INTRODUCTION
Gout is one of the most well studied and characterized forms of arthritis affecting up to 4% of the population (2.68 per 1000 people); a condition occurring in males and females in a ratio of 4:1 respectively.1,5 Gout is an arthritic condition that mostly forms in the lower limbs, with a particular prevalence in the first toe (fancy term for big toe).2 Acute (immediate/sudden) flare-ups usually peak within 24 hours and slowly resolves within one to two weeks.2(1) Other than intense pain, additional symptoms include lingering discomfort lasting up to 2-3 weeks, inflammation, redness, and limited range of motion.3 However, if symptoms do not resolve and are left unchecked, there is risk of permanent joint damage.2(1)
WHAT CAUSES GOUT?
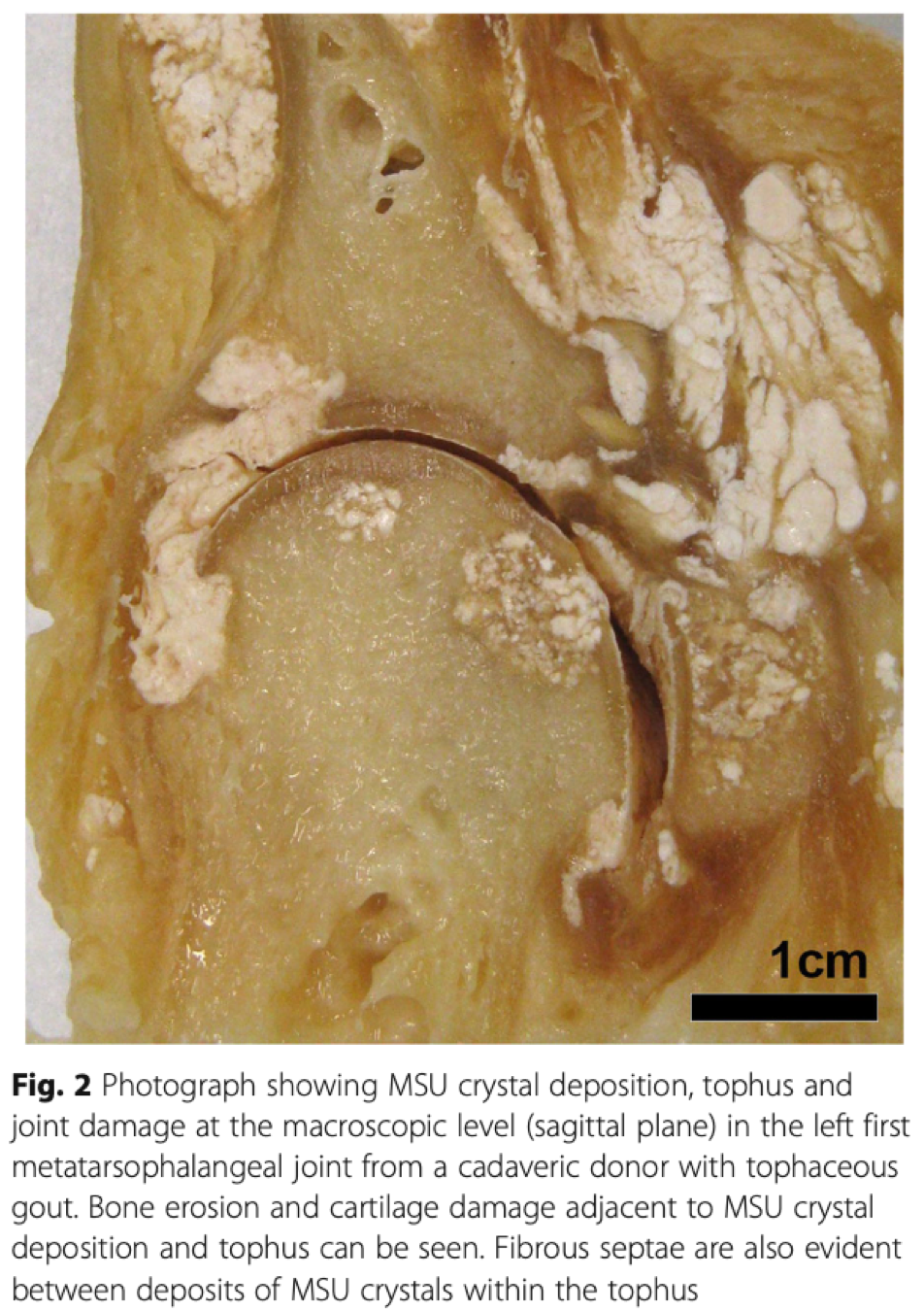
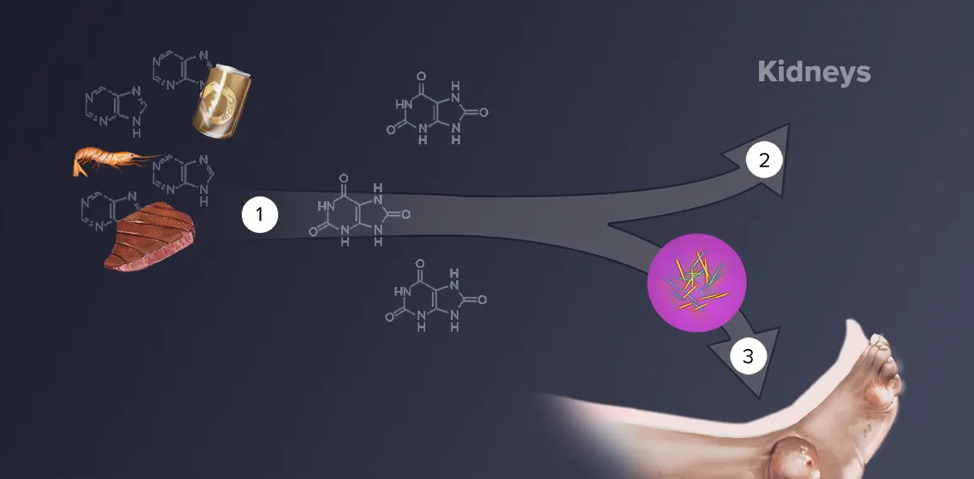
