
Metabolic syndrome (MS) is a condition defined as a constellation of risk factors which induce other disease states such as stroke, cardiovascular heart disease (CVD), and diabetes.1 Said biomarkers/risk factors include high blood pressure, decreased high-density lipoprotein cholesterol (HDL-C), elevated low-density lipoprotein cholesterol (LDL-C), abdominal obesity, impaired fasting glucose, and elevated fasting triglycerides.2,3
Therefore, proper interpretation, and interventions for, the aforementioned markers is paramount. As such, the following will consider a hypothetical blood chemistry panel, and an organic acids test, which suggest metabolic syndrome/diabetes as well as nutritional/supplemental solutions for the same.
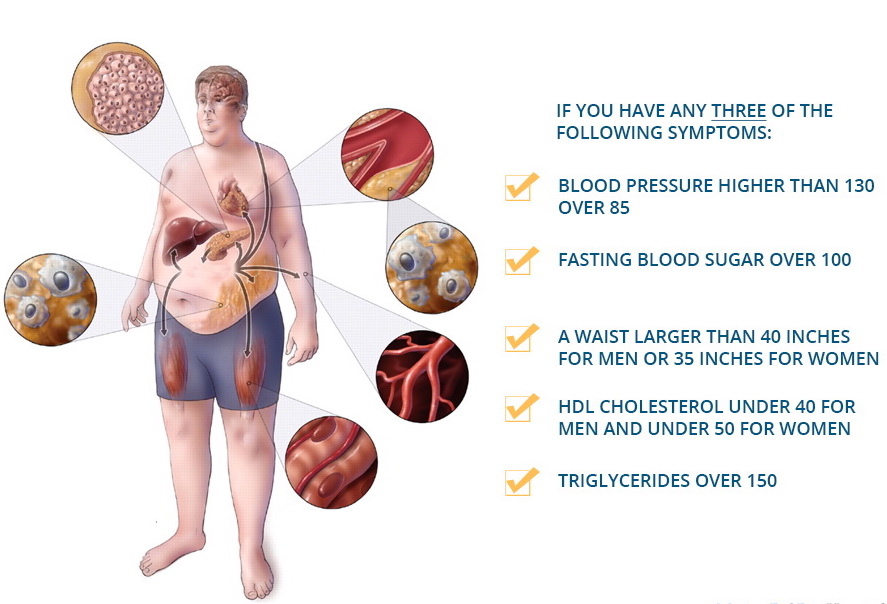
If an individual’s test results indicate the presence of at least 3 risk factors, MS is indicated.4 Thus, if a client were to present with elevated fasting glucose of 112 mg/dL, elevated triglycerides of 153 mg/dL, and LDL-C of 120 mg/dL, MS would likely be present. Although such markers are relevant and satisfy the diagnosis of MS, it is also imperative to consider all markers that indicate aberrations in homeostasis.
For example, the hypothetical client also presents with elevated hemoglobin A1C (HBA1C) of 6.2%, elevated fasting insulin of 28.1 uIU/ml, elevated cholesterol/HDL ratio of 4.4, and elevated sodium of 145 mmol/L. Such markers suggest insulin resistance (i.e., elevated insulin), elevated glucose over 3 months (i.e., HBA1C), and dyslipidemia (i.e., elevated cholesterol/HDL ratio).5 Said markers then, as a whole, places the client at increased risk of not only diabetes (high insulin/high glucose/high HBA1C), but also CVD (elevated LDL-C, high cholesterol/HDL ratio, high triglycerides, high sodium).5(314-315)

Organic tests also suggest drivers behind the client’s risk factors for MS. Arachidonic acid (AA), a type of omega-6 fatty acid, is elevated at 2.9 uM while linoleic acid (LA)/Dihomo-γ-linolenic acid (DGLA) ratios are also high measuring at 34 uM. Other organic acid tests suggest poor metabolism of fats (elevated suberate and adipate), poor metabolism of carbohydrates (elevated L-lactate), B vitamin deficiencies (low alpha-ketoisocaproate), liver detoxification issues (high orotate), mitochondrial energy metabolism issues (elevated citrate, alpha-ketoglutarate, fumarate, malate, hydroxymethylglutarate), gut dysbiosis (i.e., elevated benzoate, hippurate, indican, D-lactate) and elevated exposure to toxins (elevated 2-methylhippurate).6 Having considered both blood and organic acid markers, the following will present solutions to mitigate MS risk factors and additional interventions to improve gut health and liver function.
