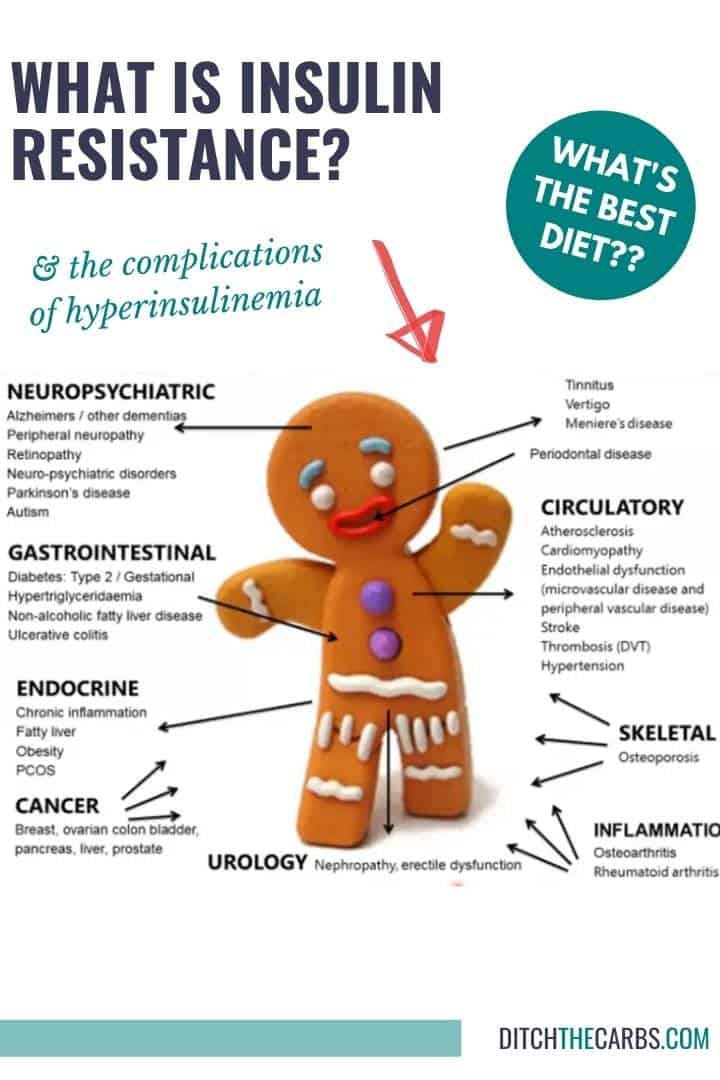
Modern Western diets derive approximately 70% of total daily energy from refined carbohydrate sources such as sugar, vegetable oils, processed foods, and alcohol (Ilich, Kelly, Kim, & Spicer, 2014). In contrast, during the paleolithic era (over 11,000 years ago) individuals consumed over 73% of total daily calories from animal sources (Cordain, Miller, Eaton, Mann, Holt, & Speth, 2000). The sharp divergence in macronutrient ratio distribution has likely caused aberrations in human health including diabetes, poor blood lipid profiles, cardiovascular disease, obesity, and decreased insulin sensitivity (Song, Lee, Song, Paik, & Song, 2014).
Due to the prominence, interconnectedness, and widespread occurrence of the above listed diseases, they have become collectively known as metabolic syndrome (MS) (Song et al., 2014). As a means of restoring the health, performance, and longevity of individuals with MS, this author would like to provide evidence supporting a return to lower carbohydrate consumption, commonly known as the very low carb/ketogenic (VLCKD) diet.
VLCKDs can be defined as less than fifty grams of carbohydrates a day (Paoli, Rubini, Volek, & Grimaldi, 2013). In one study, Cicero, Beneli, Brancaleoni, Dainelli, Merlini, and Negri (2015) considered how physicians could intervene and prescribe VLCKDs to their patients who were obese (one manifestation of MS). The test was conducted on a group of 377 patients, which were monitored for progress over a year.
Results indicated statistically significant improvements in body mass index, systolic blood pressure, diastolic blood pressure, hemoglobin A1c, low-density lipoprotein, and high-density lipoprotein counts in those who maintained VLCKDs throughout the study (Cicero et al., 2015). VLCKDs not only attenuate the aforementioned biomarkers; they also have distinct affects upon insulin resistance and type 2 diabetes. Thus, the following section will consider the impact of carbohydrate manipulation on resting blood glucose levels, as well as methods of mitigating pancreatic influence in energy production.