Gout is a condition caused by an accumulation of “crystals” in joints.1(496) These crystals are specifically termed monosodium urate crystals (MSU) that come from uric acid (SUA).1(496) When enough SUA accumulates in a joint, MSU combine together creating visible deposits known as tophi.1(496) We all have SUA floating around in us, but it can (not always though) become a problem when they exceed a threshold of 6.8 mg/dL in the blood.1(496)
THE RECIPE FOR GOUT
Hyperuricemia (high levels of SUA in the blood) is one factor that can set an individual up for gout. Other factors that may affect SUA deposition includes age, gender, hydration, the pH of fluids (synovial fluid) in the joint, electrolytes (sodium, potassium), collagen (makes cartilage), and proteoglycans (makes cartilage).1(496) However, the big factor that affects accumulation of MSU in joints is the balance (really the imbalance) between SUA production and SUA clearance (the kidneys and digestive system takes care of this).1(496)
PRODUCTION OF SUA
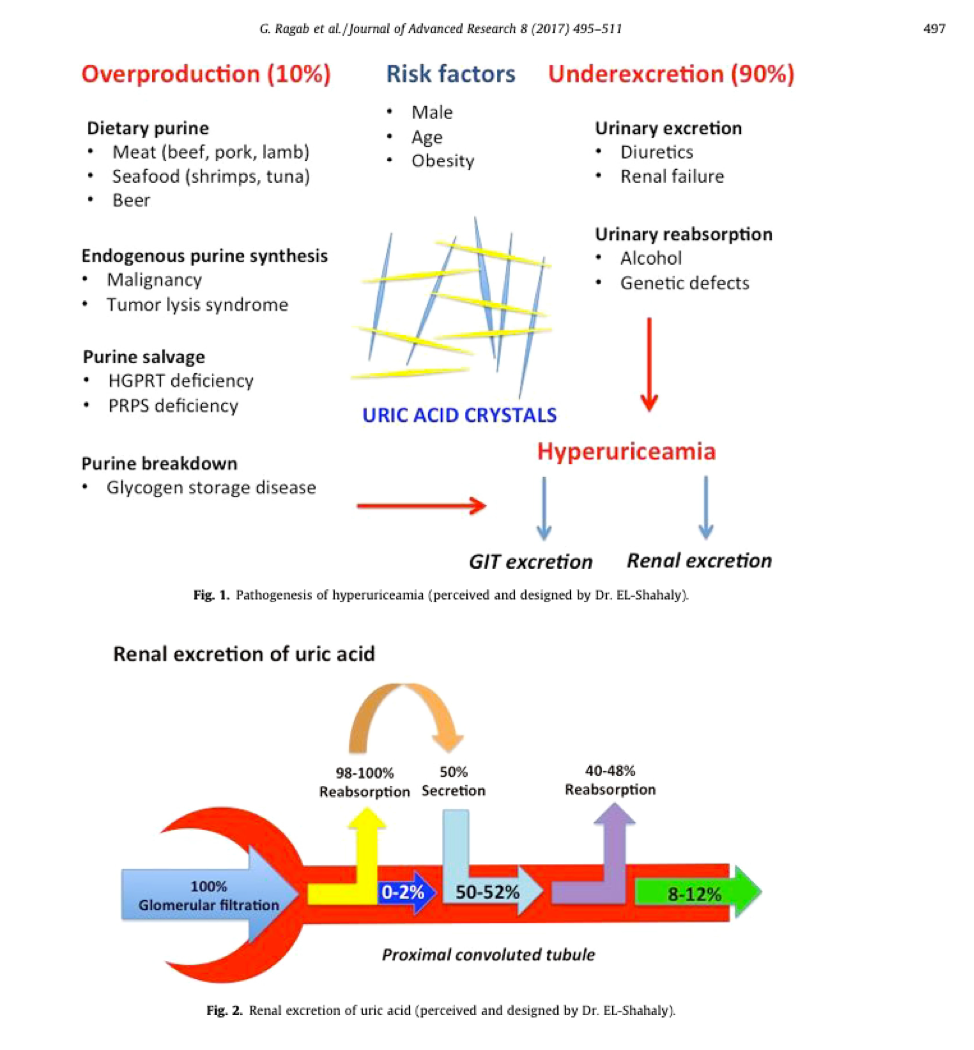
