
Migraines are a form of headache which lasts between 4-72 hours and presents with, at minimum, two of the following: moderate/severe pain intensity, unilateral localisation, further aggravation by movement, pulsating feeling, nausea, vomiting, photophobia (light sensitivity), and phonophobia (sound sensitivity).1 Migraines are deemed chronic when lasting 4 hours a day/in excess of 15 days per month, and are considered disabling and economically burdening.1(9),2 Therefore, interventions to manage the symptoms and underlying causes are paramount. As such, the following will consider the same.

Weatherall2(116) stated that migraines are the most common of cause severe and recurrent headaches. Furthermore, such headaches are experienced by over 10% men and 20% of women.2(116) Finally, migraines tend to have a genetic origin, yet individual attacks can be triggered by external and/or internal influences.2(116) As such, the latter has the potential to be modified by both nutritional and lifestyle interventions. The following will consider the same.
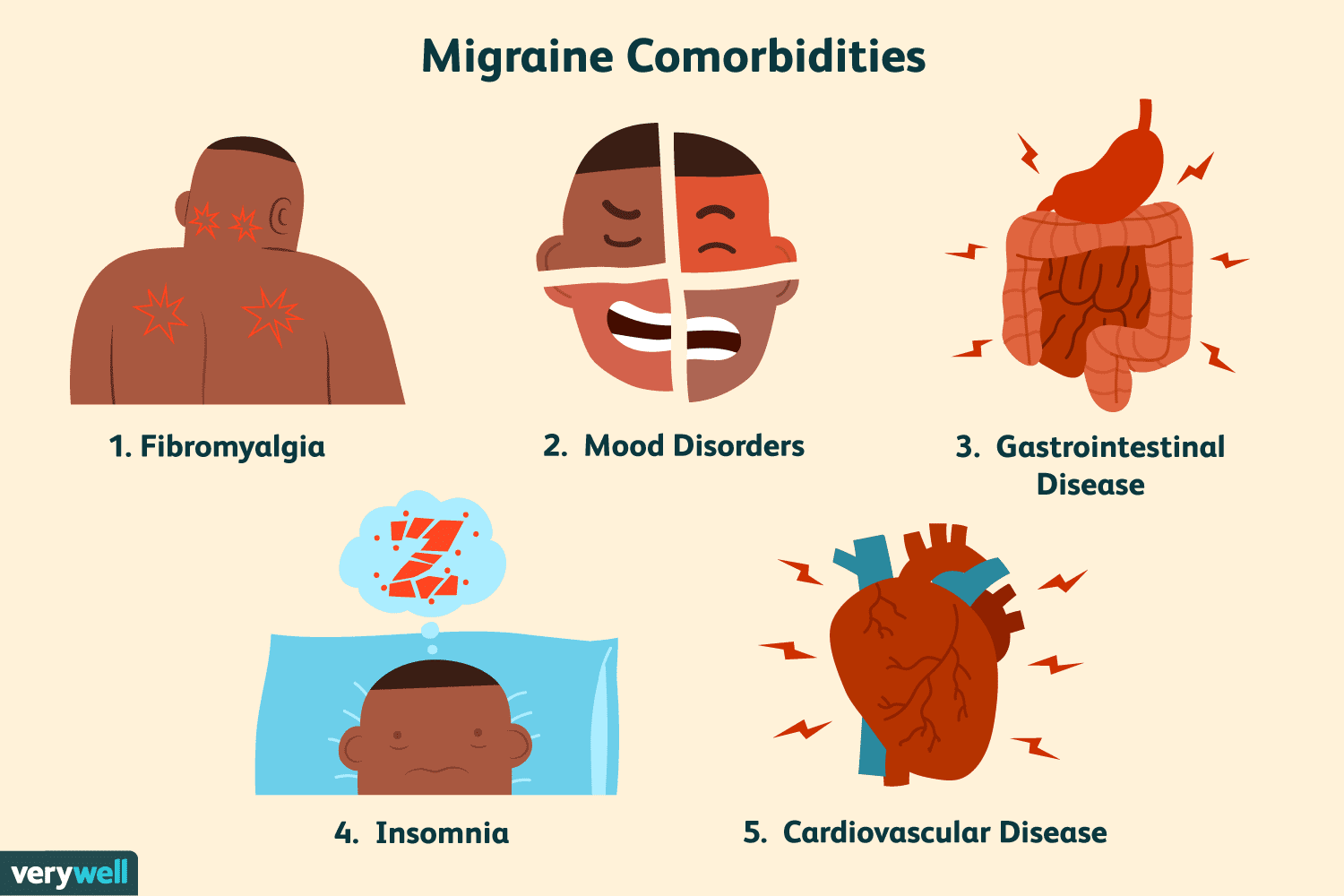
Weatherall2(119) noted that migraine sufferers frequently present with other problems that exacerbate said headaches. Such problems could include depression, other pain syndromes such as localized pain in the head/neck, fibromyalgia, conditions that create metabolic strain such as sleep apnea or postural orthostatic tachycardia syndrome, and anxiety.2(119) If an individual has a stressful life/work schedule, such a condition would likely exacerbate migraine frequency and intensity.
