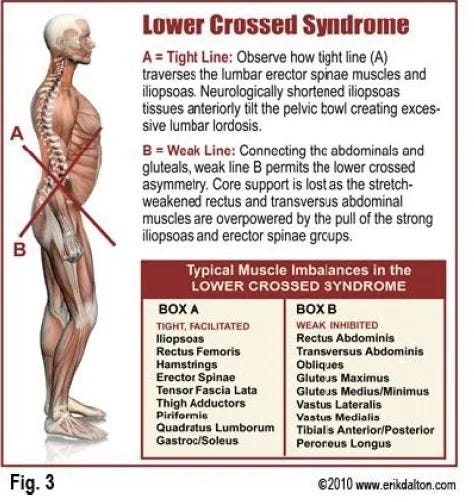
Vladimir Janda was a physician who, in the late 1970s, found trends in joint actions and muscle imbalances within the human body. Among these trends was a phenomenon he termed lower crossed syndrome (Page, Frank & Lardner, 2014). Janda observed that there were unique behaviors of muscles and joints, which created aberrant and unusual motions of the lower body.
In lower crossed syndrome (LCS), the abdominals of the anterior side, and the gluteus minimus/maximus/medius of the posterior side tend to be inhibited. Conversely, the rectus femoris/psoas major of the anterior side and thoraco-lumbar extensors of the posterior side tend to be overactive/facilitated. Thus, a crossedpattern of inhibited and facilitated muscles exists (Page et al., 2014).
In the following sections, I would like to explore Janda’s findings by observing some of the key muscles and joints involved in LCS; the erector spinae, rectus abdominis, psoas major, and rectus femoris. I will also provide the relevant anatomy (i.e., origins, insertions, nerve supply, and muscle action) as well as how these muscles behave under conditions of sub-optimal postures. Finally, I will provide solutions to slow and/or return these muscles to their natural resting lengths and function.
RECTUS ABDOMINIS: FUNCTIONAL ANATOMY
The rectus abdominis (RA) is one of several abdominal muscles (i.e., internal oblique, external oblique, transversus abdominis) that surround the anterior and lateral portions of the core (Bliven, 2014). It is the only vertically aligned abdominal muscle, is the most superficial, and is largely responsible for trunk flexion/rib depression/exhalation (Bliven, 2014). However, as a spinal stabilizer, the RA works in a pattern of co-contraction with the other abdominal muscles and back muscles (McGill, 2007). Below are deeper breakdowns of the RA, its origins and insertions, as well as innervations and actions:
| Muscle | Origin | Insertion | Innervation | Action |
| Rectus Abdominis | Fifth, sixth, and seventh costal cartilages: costoxiphoid ligaments and xiphoid process | Crest of the pubis and pubic tubercle; front of symphysis pubis | Lower seven thoracic nerves (T6-T12) | Flexes vertebral column; tenses anterior abdominal wall; compresses abdominal contents, and assists in exhalation |
Clemente (2011)
RECTUS ABDOMINIS: PATHOMECHANICS
In LCS, the rectus abdominis tends to be inhibited, in conjunction with the gluteal muscles (i.e., gluteus minimus, maximus, and medius) (Page et al., 2014). A person presenting with an inhibited RA will often exhibit a hyperlordic curve in the lumbar vertebrae with an associated extended abdomen (Sahrmann, 2002). The person may also present with low back pain, and symptoms may increase when standing, reaching overhead or lying supine with the legs extended (Sahrmann, 2002).
