phosphatase (ALP) levels can also be problematic. Such a marker is relevant because its deficiency is associated with ischemic (restricted blood flow) heart disease (IHD).7 One role of ALP is mitigating the inflammatory effects of lipopolysaccharides (LPS); mouse studies have indicated that endotoxemia, a persistently increased concentration of bacterial endotoxin LPS in the blood, can induce low-grade systemic inflammation.7(2) Such a condition can lead to diabetes, and dyslipidemia. Thus, increasing levels of ALP can facilitate decreases in chronic inflammation. Malo et al7(7) indicated that ALP could be up-regulated by increasing thyroid hormone, curcumin, short-chain fatty acids, and omega-3 fatty acids.
In conclusion, IHD is a leading cause of death worldwide, making it a considerable global health problem with far reaching consequences in terms of morbidity, and mortality and healthcare costs. However, preventative measures can be taken by assessing biomarkers, among others, such as total cholesterol, homocysteine, alkaline phosphatase, and high-density lipoproteins (HDLs). Such steps, in conjunction to targeted dietary and lifestyle interventions, can provide a meaningful opportunity to reduce IHD risk while improving the health, performance, and longevity of individuals.
References
1. Tymoczko JL, Berg JM, Stryer L. Biochemistry: A Short Course. 3rd ed. New York, NY: Freeman and Company; 2015.
2. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism.7th ed. Boston, MA: Cengage Learning; 2018.
3. Sun YE, Wang W, Qin J. Anti-hyperlipidemia of garlic by reducing the level of total cholesterol and low-density lipoprotein: A meta-analysis. Medicine. 2018;97(18):1-8. doi: http://dx.doi.org/10.1097/MD.0000000000010255.
4. Hartley L, May MD, Loveman E, et al. Dietary fibre for the primary prevention of cardiovascular disease (Review). Cochrane Database Syst Rev. 2016;7(1):1-78. doi: 10.1002/14651858.CD011472.pub2
5. Finelli C, Crispino P, La Sala N, et al. The improvement of large high-density lipoprotein (HDL) particle levels, and presumably HDL metabolism depend on effects of low-carbohydrate diet and weight loss. EXCLI J. 2016;15:166-176. doi:10.17179/excli2015-642.
6. Simopoulos AP. The importance of the omega-6/omega-3 fatty acid ratio in cardiovascular disease and other chronic diseases. Exp Biol Med. 2008;233(6):674-688. doi:10.3181/0711-MR-311.
7. Malo J, Alam MJ, Sharnaz M, et al. Intestinal alkaline phosphatase deficiency is associated with ischemic heart disease. Hindawi. 2019;1-11. doi: https://doi.org/10.1155/2019/8473565.
-Michael McIsaac