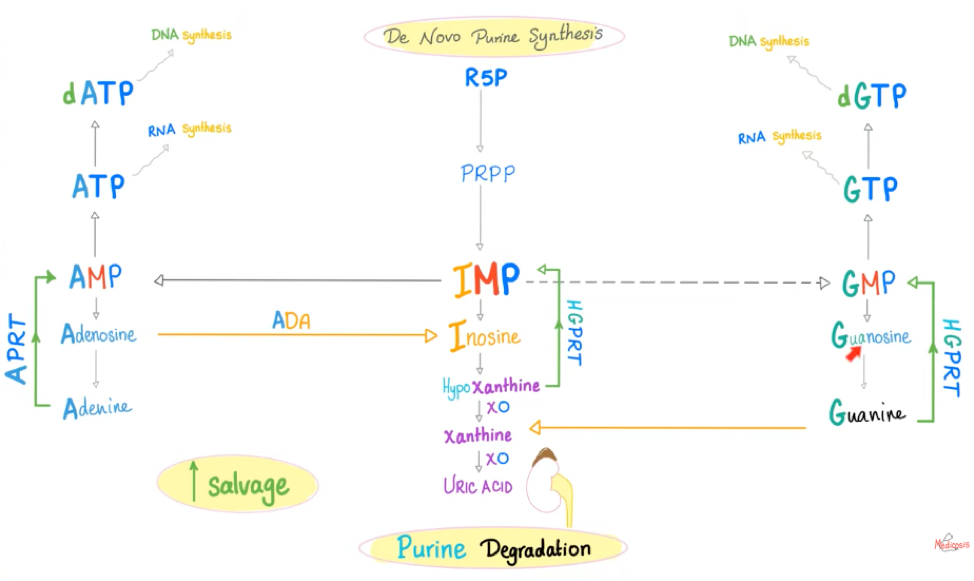
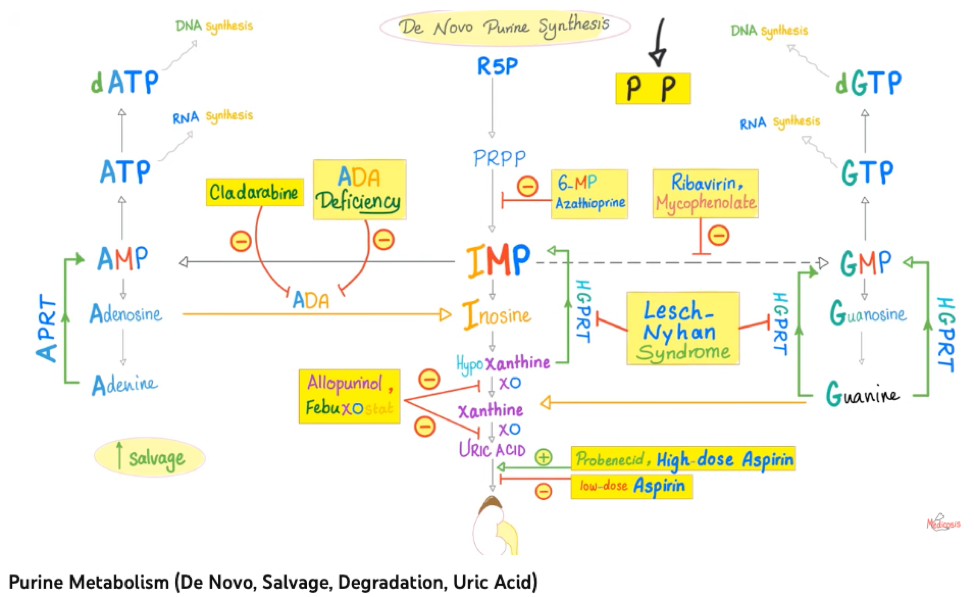
As mentioned, the imbalance between SUA production/overproduction and compromised excretion (removal) can create hyperuricemia. Overproduction can be caused by genetic abnormalities that hinder the proper creation of an enzyme known as hypoxanthine-guanine phosphoribosyltransferase (HGRPT) and over produce the enzyme phosphoribosyl pyrophosphate synthetase (PRPS or PRPP)…mouthful, right?.1(496)
These enzymes, when made correctly and in optimal amounts, manage the production and break down substances/redirect usage that would otherwise turn into SUA. These substances, from food, are known as purines; adenine and guanine (nerd fact: these molecules also help form your DNA and help make ATP…the stuff that gives you energy).1(496) Purines from food account for about one third of the body’s daily SUA production (in healthy people).5
Furthermore, the body naturally produces purines (remember they DO have important roles, in the right amounts) from glucose AND will also produce them when the body is under stress from malignancy (cancel cell growth), haematological (blood) disorders, and inflammatory diseases (obesity, diabetes, cardiovascular disease).1(496) However, when you really look close, overproduction of SUA accounts for only about 10% occurrence of elevated uric acid, while lowered excretion (removal) contributes to 90%; so hyperuricemia is mostly an issue of poor removal.1(496)
REMOVAL OF SUA
The bulk (60-70%) of SUA is actually removed (excreted) by the kidneys, and to a lesser extent, through the digestive system and resident bacteria.4 Most importantly, 90% of individuals with hyperuricemia (high SUA levels) are suffering due to impaired urinary excretion.5 Within the kidney, there are little transporters that control movement of SUA into the urine and bladder.