PSOAS MAJOR: FUNCTIONAL ANATOMY
The psoas major is a muscle that is a powerful hip flexor. During the open chain phase of walking or climbing stairs, the psoas helps lift the leg forwards and upwards. When the legs are fixed, the psoas flexes the trunk (Clemente, 2011). Clemente (2011) also noted that in cadavers, 40% of dissections indicated the presence of the psoas minor. The psoas minor does not flex the hips, however, it is a weak flexor of the trunk. Below are deeper breakdowns of the psoas major and minor, their origins and insertions, as well as innervations and actions:
| Muscle | Origin | Insertion | Innervation | Action |
| Psoas Major | Transverse process and body od T12 and upper 4 lumbar vertebrae; intervertebral discs between T12 and L5 | Lesser trochanter of the femur (also receives the fibers of the iliacus muscle) | Branches from upper four lumbar nerves | Powerful flexor of the thigh at the hip; when the femurs are fixed, they flex the trunk |
| Psoas Minor | Lateral surface of the bodies of T12 and L1 vertebrae | Pectineal line and iliopectineal eminence and the iliac fascia (frequently merges with the psoas major tendon) | Branches from L1 nerve | Weak flexor of the trunk |
Clemente (2011)
PSOAS MAJOR: PATHOMECHANICS
In LCS, the psoas major tends to be in a shortened/facilitated position. A shortened psoas major will create an anterior pelvic tilt when standing upright or when in a supine position with passive hip extension (Sahrmann, 2002). Because the psoas major is attached to the lumbar spine, it can create compression, anterior shear, and pain of the lumbar vertebrae when in a shortened position (Sahrmann, 2002).
RECTUS FEMORIS: FUNCTIONAL ANATOMY
The rectus femoris is part of a larger group of muscles collectively known as the quadriceps femoris (Bliven, 2014). The quadriceps femoris is composed of the vastus lateralis, vastus intermedius, vastus medialis and rectus femoris. All four muscles extend the knee. However, the rectus femoris also assists in hip flexion because of its unique origin; it originates in the groove above the acetabulum and anterior inferior iliac spine, unlike the other quadriceps femoris muscles (Clemente, 2011). Below are deeper breakdowns of the rectus femoris, its origins and insertions, as well as innervations and actions:
| Muscle | Origin | Insertion | Innervation | Action |
| Rectus Femoris | Straight head; anterior inferior iliac spine
Reflected head; the groove above the acetabulum |
Shares a common tendon on the patella with the other 3 quadriceps muscles and inserts on the tibial tuberosity | Femoral nerve
(L2, L3, L4) |
Extends the knee and assists in hip flexion |
Clemente (2011)
RECTUS FEMORIS: PATHOMECHANICS
In LCS, the rectus femoris tends to be in a shortened/facilitated position along with the psoas major. A shortened rectus femoris will induce an anterior pelvic tilt and lumbar extension (Sahrmann, 2002). During a Thomas test, a shortened rectus femoris will be indicated by knee flexion of less than 90 degrees (Sahrmann, 2002).
ERECTOR SPINAE: FUNCTIONAL ANATOMY
The erector spinae is a term used to describe a group of muscles along the spinal column of the back, traversing the lumbar regions up to and including the cervical regions. The erector spinae can be subdivided into 3 major groups: the iliocostalis, longissimus, and spinalis (Bliven, 2014). Unilaterally, these muscles provide lateral flexion to the same side they contract on. Bilaterally, the erector spinae group extends the spinal column. Below are deeper breakdowns of the 3 erector spinae groups, their origins and insertions, as well as innervations and actions:
| Iliocostalis (subdivisions below) | Origin | Insertion | Innervation | Action |
| Lumborum | Posteromedial iliac crest, and from the common tendon of erector spinae muscle | 6-7 muscle fascicles on the inferior borders of 6 or 7 ribs | Dorsal posterior rami of lower thoracic and upper lumbar nerves | Extend, laterally flex and assists in rotation of the vertebral column. Also depresses the ribs |
| Thoracis | Upper borders of lower 6 ribs | Upper border of first six ribs and on transverse process of the seventh cervical vertebrae | Dorsal primary rami of the C8 and upper six thoracic spinal nerves | Extends, laterally flexes and assists in rotation of the thoracic vertebrae |
| Cervicis | Angles of the third, fourth, fifth, and sixth ribs | Posterior tubercles of the transverse processes of the fourth, fifth, and sixth cervical vertebrae | Dorsal primary rami of the lower cervical and upper thoracic spinal nerves | Extends, laterally flexes, and assists in rotation of the cervical and upper thoracic vertebrae |
(Clemente, 2011)
| Longissimus (subdivisions below) | Origin | Insertion | Innervation | Action |
| Thoracis | Intermediate continuation of the erector spinae muscle; transverse processes of the lumbar vertebrae | On the tips of the transverse processes of all thoracic vertebrae; onto the lower 9 or 10 ribs between their tubercles and angles | Dorsal primary rami of the thoracic and lumbar spinal nerves | Extends and laterally flexes the vertebral column. Also helps depress the ribs |