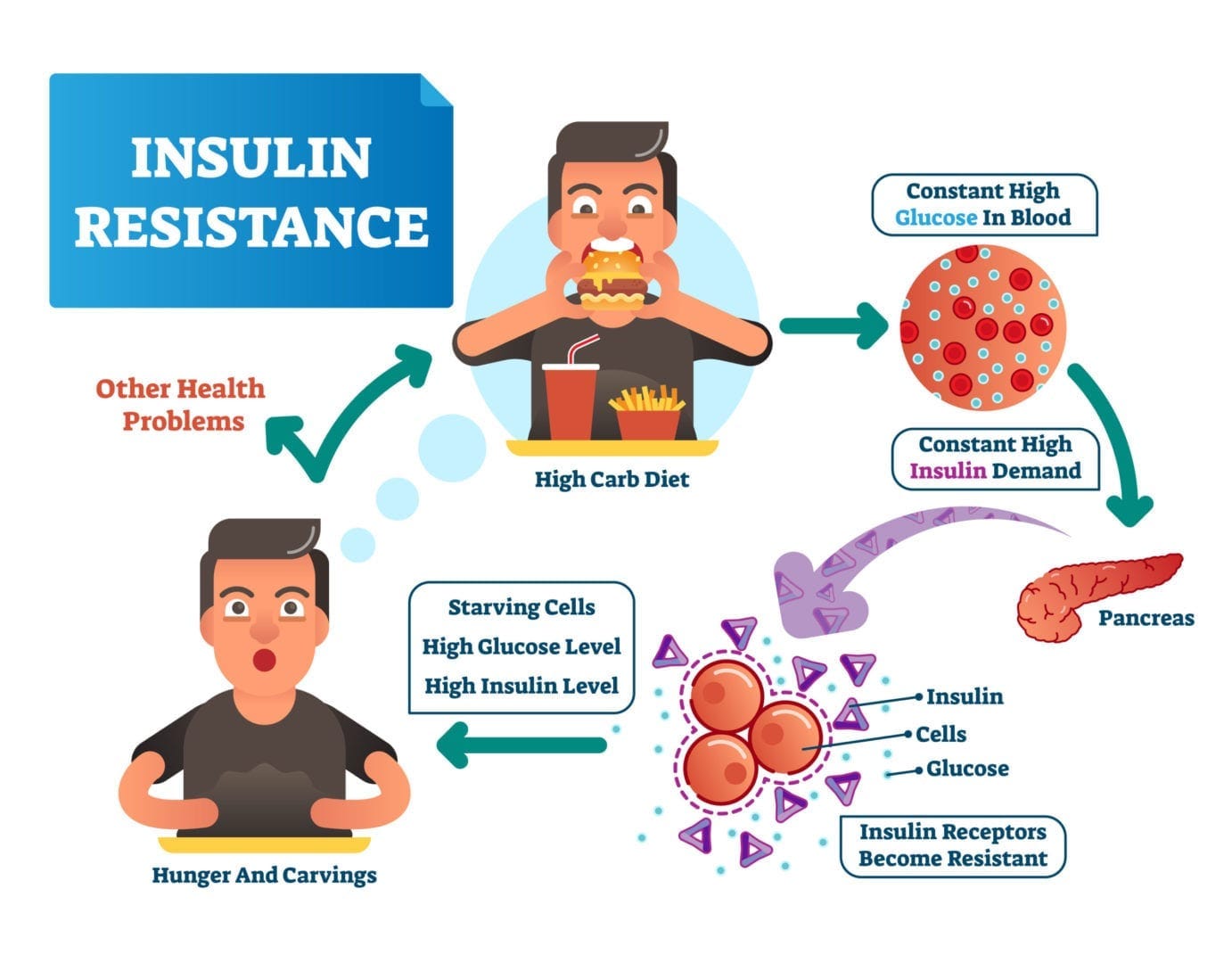
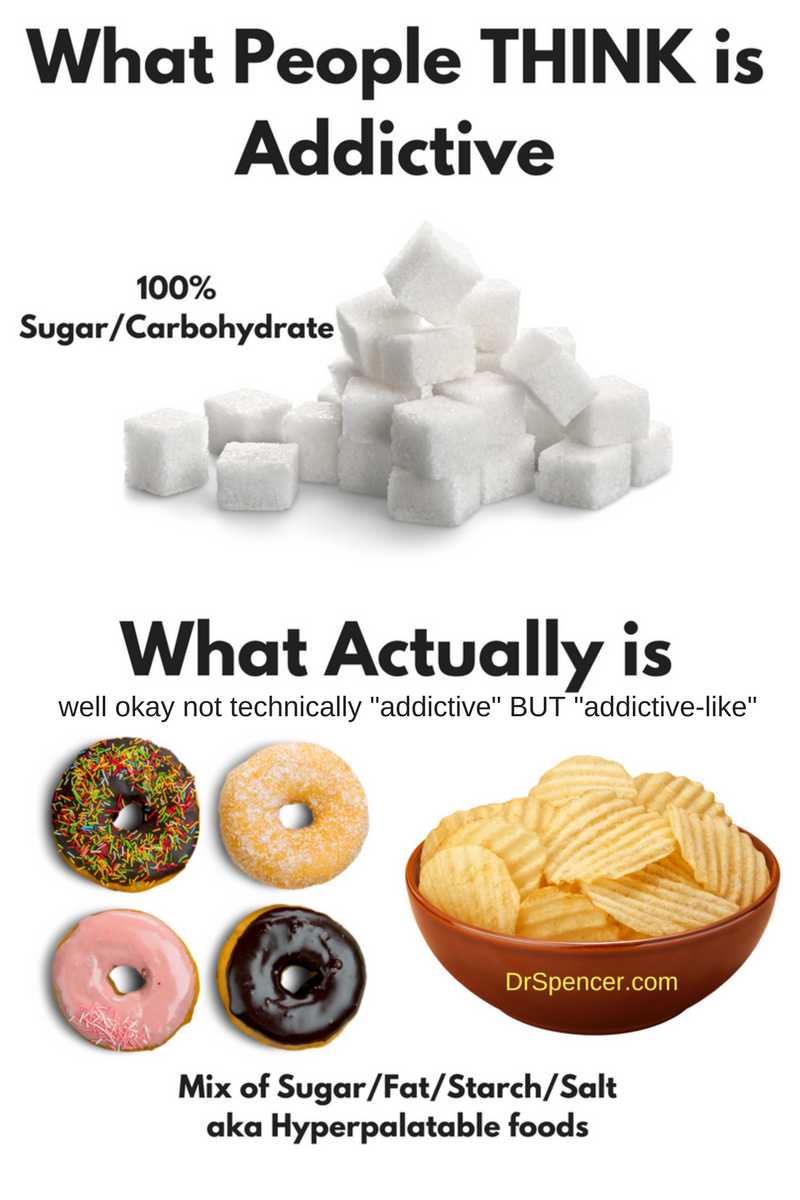
Insulin resistance and type 2 diabetes are other constituents of MS characterized by an impaired ability to metabolize glucose (Paoli et al., 2013). Generally, small and infrequent episodes of excess sugar consumption do not cause serious physiological or biochemical maladies.
However, chronic overconsumption of carbohydrates leads to marked changes in the management and storage of blood glucose, leading to reduced lean body mass and increased fat mass/obesity (Paoli et al., 2013). Although excessive carbohydrate consumption can induce unfavorable changes in homeostasis, the severity of insulin resistance and type 2 diabetes has been mitigated and/or eradicated by VLCKDs (Paoli et al., 2013).
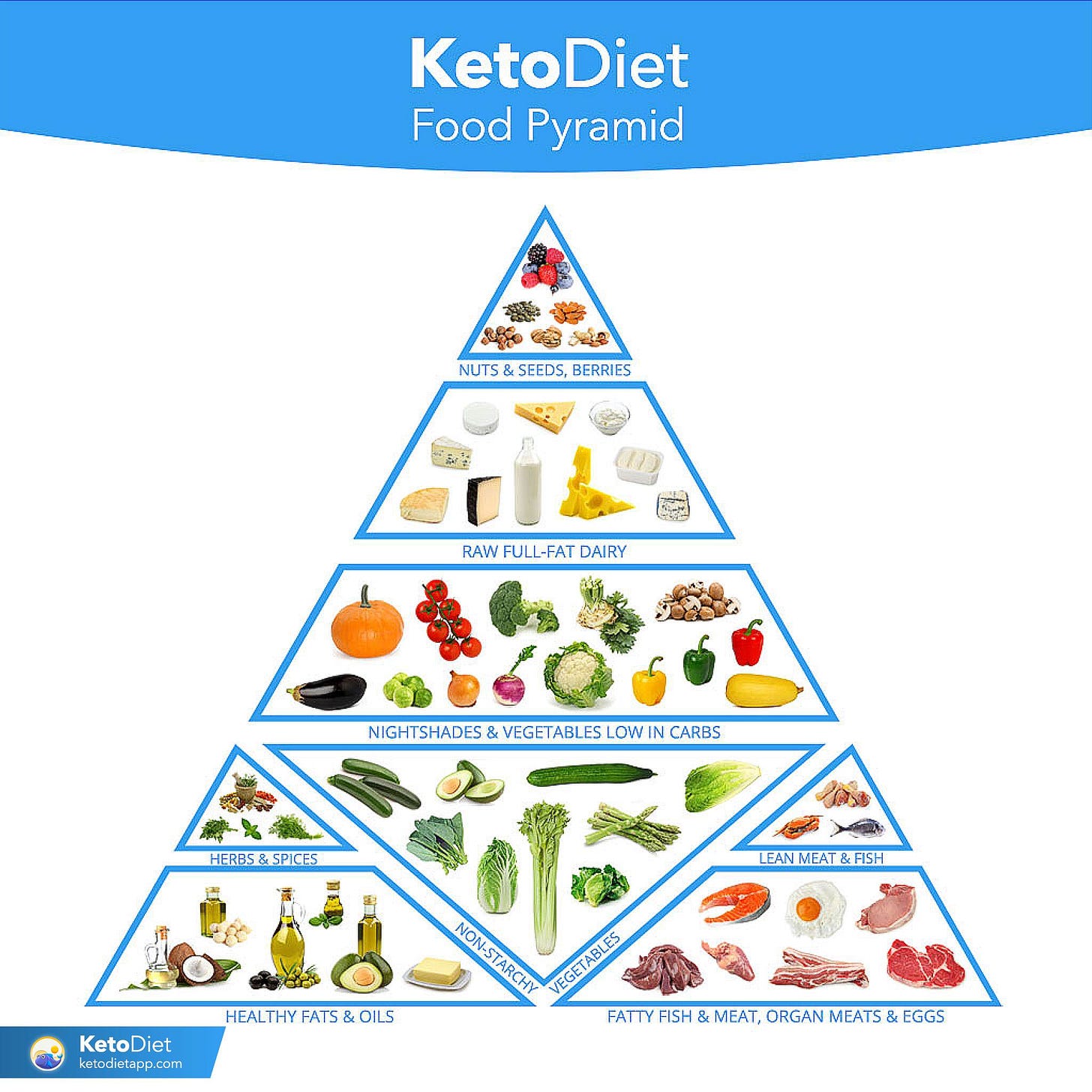
Slowly introducing foods that supply energy (i.e., proteins and fats) while being low in sugars, allows blood glucose concentrations to decrease without the need for insulin, minimizing the requirement for pancreatic influence (Paoli et al., 2013).
In essence, providing lower carbohydrate ingestion encourages an adaptive change in substrate utilization from glucose to fatty acids derived from the breakdown of triglycerides. Such a process is postulated to help mitigate insulin resistance and/or type 2 diabetes (Paoli et al., 2013). Moreover, VLCKDs also help manage bodyweight, which will be covered in the following section.