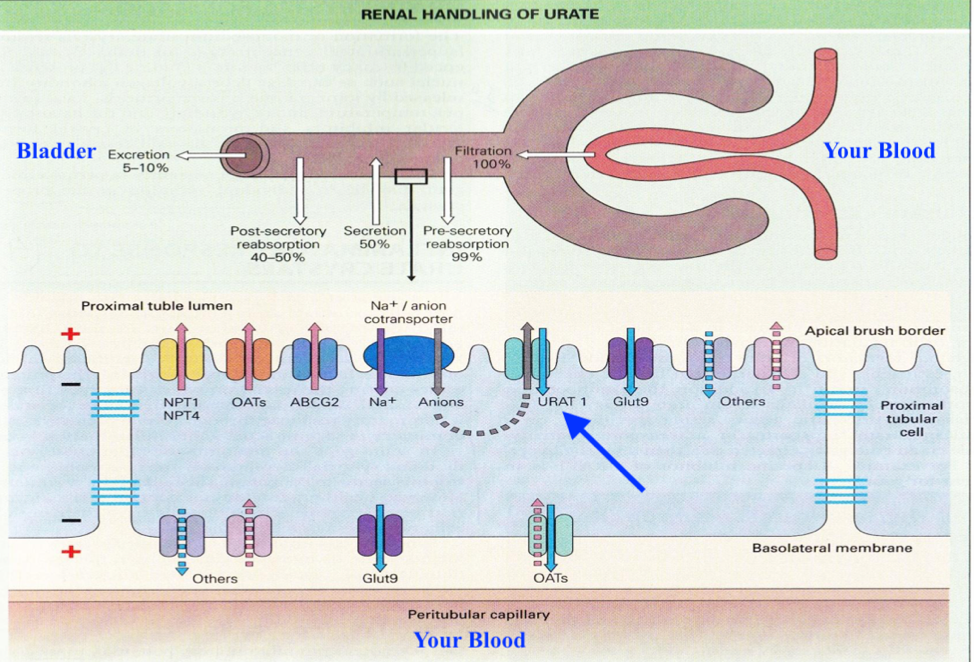
One of these transporters are called URAT1 (see pic above).6(6) When working properly, URAT1 helps pull SUA back into the body in normal amounts (called reabsorption). However, if the genes that make URAT1 have mutations, URAT1 can absorb excessive amounts of SUA back into the body; a major cause of hyperuricemia.6(6)
HOW CAN I CONTROL HYPERURICEMIA?
So far, we covered how genetic mutations can cause the overproduction and/or poor removal of SUA; factors that are out of our control. There are medications that your family physician can explore with you to manage gout if it is frequent and severe. These medications work on different pathways to limit blood levels of SUA and support excretion (see above).
WHAT ELSE CONTRIBUTES TO GOUT?
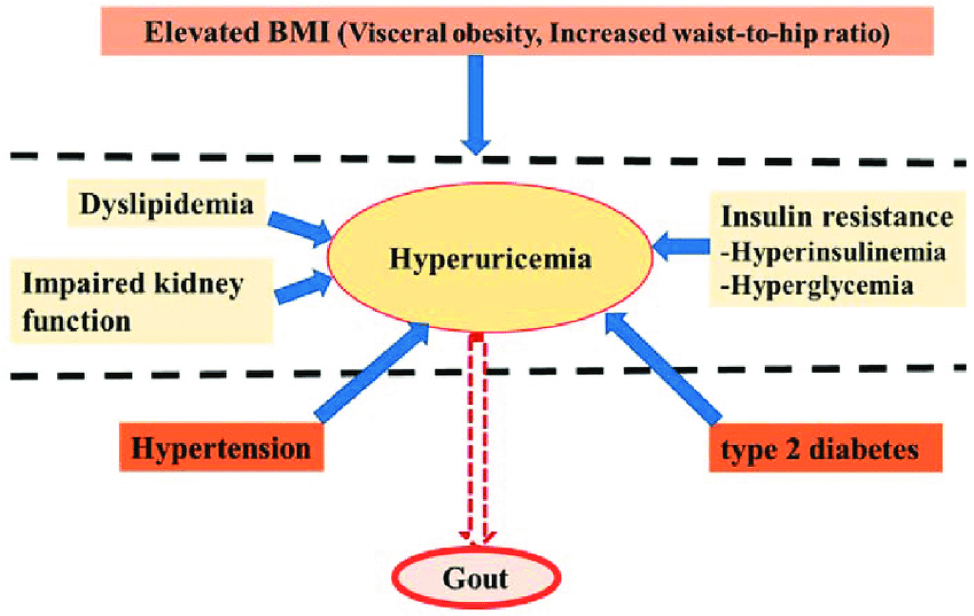
There appears to be compelling associations between hyperuricemia and other diseases (see image above).7 What seems unclear, is if hyperuricemia causes these conditions, or if the conditions cause hyperuricemia.7(10) Copur et al7(4) noted, however, that there is a well-predicted trend of hyperuricemia amongst people adopting the Western lifestyle.