| Cervicis | Tips of the transverse processes of the upper four or five thoracic vertebrae | Posterior tubercles of the transverse processes of C2–C6 cervical vertebrae | Dorsal primary rami of the upper thoracic and lower cervical spinal nerves | Extends the vertebral column and bends it to one side |
| Capitis | From the transverse processes of the upper four or five thoracic vertebrae and off of the articular processes of the lower three or four cervical vertebrae | Posterior margin of the mastoid process of the temporal bone | Dorsal primary rami of the middle and lower cervical spinal nerves | Extends the head. The muscle of one side bends the head to the same side and turns the face to that side |
(Clemente, 2011)
| Spinalis
(subdivisions below) |
Origin | Insertion | Innervation | Action |
| Thoracis | From spinous processes of T11, T12, L1, and L2 vertebrae | Spinous processes of the upper four to eight thoracic vertebrae | Dorsal primary rami thoracic spinal nerves | Extends the vertebral column |
| Cervicis | Spinous processes of C7, T1, and T2 vertebrae and the ligamentum nuche | Spinous processes of the axis and those of the C3 and C4 | Dorsal primary rami of the lower cervical spinal nerves | Extends the cervical vertebrae |
| Capitis | Spinous processes of the lower cervical and upper thoracic vertebrae | Inserts with the semispinalis capitis muscle between the superior and inferior nuchal lines of the occipital bone | Dorsal primary rami of the upper cervical spinal nerves | Extends the head |
(Clemente, 2011)
ERECTOR SPINAE: PATHOMECHANICS
A person with LCS would likely present with a hyperlordic curve in the lumbar vertebrae, with an associated extended abdomen (Sahrmann, 2002). The person may also present with low back pain, and symptoms may increase when standing, reaching overhead or lying supine with the legs extended (Sahrmann, 2002). This is due to the increased lumbar extension that these movement patterns would impose. Associated diagnoses may include spinal stenosis, facet syndrome, degenerative disc disease, spondylolysis and osteoporosis (Sahrmann, 2002).
CORRECTING LOWER CROSSED SYNDROME
Relaxing and lengthening facilitated muscles (i.e., erector spinae, psoas major, and rectus femoris) would be a first step. Sullivan, Silvey, Button, and Behm (2013) reported that brief foam rolling, or self-myofascial release, for 10 seconds or more over a muscle group both relaxes and lengthens the same muscle group. Additionally Mohr, Long and Goad (2014) found that combining foam rolling with static stretching improved range of motion greater than stretching or foam rolling alone. Considering the benefits of foam rolling and stretching, I would suggest that the client with LCS perform foam rolling on the erector spinae, iliopsoas, and rectus femoris for 20 repetitions (i.e., approximately 10 seconds or more) per muscle group followed by static stretching, everyday. I would also include exercises to activate and strengthen inhibited muscles. The rationale for targeting facilitated muscles first is to increase range and mobility, as facilitated muscles tend to restrict joint range of motion. This will allow the strengthening exercises to have a greater effect over a larger range of motion. Below is a synopsis of a program, including video links, for a person with LCS. I would recommend this protocol 2-3 times per week on alternating days (i.e., Monday, Wednesday, Friday) to allow for recovery between sessions:
Videos can also be found at: http://www.youtube.com/watch?v=RV1ihOLdYY0&list=PLD5Xk-dZZYNqTUWYtk74rf75aZ-UkYG94
| Muscle | Impairment | Exercise | Sets | Repetitions | Weight |
| Erector Spinae | Facilitated | Foam Rolling | 1 | 20 (or greater than 10 seconds) | Bodyweight |
| Psoas Major | Facilitated | Foam Rolling +
|
1 | Foam rolling: 20 (or greater than 10 seconds) / Stretches: 20-30 seconds | Bodyweight |
| Rectus Femoris | Facilitated | Foam Rolling +
|
1 | Foam rolling: 20 (or greater than 10 seconds) / Stretches: 20-30 seconds | Bodyweight |
| Rectus Abdominis | Inhibited | Static planking variations:
Front and Side Plank
progressing to dynamic and unstable movement patterns:
Planking variations both stimulate the abdominals and stabilize the spine (McGill & Karpowicz, 2009). |
2-3 | Up to 40 seconds | Bodyweight |
| Gluteus Medius/Minimus/Maximus
(These muscles are out of the requirements of this paper. However, I included these as they are part of treating lower crossed syndrome) |
Inhibited | Hip Bridges
progressing to hip dominant patterns:
Research indicates hip bridges and deadlifts recruit gluteus maximus muscles optimally (Reiman, Bolgla, & Loudan, 2012). |
2-3 | 6-8 | Bodyweight, progressing to external loading |
As evidenced by the complexity and interrelationships found within LCS, treating one component of the condition might be shortsighted, as the syndrome does not occur in a vacuum. Many joints, muscles, and movement patterns contribute to the movement impairments unique to LCS. Thus, an approach that acknowledges the influences of each constituent of LCS would be advisable when treating this syndrome and seeking optimal outcomes.
