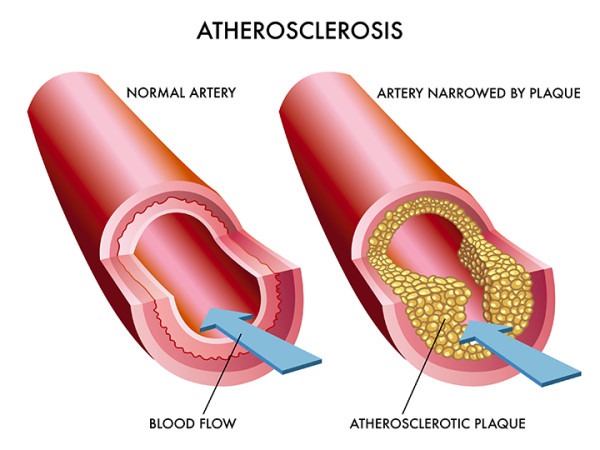
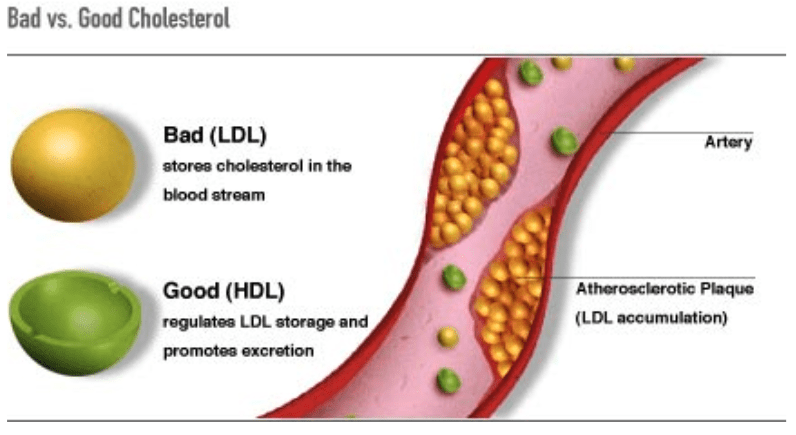
Atherosclerosis can be defined as the buildup of fats, cholesterol, and other substances in and on the artery walls (plaque), which can restrict blood flow (Mayo Clinic, 2018). Said condition can manifest as early as childhood with the development and deposition of fatty cholesterol streaks along the endothelium (blood vessel wall) (Lee & Nieman, 2013). As time passes, lipids continue to deposit and collect forming a fibrous plaque. Left untreated, atherosclerosis can lead to ischemia (impaired blood flow) or a myocardial infarction (heart attack); a leading cause of death among American males and females (Lee & Nieman, 2013). Thus, it is imperative to use a biomarker/biomarkers to track progressions of such a condition. One such biomarker is low-density lipoprotein (LDL). As a means of appreciating LDLs as a risk factor, the following will briefly consider its structure, utility, and limitations in predicting cardiovascular events.
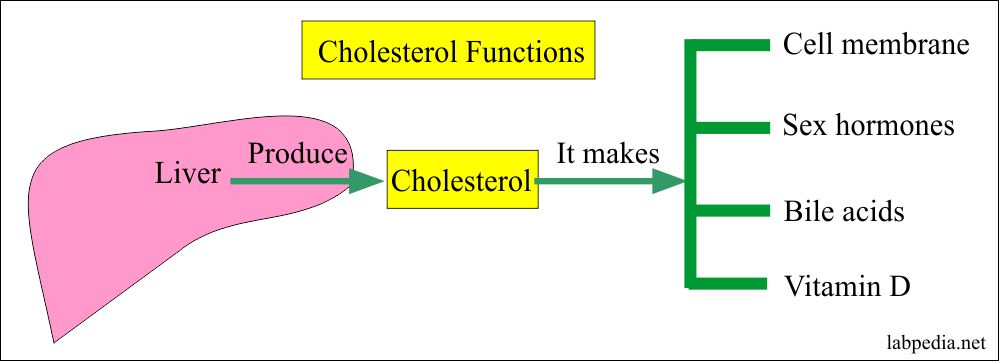
LDLs act as transporters of cholesterol (and triglycerides); cholesterol, by itself, is not soluble in the bloodstream. Therefore, LDLs (and other lipoproteins) carry said lipid in a form that allows for successful transport throughout the blood, cells, tissues, and organs of the body (Lee & Nieman, 2013). Cholesterol is a lipid that is essential for the structure of cell membranes, is a precursor for steroid hormones and vitamin D, and is used by the liver to produce bile acids (helps with digestion) (Lee & Nieman, 2013). Thus, it is erroneous to anthropomorphize cholesterol as “good” or “bad”. Rather, it is more appropriate to view said lipid as a tool in the body’s physiological arsenal that can work favorably, or unfavorably, upon the homeostasis of an individual. The following will explore the constituents and function of LDLs in greater detail.
