
Understanding the tissue healing process, without medical intervention, serves as a baseline to determine and compare the efficacy of modern-day therapeutic techniques. As a means of appreciating the undisturbed process of tissue healing, the following will examine the research of Frank, Woo, Amiel, Harwood, Gomez, and Akeson (1983) as it relates to medial collateral ligament (MCL) healing, after complete rupture.
Frank et al. (1983) endeavored to determine if there were biochemical, histological, and biomechanical changes within a healed MCL after deliberate rupturing of the ligament. Such an experiment was carried out by way of animal testing; 64 New Zealand White rabbits were selected, whereby 16 were designated as normal controls (NORMAL). The remaining 48 rabbits underwent 2 procedures; the MCL on the right leg was designated as the experimental leg (EXP), and the MCL on the left leg was designated as the sham operated controls (SHAM). The EXP had the MCL completely ruptured, and the MCL was simply exposed in the SHAM, with no rupturing. Observation and analysis was performed between NORMAL, SHAM, and EXP conditions at 10 days, 3 weeks, 6 weeks, 14 weeks, and 40 weeks by way of biochemical, histological, and biomechanical analysis (Frank et al., 1983).

Histologically, the EXP began healing via scar tissue formation as early as the 10-day point, up to and including, the 40-week point. The SHAM was initially swollen and watery up to the 3-week point but regained a normal appearance thereafter (Frank et al., 1983). Representative sections that were closely examined confirmed gross observations; EXP exhibited inflammatory cells (indicating the 1rststage of connective tissue repair), which slowly decreased up to the 3-week point, with an increase in fibroblast activity (a marker of the 2ndstage of repair) in the same period (Frank et al., 1983).
Biochemically, water content (a component of ground substance, which is involved in connective tissue formation) was the highest in EXPs compared to SHAMS and NORMALS in the 10 day and 3 week points (Delforge, 2002; Frank et al., 1983). Glycosaminoglycans (GAGs- another constituent of ground substance) were also significantly elevated during all testing points. However, GAGs never matched the same number found in NORMALs (Delforge, 2002; Frank et al., 1983). Collagen content (a predominant contributor to tensile strength in connective tissue) was low compared to NORMAL and SHAM within the 10 day mark. However, EXP collagen content slowly increased thereafter but never matched NORMAL and SHAM conditions (Frank et al., 1983). Collagen quality was also poor. Such quality is determined the ratio of intermolecular reducible Schiff base crosslinks dihydroxylysinorleucine (DHLNL) and hydroxylysinorleucine (HLNL); EXP had low DHLNL and HLNL ratios compared to NORMAL and SHAM.
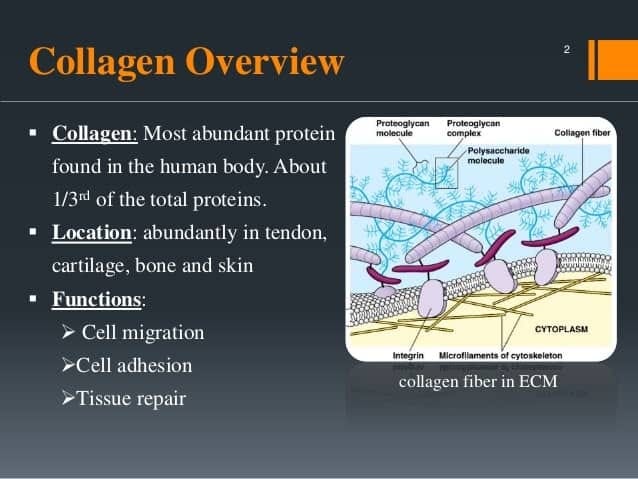
The aforementioned ratios also helped determine the maturity of collagen, which was found to be in its immature state for many weeks in the EXP (Frank et al., 1983). Moreover, type 3 collagen was higher in the EXP than NORMAL and SHAM, indicating a weaker form of collagen in the scar formation (Frank et al., 1983). Not surprisingly, such qualities negatively affected the tensile strength in EXP compared to SHAM and NORMAL; EXP persistently scored lower on tensile strength tests up to and including the 40 week point (Frank et al., 1983).

In conclusion, such knowledge indicates that, although ligaments can repair themselves over the course of time, less-than-ideal histological and biochemical changes negatively affect the biomechanics/tensile strength of the EXP. Finally, the work of Frank et al. (1983) should provide a baseline, and inspire the implementation of therapeutic interventions that optimize the aforementioned healing process.
References
Delforge, G. (2002). Musculoskeletal trauma; Implications for sports injury management. Champaign, IL: Human Kinetics.
Frank, C., Woo, L. Y., Amiel, D., Harwood, F., Gomez, M., & Akeson, W. (1983). Medial collateral ligament healing. A multidisciplinary assessment in rabbits. American Journal of Sports Medicine, 11(6), 379-389.
-Michael McIsaac