References
Bliven, K. (2014). Functional anatomy of the back and spine. Part 1: Overview [Slideshow Presentation]. Retrieved February 25, 2014, from https://mycourses9.atsu.edu/bbcswebdav/pid-346743-dt-content-rid-7386865_1/courses/13-14WI-ONL-HM502-2-ASHS/Cervical%20and%20thoracic%20spine%281%29/Module%201%20-%20Presentation%20%20Back%20%26%20Spine%20-General%20Overview.pdf
Bliven, K. (2014). Functional anatomy of the back and spine.Part 4b: Lumbar spine, sacrum, & pelvis muscles [Slideshow Presentation]. Retrieved February 25, 2014, from https://mycourses9.atsu.edu/bbcswebdav/pid-347252-dt-content-rid-7392105_1/courses/13-14WI-ONL-HM502-2-ASHS/Lumbar%20and%20pelvic%20regions%281%29/Handout%20Back%20%26%20Spine.Lumbar%20Pelvis.P1%20structure.pdf
Clemente, C. D. (2011). Anatomy: A regional atlas of the human body(6thed.). Baltimore, MD: Lippincott Williams & Wilkins.
McGill, S. (2007). Low back disorders: Evidence-based prevention and rehabilitation(2nd ed.). Windsor, ON: Human Kinetics.
McGill, S., & Karpowicz (2009). Exercises for spine stabilization: Motion/motor patterns, stability progressions, and clinical technique. Archives of Physical Medicine and Rehabilitation,90 (1), 118-126.
Mohr, A. R., Long, B. C., & Goad, C. L. (2014). Foamrollingand static stretching on passive hip flexion range of motion.Journal Of Sport Rehabilitation. Retrieved January 30, 2014 from http://eds.a.ebscohost.com.p.atsu.edu/eds/detail?vid=7&sid=bd6a6510-bbd3-469c-947c-04a1752928df%40sessionmgr4001&hid=4113&bdata=JnNpdGU9ZWRzLWxpdmU%3d#db=cmedm&AN=24458506
Page, P., Frank, C., & Lardner, R. (2014). The Janda approach to chronic pain syndromes: Preserving the teachings of Dr. Vladimir Janda. Retrieved January 25, 2014 from http://www.jandaapproach.com/the-janda-approach/jandas-syndromes/
Reiman, M. P., Bolgla, L. A., & Loudan, J. K. (2012). A literature review of studies evaluating gluteusmaximusand gluteusmedius activationduring rehabilitation exercises. Physiotherapy Theory and Practice, 28(4), 257-268.
Sahrmann, S. (2002). Diagnosis and treatment of movement impairment syndromes(1rst ed.). St. Louis, MO: Mosby Inc.
Sullivan, K. M., Silvey, D. B. J., Button, D. C., & Behm, D. G. (2013). Roller-massager application to the hamstrings increases sit-and-reach range of motion within five to ten seconds without performance impairments.International Journal of Sports Physical Therapy.8 (3), 228-229.
-Michael McIsaac