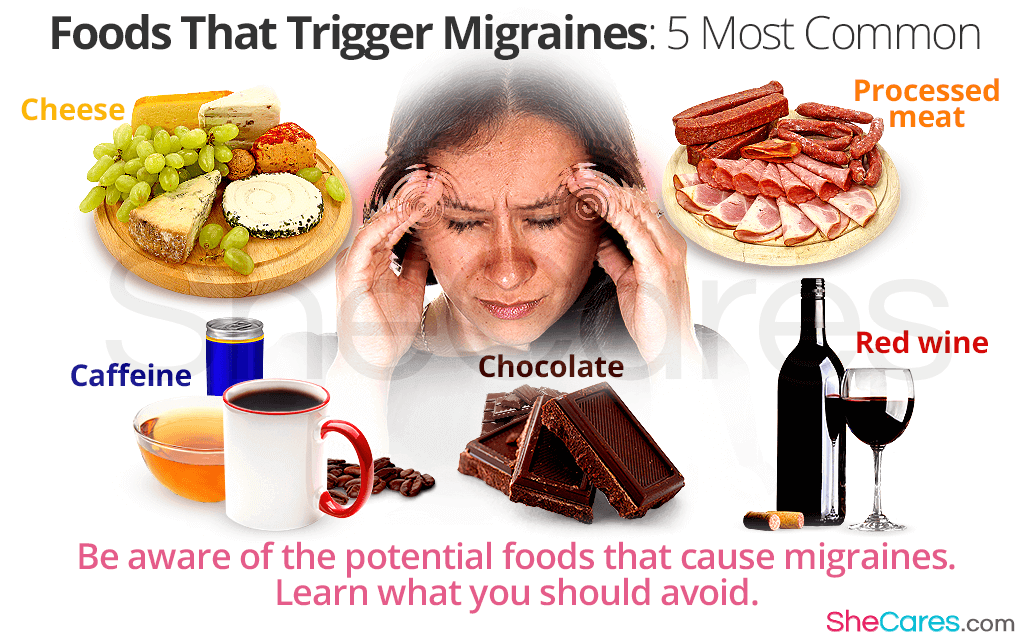
In addition to psychological stress and other pain syndromes, the most common food triggers which induce migraines would include are chocolate, cheese, alcohol, caffeine, monosodium glutamate, and aspartame.3 In addition to environmental factors, chronic diseases, premenstrual syndrome, hypertension, pregnancy, and/or obesity could be causes and triggers of pain.3(45) Thus, the development of migraines are multifactorial and can emanate from lifestyle, nutritional, and chronic disease states.

Interventions to help manage the presence and severity of migraines could include removal of food triggers via allergy testing.3(48) Although research has supported that migraine attacks developed due to food allergy, the role of the interaction between migraine and allergy and the role of IgE (a measure of the immune response) mediated allergic mechanisms in pain production are still debated.3(48) IgE should be explored when considering elimination diets for patients with migraine based on food allergy; Ozturan et al3(48)indicated that specific diets have been shown to reduce migraine attacks. However, the IgG response (another measure of immune response) generally develops more slowly. Other interventions to help manage migraines include maintaining optimal sleep hygiene, performing relaxation and breathing exercises, consuming adequate amount of daily fluid, and maintaining a social life.3(49)
In conclusion, migraines are a form of headache lasting between 4-72 hours and can present with moderate/severe pain intensity, unilateral localisation, further aggravation by movement, a pulsating feeling, nausea, vomiting, photophobia (light sensitivity), and phonophobia (sound sensitivity). Although migraines and are considered disabling and economically burdening, simple steps such as relaxation techniques, avoidance of triggering foods, enhancing sleep hygiene, and maintaining adequate hydration can help manage, and possibly lessen, the severity and frequency of migraine episodes.
References
1. Schellack N, Magongwa N, Makola F. Migraine headaches: A brief overview. Prof Nurs Today. 2019;23(3):9-12.
2. Weatherall MW. The diagnosis and treatment of chronic migraine. Ther Adv Chronic Dis. 2015;6(3):115-123. doi:10.1177/ 2040622315579627.
3. Ozturan A, Sanlier N, Coskun O. The relationship between migraine and nutrition. Turk J Neurol. 2016;22(2):44-50. doi:10.4274/tnd.37132.
-Michael McIsaac