Weight loss is another component positively affected by VLCKDs. Although individuals who have embarked on VLCKDs experience reductions in fat mass, researchers are still uncertain regarding the mechanisms, which contribute to changes in body composition (Paoli et al., 2013).
Paoli et al. (2013) outlined four factors, which are thought to create weight loss: appetite suppression and higher satiety from protein consumption, reduction in lipogenesis and increased lipolysis (explained in the previous section), increased metabolic efficiency in consuming fats, and increased metabolic costs of gluconeogenesis and the thermic effect of proteins. In essence, VLCKDs appear to satisfy hunger while individuals lose bodyweight.
MS has an intimate connection to excessive refined carbohydrate consumption. However, diabetes, poor blood lipid profiles, cardiovascular disease, obesity, and decreased insulin sensitivity (constituents of MS) can be treated by reconsidering the impact of food on health (Paoli et al., 2013). Ultimately, such an approach embraces nutrients as medicine, treating the cause rather than the symptoms; a paradigm shift from a traditional allopathic approach, which treats the symptoms rather than the cause.
References
Cicero, A. F. G., Beneli, M., Brancaleoni, M., Dainelli, G., Merlini, D., & Negri, R. (2015). Middle and long-term impact of a very low-carbohydrate ketogenic diet on cardiometabolic factors: A multi-center, cross-sectional, clinical study. High Blood Pressure and Cardiovascular Prevention, 22(4), 389-394.
Cordain, L., Miller, J. B., Eaton, S. B., Mann, N., Holt, S. H. A., & Speth, J. D. (2000). Plant-animal subsistence ratios and macronutrient energy estimations in worldwide hunter-gatherer diets. The American Journal of Clinical Nutrition, 71, 682-692.
Ilich, J. Z., Kelly, O. J., Kim, Y., & Spicer, M. T. (2014). Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Archives of Industrial Hygiene and Toxicology, 65(2), 139-148.
Paoli, A. (2006). Ketogenic diet for obesity: Friend or foe? International Journal of Environmental Research and Public Health, 11(2), 2092-2107.
Song, S., Lee, J.E., Song, W.O., Paik, H.Y., & Song, Y.J. (2014). Carbohydrate intake and refined-grain consumption are associated with metabolic syndrome in the Korean adult population. Academy of Nutrition and Dietetics, 114(1), 54-62.
-Michael McIsaac
