
Metabolic syndrome (MS) is a condition defined by a constellation of associated risk factors that increase a person’s chances of contracting stroke, cardiovascular disease (CVD), and diabetes (Chen, Yen, Huang, Lee, Hsia, & Lin, 2012). Said risk factors include: abdominal obesity (waist circumference 102 cm for males, 88cm for females), impaired fasting glucose (≥6.1 mmol/L), elevated fasting triglycerides (≥1.7mmol/L), decreased high-density lipoprotein cholesterol (HDL-C, <1 mmol/l for males, <1.3 mmol/L for females), and high blood pressure (BP ≥130/85 mm Hg) (Lopez-Huertas, 2012). Thus, any interventions that help control said biomarkers should help reduce chances of stroke, cardiovascular disease, and diabetes. One such intervention includes fish oil supplementation. As such, the following will consider its role in MS and reducing associated risk factors, with specific emphasis on low density lipoproteins and triglycerides.
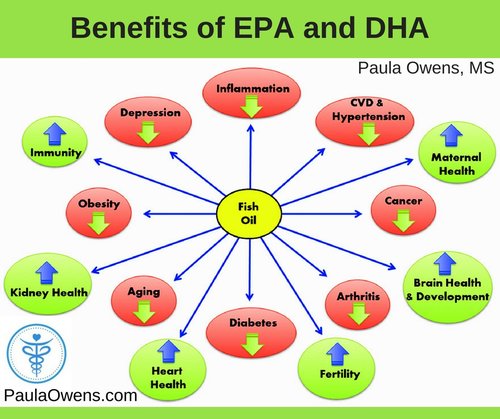
Fish oil is made primarily of very long-chain polyunsaturated fatty acids, colloquially known as omega-3 fatty acids (n-3), made primarily of eicosapentaenoicacid (EPA) and docosahexaenoic acid (DHA) (Lopez-Huertas, 2012). Evidence suggests that n-3 supplementation reduces plasma triglyceride (TG) levels and thereby the risk of CVD. Other potential mechanisms cited by Lopez-Huertas (2012) may include lowering of blood pressure, reduced thrombotic (blood clot formation) tendency, anti-inflammatory and antiarrhythmic effects, improved vascular endothelial function, increased plaque stability, increased paraoxonase levels and improved insulin sensitivity. The following sections will explore n-3 supplementation and its affects upon low-density lipoprotein (LDL) particle size in greater detail.
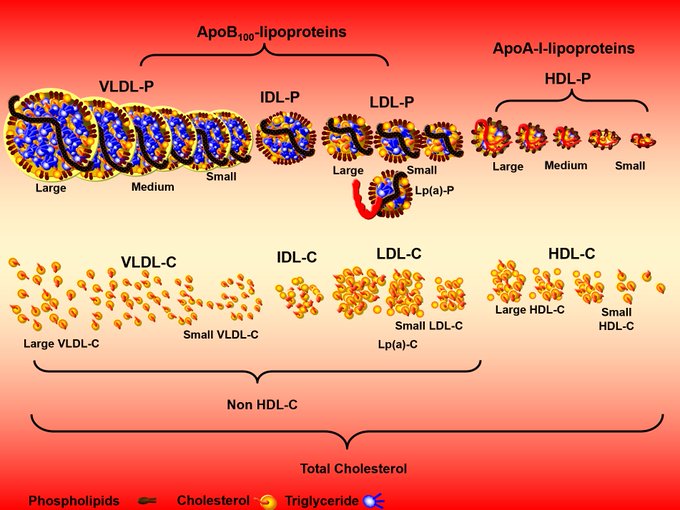
In my last post, I covered the strong associations and mechanisms of small dense low-density lipoproteins (SDLDL) and CVD risk. Lopez-Huertas (2012) indicated that his systematic review of 17 randomized controlled trials (covering associations between n-3 supplementation and MS biomarkers) indicated LDL particle size is an important predictor of cardiovascular events and progression of CVD. The researcher also indicated that SDLDL were pro-atherogenic and have been associated with obesity, insulin resistance, high blood TG, and oxidative stress (Lopez-Huertas, 2012). Supplementation of MS patients with N-3 consistently reduced the percentage of SDLDL particles in favour of the large, buoyant, less atherogenic. Such reduction is thought to reduce cardiovascular risk (Lopez-Huertas, 2012). The following will explore potential mechanisms behind reduced SDLDLs.