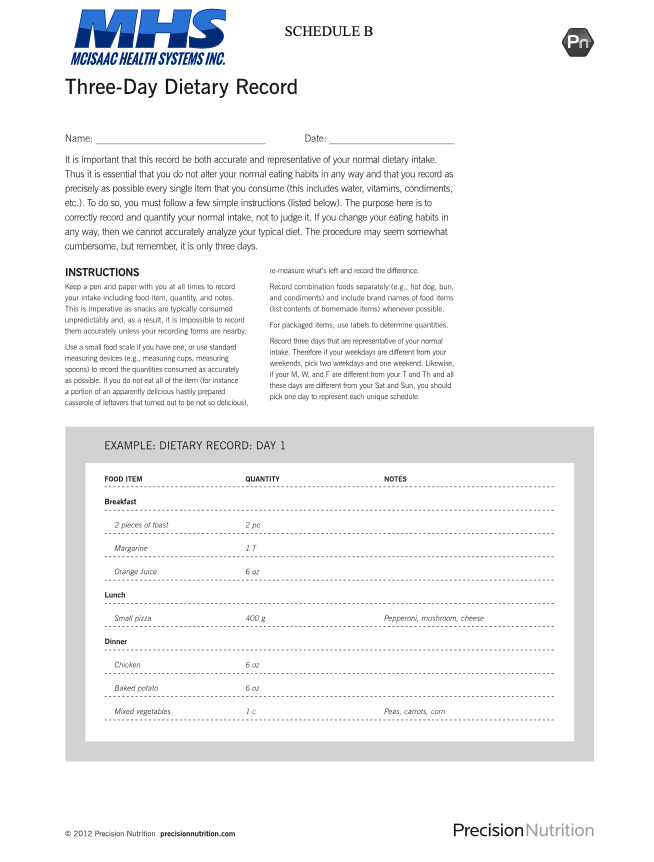
This author would first suggest a 3-day dietary record to gain further insight into the client’s nutritional proclivities. It is likely that the client is consuming larger amounts of refined carbohydrates, as such foods tend to elevate blood glucose, triglycerides, LDL-C, and insulin; markers of MS and diabetes.7
Additionally, the client is ingesting pro-inflammatory fatty acids (omega-6) that contribute to inflammation and heart disease, as seen in elevated arachidonic acid levels.6(274) Other fatty acids contributing to inflammation also include elevated LA/DGLA ratios, of which are high in the client’s markers; LA is an omega-6 fatty acid and precursor to AA, while DGLA is an omega-6 fatty acid with anti-inflammatory properties.6(300),8
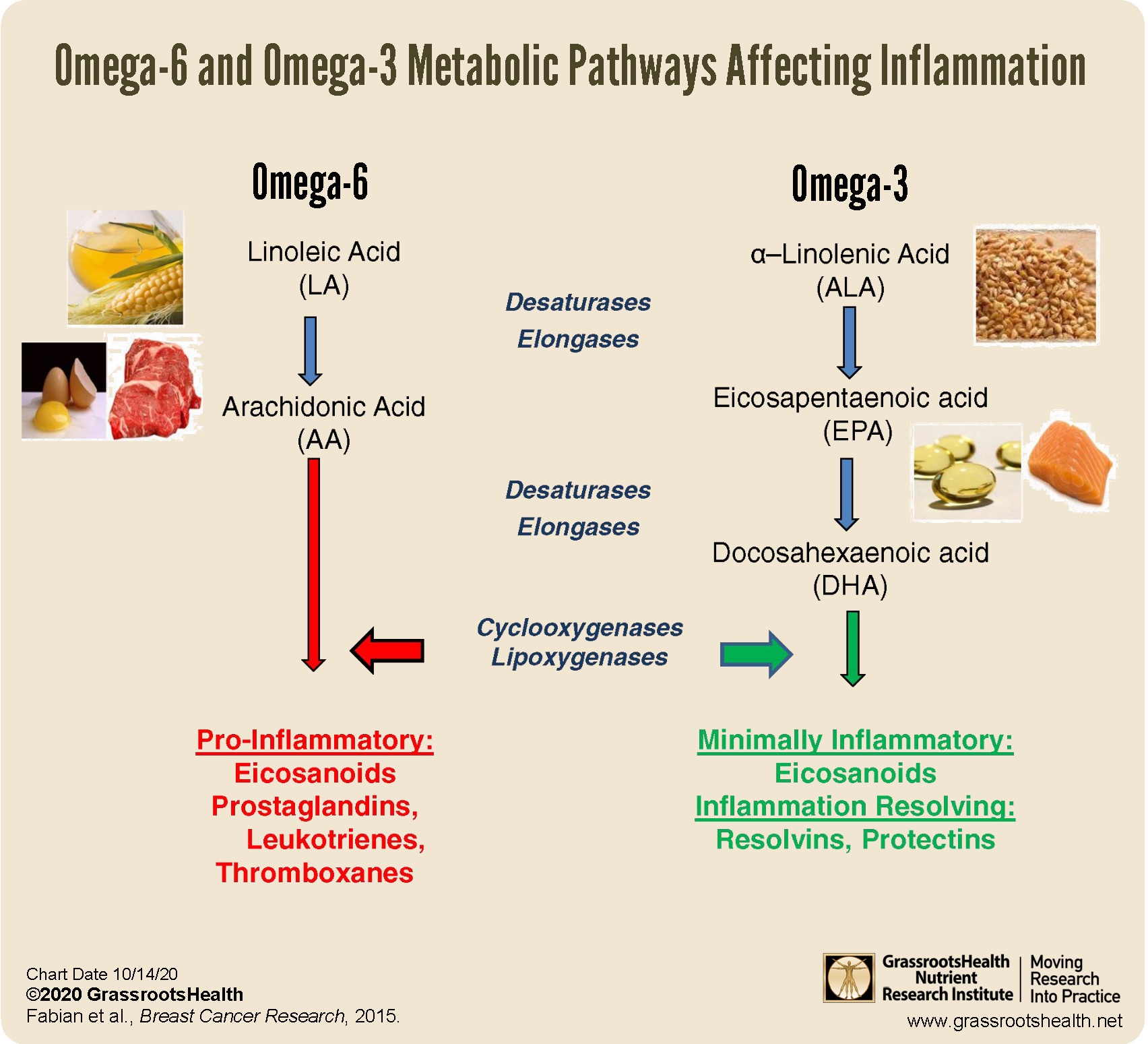
Reducing omega-6 fatty acids, substances found in abundance amongst processed foods and refined carbohydrates, should help reduce the aforementioned inflammatory LA and AA markers.9 Furthermore, such a reduction should help attenuate and improve the LA/DGLA ratio, which could be further optimized by increasing dietary DGLA; such could be achieved by increasing consumption of borage and evening primrose.6(300)
Eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) are not truly deficient in the client’s blood panel, however, they are trending towards such a state. As such, this author would encourage weekly consumption of fish in addition to supplemental omega-3 in the range of at least 3000 mg/day until markers reach optimal levels.10 Said fatty acids would also help reduce triglycerides and improve LDL profiles.11

Although reducing processed carbohydrates/omega-6 rich foods and increasing anti-inflammatory omega-3 fatty acids are likely to have the most prominent impact upon the client’s health and panels, other interventions can play a supportive role. For example, the client exhibited aberrations in carbohydrate and fat metabolism as outlined previously. Reducing starchy carbohydrate load should help the former by reducing its prevalence in the diet.