A Western lifestyle is characterized as populations suffering from widespread chronic non-infectious diseases such as cardiovascular disease, diabetes, obesity, autoimmune disease, cancer, Alzheimer’s disease and several more; conditions rarely observed in non-westernized populations.8 Characteristics of Western lifestyles includes the widespread presence and consumption of processed foods as well as poor sleep and sedentary behaviour.8(2229) Please review the links below to learn more about the negative effects of the Westernized living:
LINK: Processed Food, Definition, and Healtth Consequences
LINK: Processed Foods, Cardiovascular Disease, and Insulin Resistance
LINK: Inactivity, Addictive Foods, and How They Drive Obesity
LINK: Inadequate Sleep and Health Outcomes

SUPPORT FOR HYPERURICEMIA AND GOUT
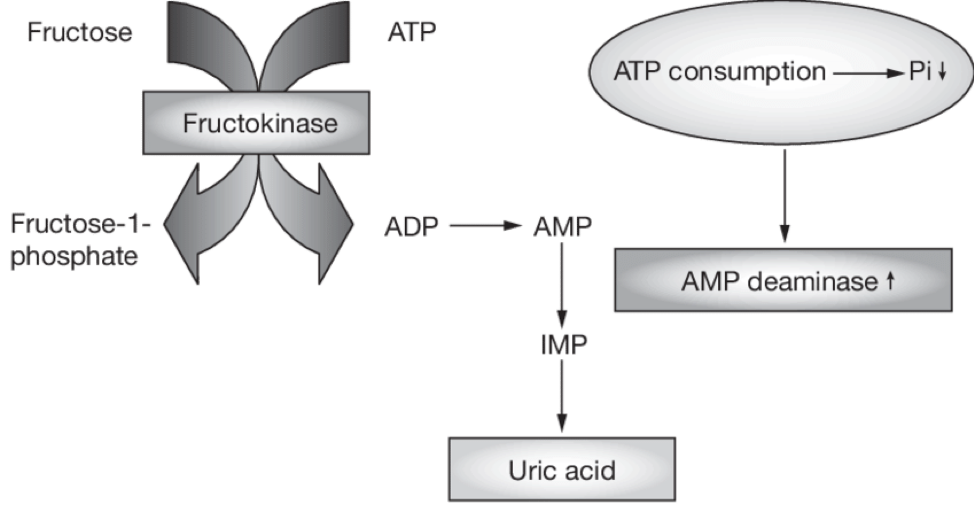
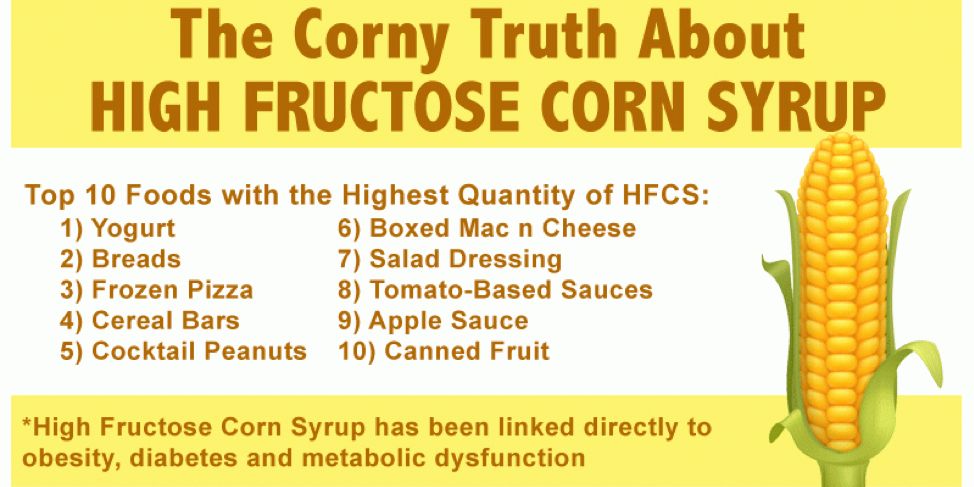
Considering there are foods rich in purines, removing and/or lowering these would make sense. Such purine-rich foods/drinks would include organ meats (liver), mussels, turkey, beer, and many more (see above image). Highly processed foods often contain high fructose corn syrup (HFCS); a substance tightly linked (temporally) to obesity, metabolic syndrome, and chronic kidney disease.9 HFCS is problematic because as it is metabolized to make/store energy, there are “leftovers” that make their way into forming uric acid (see image below).9(88)
Unfortunately, high SUA is not the only issue with HFCS. Due to the ubiquity of this sugar in the food system, and the fact it is often embedded within processed foods, many people are overconsuming this product. READ THE LABELS ON FOOD.