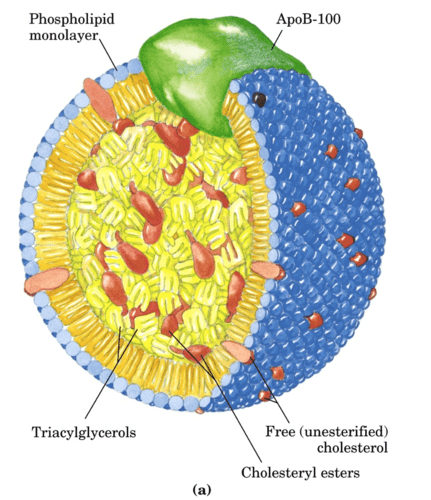
LDLs are composed (by mass) of 25% protein, 43% cholesterol, 23% phospholipids, and 9% triglycerides (Lee & Nieman, 2013). They are considered low-density due to the comparatively low levels of protein/lipid ratios when compared to another lipoprotein known as high-density lipoprotein (HDL); HDLs which have a significantly higher proportion of protein molecules to its associated lipids (50% protein, 18% cholesterol, 30% phospholipids, 2% triglycerides) making it denser and smaller than LDLs (Lee & Nieman, 2013). The protein component of lipoproteins (known as apoproteins, such as Apo-B) are highly active sites; apoproteins are responsible for modifying the composition and structure of their spherical macromolecular complex. Such activity enables binding and ingestion of LDLs to target cells as well as the exchange of lipids (Lee & Nieman, 2013).
LDL serum concentrations (i.e., LDL-C levels <100mg/dL is considered optimal) have long been used as a risk factor as LDLs tend to deposit cholesterol along the endothelium (atherogenic), where HDLs tend to remove cholesterol from the same (Lee & Nieman, 2013). However, evidence now indicates that LDL concentrations are only one element to consider when analyzing said lipoprotein; different subclasses and concomitant degrees of atherogenicity exist among LDLs. Smaller LDLs tend to be more atherogenic than larger LDLs as they can penetrate the endothelium in an easier fashion, are more easily oxidized, and more likely to form plaques(Rosenson, 2004). Thus, higher concentrations of LDL-C, by itself, does not indicate the particle size, only concentration. Ultimately, in the light of LDL particle size and atherogenicity, LDL-C serum concentrations as an exclusive measure might be limiting it its meaningfulness, interpretation, and utility.
LDL particle size can be revealed by using nuclear magnetic resonance (NMR) imaging (Rosenson, 2004). Such a technology has identified small LDLs as ≤20.5nm, which are highly atherogenic. In addition to the particle size of small LDLs, another pertinent risk factor includes the number/concentration of said lipoprotein. Rosen (2004) indicated that a small LDL particle concentration of >30mg/dL was highly associated with coronary progression, as measured by the presence of apolipoprotein B (the main protein component of LDL) (Pagna & Pagna, 2014). In essence, high concentrations of small LDL particles are closely associated with atherosclerotic plaque and cardiovascular events (Rosenson, 2004).
In conclusion, total LDL-C, as a stand-alone biomarker, provides a narrow and limiting insight/interpretation of cardiovascular risk. However, deeper examination of LDL particle size and concentration (especially when combined with other biomarkers-total cholesterol, triglycerides, HDL-C, ratios of LDL-C/HDL-C, and total cholesterol/HDL-C) provides a more meaningful outline of an individual’s cardiovascular status. Ultimately, such knowledge provides at-risk individuals the opportunity to proactively manage their lipid profiles before their conditions worsen.
References
Lee, R. D., & Nieman, D. C. (2013). Nutritional assessment (6thed.). New York, NY: McGraw-Hill.
Mayo Clinic (2018). Arteriosclerosis/Atherosclerosis. Retrieved from https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/symptoms-causes/syc-20350569
Pagana, K. D., & Pagana, T. J. (2014). Manual of diagnostic and laboratory tests (5thed.). St. Louis, MO: Mosby.
Rosenson, R. S. (2004). Clinical role of LDL and HDL subclasses and apolipoprotein measurement. ACC Current Journal Review, 13(5), 33-37.
-Michael McIsaac