The latter could be attenuated by increasing carnitine levels, which is rich in meats but may also need to be supplemented. If required, 1000-2000 mg/day would be indicated.10(366) B-vitamin deficiencies can be mitigated by increasing dark leafy green vegetable consumption and by supplementation. Low alpha-ketoisocaproate is indicative of low B1/B1/B3/B5, thus a B-complex vitamin containing the same may also be helpful to include lipoic acid at 100 mg/day.6(322, 341)

Liver detoxification, indicated by high orotate, occurs when there are deficient levels of arginine (used to facilitate removal of NH4/ammonia) within the body.6(364) As such, consumption of arginine-rich foods including meat proteins, nuts/seeds, and supplementation of approximately 1000-3000 mg/day can improve liver function.6(323) Magnesium also facilitates the removal of NH4 from the liver and is often implicated in high orotate levels.6(364) Thus, analyzing red blood cell magnesium levels to ensure optimal levels might be indicated.10(192)

Compromised mitochondrial energy production, indicated on the client’s organic acids test, can be improved by arginine supplementation (1000-3000 mg/day), B-complex (3/day), lipoic acid (100 mg/day), CoQ10 (50 mg x 3/day), and magnesium (500 mg/day).6(322)
Gut dysbiosis markers outlines in the previous section could be controlled by increased glycine (2000-5000 mg/day), B5 (100 mg x 3/day), and digestive aids to include betaine and digestive enzymes.6(323) Finally, avoidance of xylene exposure, indicated by elevated 2-methylhippurate, can be achieved by avoidance of paint thinners, fuel/exhaust, industrial degreasers and solvents.6(363) Finally, removal of said toxins can be supported by glycine (2000-5000 mg/day) and B5 (100 mg x 3/day).6(323)
In conclusion, MS is a condition defined by a constellation of risk factors which induce other disease states such as stroke, cardiovascular heart disease (CVD), and diabetes. Early detection of signs and symptoms, in addition to monitoring blood and urine biomarkers, serve as vital first steps towards mitigation/remission of such diseases. Ultimately, reducing foods which worsen glucose, insulin, and inflammatory levels are likely to produce the greatest meaningful changes. However, concomitantly addressing nutrient deficiencies that inhibit detoxification/energy production/digestion/absorption, and avoidance of environmental exposures to toxins, will further support health, homeostasis, and overall quality of life.
References
1. Agyemang-Yeboah F, Eghan BAJ, Annani-Akollor ME, et al. Evaluation of metabolic syndrome and its associated risk factors in Type 2 diabetes: A descriptive cross-sectional study at the komfo anokye teaching hospital, Kumasi, Ghana.Biomed Res Int. 2019; doi:https://doi.org/10.1155/2019/4562904. 2. Lopez-Huertas E. The effect of EPA and DHA in metabolic syndrome patients: A systematic review of randomized controlled trials. Br J Nutr. 2012;107(s2):1185-1194. doi:https://doi.org/10.1017/S000711451200157.
3. Marshall JC, Dunaif, A. Should all women with PCOS be treated for insulin resistance? Fertil Steril.2012;97(1):18-22.doi:10.1016/j.fertnstert.2011.11.036.
4. Metabolic Syndrome. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/diagnosis-treatment/drc-20351921. March 14, 2019. Accessed January 28, 2020.
5. Reisner EG, Reisner HM. An Introduction to Human Disease: Pathology and Pathophysiology Correlations. 10th ed. Burlington, MA: Jones & Bartlett Learning; 2017.
6. Lord RS, Bralley, JA. Laboratory Evaluations for Integrative and Functional Medicine. 2nd Duluth, GA: Genova Diagnostics; 2012.
7. Sweazea KL. Compounding evidence implicating Western diets in the development of metabolic syndrome.Acta Physiol. 2014;211(3):471-473. doi:10.1111/apha.12303.
8. Rett BS, Whelan J. Increasing dietary linoleic acid does not increase tissue arachidonic acid content in adults consuming Western-type diets: A systematic review. Nutr Metab. 2011;8(36):1-15. doi:10.1186/1743-7075-8-36.
9. Ilich JZ, Kelly, OJ, Kim Y, et al. Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Arh Hig Rada Toksikol. 2014;65(2),139-148. doi: 10.2478/10004-1254-65-2014-2541.
10. Kohlstadt I. Advancing Medicine with Food and Nutrients. 2nd ed. London, NY: CRC Press; 2012.
11. Lopez-Huertas E. The effect of EPA and DHA in metabolic syndrome patients: A systematic review of randomized controlled trials. Br J Nutr, 2012;107(s2):1185-1194. doi: https://doi.org/10.1017/S0007114512001572.
-Michael McIsaac