OTHER PROBLEMS WITH HFCS
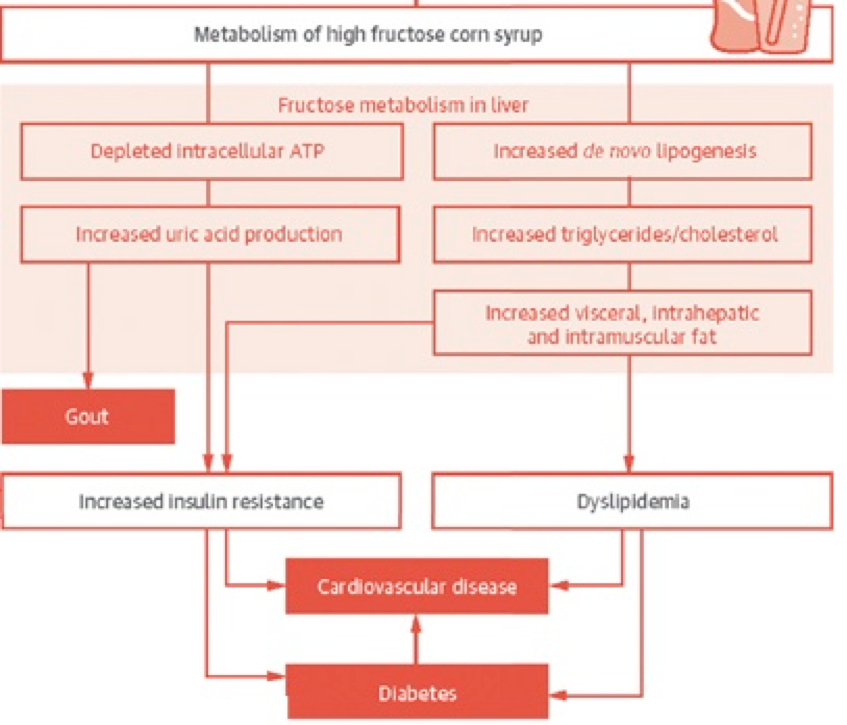
HFCS produces substances that help make energy for us. On the surface, this would appear beneficial to us, but as you have already seen, this sugar creates more problems than benefits. Another issue with HFCS is the rapid production of substrates (acetyl-CoA) used to make energy; if the body does not immediately need these substrates to make energy, they are quickly stored as triglycerides and body fat.9(88)
High triglycerides (which contributes to dyslipidemia) are not good because they can convert into very low-density lipoproteins (VLDLs), which contribute to atherosclerosis (see link below). HFCS also contributes to weight gain and obesity (the body doesn’t like to waste energy).9(88) Obesity is problematic because it drives inflammation, insulin resistance, and is implicated with the development of diabetes over time (see the image below).
LINK: Low Carbohydrate Nutrition: Managing High Triglycerides and Low
Density Lipoproteins
LINK: Omega-6 Consumption: Connections to Chronic Inflammation and Obesity
LINK: Why Processed Foods Will Make You Sick
LINK: Processed Foods, Cardiovascular Disease, and Insulin Resistance
As you can see, HFCS consumption can create obesity, cardiovascular disease, and diabetes; conditions that are also linked to hyperuricemia and gout (mentioned previously).
PUTTING IT ALL TOGETHER
So hopefully you have learned that foods rich in purines and HFCS syrup are implicated in causing gout. I also hope that you understand conditions like obesity, cardiovascular disease, diabetes can worsen/are associated with uric acid levels, and that uric acid levels can worsen/are associated with these diseases. Make sure you become aware of high purine foods, and food/drinks that contain high fructose corn syrup…then remove them.