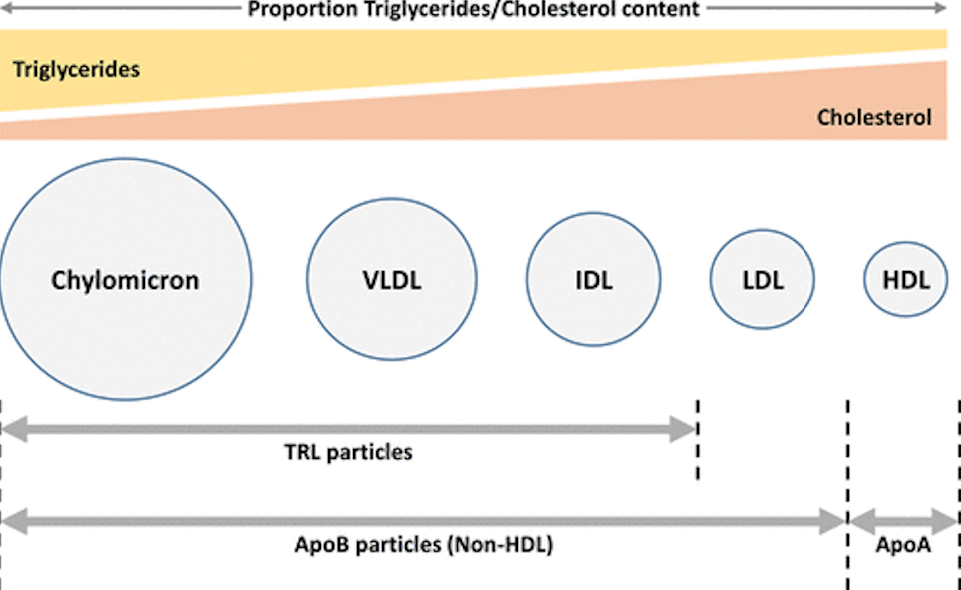
Lopez-Huertas (2012) stated that concentrations of SDLDLs are regulated by the presence of plasma TGs. In MS, slow clearance of TG from triglyceride rich lipoproteins (TRLs) such as chylomicrons (CMs) and very low-density lipoproteins (VLDL) allows for longer periods of circulating TG, which can directly affect the composition (particle size) of LDL. Increased transfer of TG to SDLDL via cholesterol ester transfer protein (a plasma protein that facilitates the movement of triglycerides between lipoproteins) during neutral-lipid exchange and subsequent hydrolysis of LDL-TG by lipases results in an abundance of SDLDL. Suppression of TG production in the liver by EPA and reduction of CETP activity may explain the beneficial shift of LDL composition mentioned in the previous section (Lopez-Huertas, 2012). As little as 1+ grams/day of EPA/DHA can reduce plasma TGs as high as 25% (Lopez-Huertas (2012).
In conclusion, MS is a condition affecting 10-25% of individuals globally (Lopez-Huertas (2012). Although this review of MS and n-3 interventions is not exhaustive (exercise, improved sleep, other nutritional interventions reduce MS risk factors), said information regarding beneficial effects of n-3 remains relevant; n-3 supplementation helps reduce serum TG concentrations and increases LDL particle size (Lopez-Huertas (2012). Due to n-3’s cost-effectiveness and ease of use, said fatty acid can become part of an overall strategy to improve blood lipids and other biomarkers associated with MS.
References
Chen, S. J., Yen, C. H., Huang, Y. C., Lee, B. J., Hsia, S., & Lin, P. T. (2012). Relationships between inflammation, adiponectin, and oxidative stress in metabolic syndrome. Plos One, 7(9), e45693.
Lopez-Huertas, E. (2012). The effect of EPA and DHA in metabolic syndrome patients: A systematic review of randomized controlled trials. British Journal of Nutrition, 107(s2), 1185-1194.
-Michael McIsaac
