
The nervous system is a platform, which connects to, and communicates with, all tissues, organs, and systems of the human body. Any form of breakdown within such a system can compromise signal transmission, and ultimately, function within the tissues and organs it communicates with. As a means of appreciating such a system, the following will consider a neurological disorder known as multiple sclerosis (MS), in addition to its etiology, symptoms, manifestations, and treatment.
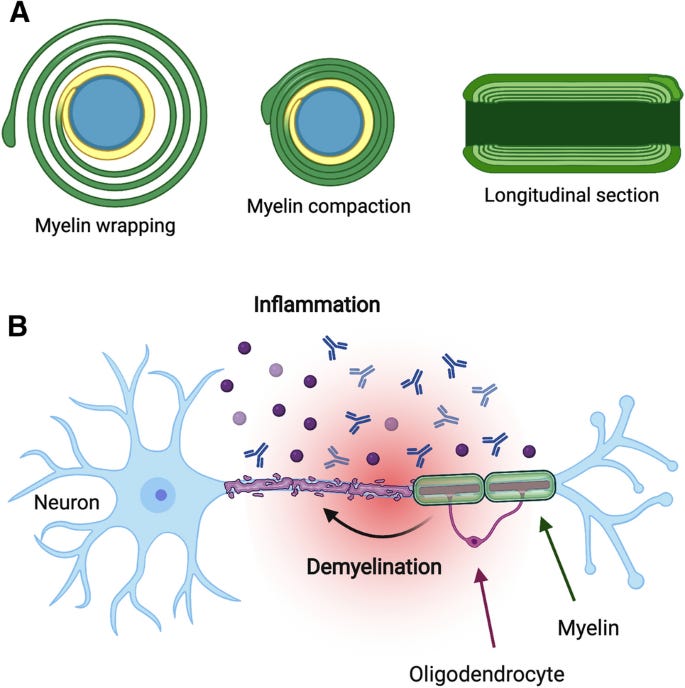
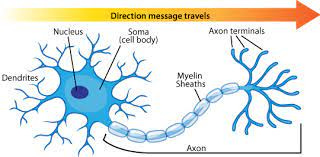
The central nervous system (CNS) consists of the brain, the brain stem, the cerebellum, and the spinal cord, which are all enveloped by membranes known as meninges (Reisner & Reisner, 2017). Within each of the constituents listed above is the neuron; a nerve cell, which delivers electrical impulses between other neurons and towards (efferent), and from (afferent), tissues and organs in the body (Reisner & Reisner). The neuron is enveloped and insulated by a myelin sheath; a fatty white substance, which helps expedite the rate of action potential transmission along the axon (connects two ends of the neuron). Thus, any compromise within the myelin sheath negatively affects it ability to efficiently communicate with other systems in the body. MS is a chronic autoimmune disease, which progressively degenerates the nerve fibers of the brain and spinal cord (Reisner & Reisner, 2017).
Such lesions randomly develop in multiple regions upon the myelin sheaths of the neuron, and the immune system reacts by replacing said lesions with scar (sclerotic) tissue. Hence, the disease is known as multiple sclerosis (Reisner & Reisner, 2017). MS is considered a disease of young adults and generally occurs before the age of 15; MS after 40 years of age is considered rare (Reisner & Reisner, 2017). Symptoms include intermittent acute neurologic aberrations (dependent on location and degree of demyelination) followed by remission, and such a pattern can continue for several years. In time, the action potential disturbances from myelin scarring become permanent as the number of lesions grows in number (Reisner & Reisner, 2017). MS is also considered an autoimmune disease, with the possibility of initiation through viral delivery, and is thought to develop in genetically predisposed individuals with abnormal/compromised immune systems (Reisner & Reisner, 2017). Having considered the nature and manifestations of MS, the following will consider nutritional interventions to help manage such a disease.

It has been postulated that gluten (a protein found in wheat, barley, and rye) may “appear” like other antigens the immune system attacks under normal circumstances (considered a molecular mimic) (Mokarizadeh et al., 2015). As such, gluten may serve as an antigenic impetus of MS. Mokarizadeh et al. (2015) provided other examples to help support their hypothesis; in gluten sensitivity, antibodies were produced against α-gliadin 33-mer peptide (protein found in gluten) and was shown to react with neural antigens such as asialoganglioside (component of nerve cell membranes), synapsin (protein found in nerve axons), and myelin basic protein (within the structure of myelin sheath). Although such evidence does not directly determine the cause of MS itself, it does show an unfavourable interaction of gluten proteins upon nerve fibres, which could be involved in MS, although further research must be performed to support, or refute, such a hypothesis.

In conclusion, if gluten has been shown to induce an immune response in some individuals, elimination of such foods might be a simple and cost-effective strategy for those with MS, as it carries little risk. Additionally, since many foods exist today devoid of gluten, such a nutritional modification would require little effort to incorporate on behalf of an individual afflicted with MS.
References
Mokarizadeh, A., Esmaeli, P., Soraya, H., Hazzanzadeh, K., Jalili, A., Abdi, M., & Faryabi, M. R. (2015). Antibody against α-gliadin 33-mer peptide: Is the key initiating factor for development in multiple sclerosis during gluten sensitivity? Journal of Medical Hypothesis, 9(1), 38-44.
Reisner, E. G., & Reisner, H. M. (2017). An introduction to human disease: Pathology and pathophysiology correlations (10th ed.). Burlington, MA: Jones & Bartlett Learning.
-Michael McIsaac