GIVE ME THE COLE’S NOTES ON WHAT TO DO
1. Reduce processed food intake: these foods are often rich in HFCS and omega-6 (increases inflammation). Elect to consume more leafy vegetables instead, and choose proteins that are low in purines. If you have weight on, also consider gentle reduction in low purine carbohydrates as well, to help lower body fat.
2. Exercise daily: This is a great way to help manage obesity, cardiovascular disease, and diabetes (associated with gout). See the link below for more information…
LINK: Obesity and Metabolic Syndrome: Management and Prevention
3. Get optimal sleep every night: Poor sleep dysregulates glucose metabolism, increases hunger, and contributes to inflammation, diabetes, heart disease, and hypertension.
LINK: Processed Food, Poor Sleep, and Low Grade Chronic Inflammation
LINK: Improving Sleep Quality and Duration
4. Stay hydrated: low water intake and excessive sweating has been shown to increase concentrations of uric acid which could trigger an episode of gout.10
LINK: Mild Chronic Dehydration and Implications
LINK: Environmental Conditions, Hydration, and Fluid Content
5. Vitamin C supplementation: it is possible that extra vitamin C may help control uric acid levels. Kakutani-Hatayama et al10(327) noted a decreasing trend in sample of 1387 males, whereby serum uric acid levels dropped as more vitamin C was ingested. Another study (randomized control trial) indicated that 500 mg/day of vitamin C for 3 months reduced uric acid by increasing removal through the kidneys.10(327)

CONCLUSIONS
Gout is one of the most well studied and characterized forms of arthritis affecting up to 4% of the population (2.68 per 1000 people). Flare-ups can be quite excruciating, so management and prevention is key. In addition to prescription medications that your family physician may recommend, I hope you now see that there are several interventions that can be used manage/prevent gout attacks. If you choose to implement these steps, these food and lifestyle changes will not only help keep your joints happy; they will also support your overall health, performance, and longevity. Good luck!
References
1. Ragab G, Elshahaly M, Bardin T. Gout: An old disease in new perspective – A review.J Adv Res. 2017;8(5):495-511. doi:10.1016/j.jare.2017.04.008.
Towiwat P, Chhana A, Dalbeth N. The anatomical pathology of gout: A systematic literature review. BMC Musculoskelet Disord. 2019;20(1):1-14. doi:https://doi.org/10.1186/s12891-019-2519-y .
3. Gout. Mayo Clinic. Updated November 16, 2022. Accessed December 6, 2023. https://www.mayoclinic.org/diseases-conditions/gout/symptoms-causes/syc-20372897.
4. Bobulescu IA, Moe OW. Renal transport of uric acid: Evolving concepts and uncertainties.Adv Chronic Kidney Dis. 2012;19(6):358-371. doi:10.1053/j.ackd.2012.07.009.
5. George C, Leslie SW, Minter DA. Hyperuricemia. In: StatPearls. Treasure Island (FL): StatPearls Publishing. Updated October 14, 2023. Accessed December 10, 2023.
6. Sun HL, Wu YW, Bian HG, et al. Function of uric acid transporters and their inhibitors in hyperuricemia. Front Pharmacol. 2021;12(667753):1-15. doi: 10.3389/fphar.2021.667753.
7. Copur S, Demiray A, Kanbay M. Uric acid in metabolic syndrome: Does uric acid have a definitive role?Eur J Intern Med. 2022;103:4-12. doi:10.1016/j.ejim.2022.04.022.
8. Kopp W. How Western diet and lifestyle drive the pandemic of obesity and civilization diseases.Diabetes Metab Syndr Obes. 2019;12:2221-2236. doi:10.2147/DMSO.S216791.
9. McChesney, Monica J.Relationship between high-fructose corn syrup, uric acid, and metabolic syndrome. J Pediatr Surg Nurs. 2016;5(4):88. doi:10.1097/JPS.0000000000000115.
10. Kakutani-Hatayama M, Kadoya M, Okazaki H, et al. Nonpharmacological management of gout and hyperuricemia: Hints for better lifestyle.Am J Lifestyle Med. 2015;11(4):321-329. doi:10.1177/1559827615601973
-Michael McIsaac

