Multiple sclerosis (MS) is a disease characterized by inflammatory, demyelinating, and autoimmune events affecting more than 2 million people worldwide (Reich, Lucchinetti, & Calabresi, 2018).Brum, Comini-Frota, Vasconcelos, and Dias-Tosta (2014) stated that although the etiology of multiple sclerosis (MS) has not been clearly uncovered, there does exist environmental and genetic factors thought to manifest the disease. Such factors included smoking, some viruses, and low vitamin D levels (25-hydroxyvitamin D). As such, the following will explore the same with particular emphasis on low vitamin D levels and its relationship to MS.
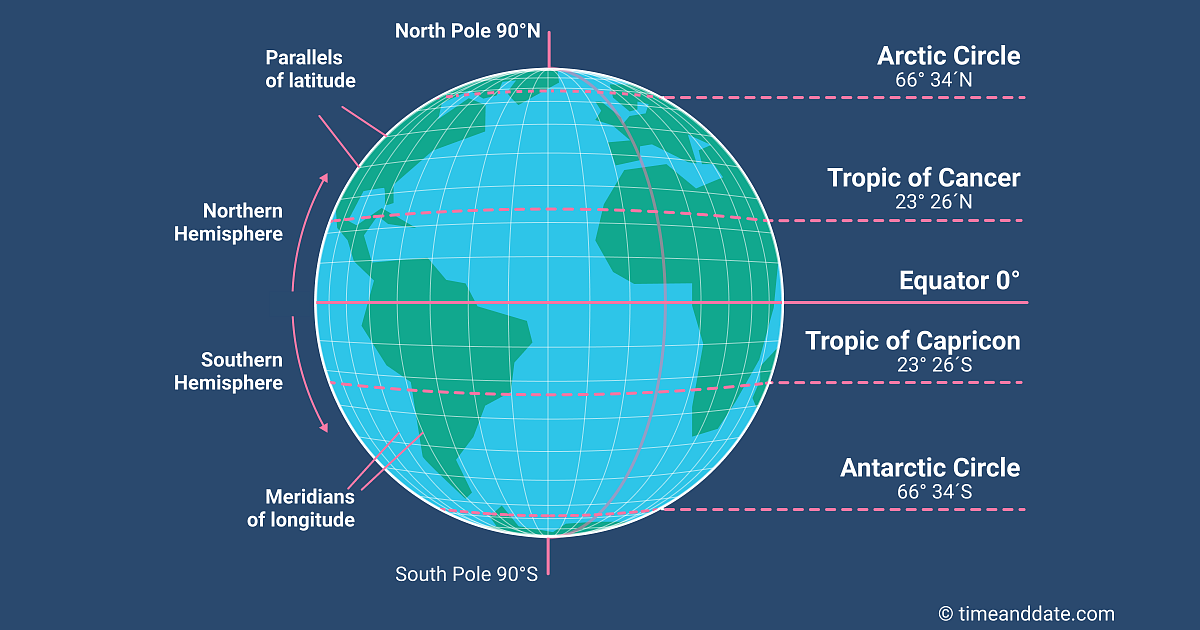
Interestingly, as populations move further from the equator, incidences of MS increase; the northern hemisphere is particularly characterized by its high rate of MS, especially among Caucasians (Brum et al., 2014). The relationship between distance from the equator and MS is thought to be related to MS, in part, to low solar radiation and general low vitamin D (via serum analysis) levels in said population. Brum et al. (2014) presented several studies that considered vitamin D3 (of differing doses)and its affect upon biomarkers such as bone mineral density, relapse rates, disease progression, and lesion growth. All studies indicated no change in said biomarkers except a reduction in gadolinium enhancing lesion; a substance that detects the presence of disrupted myelin sheaths (Brum et al., 2014).
Considering the above results, it should be stated that the studies reviewed by Brum et al. (2014) had limitations: some studies used lower doses of vitamin D3(i.e., 3000 IU/day), other studies had low sample sizes (i.e., 25 participants in intervention and control groups), while other studies used high doses of vitamin D (12,000 IU/day). Due to the lack of homogeneity in study designs, Brum et al. (2014) suggested the need for double blind, randomized, controlled trials (RCTs) with large control and intervention groups that analyze key biomarkers: bone mineral density, relapse rates, disease progression, and lesion growth.

Although more refined studies need to be constructed to validate vitamin D3 dosing and its relationship to MS biomarkers, evidence continues to support the need to reach optimal levels of 25-hydroxyvitamin D for overall health, despite the presence or absence of MS. Optimal 25-hydroxyvitamin D levels should be ≥30ng/ml since levels <20ng/ml is considered insufficient and is associated with an increased risk for immune, metabolic, and neoplastic disorders (Brum et al., 2014; Rosen, 2011). Individuals can slowly increase daily levels while monitoring 25-hydroxyvitamin D to avoid exceeding 70ng/ml; a level considered excessive (Rosen, 2011).
In conclusion, MS is a disease characterized as an inflammatory, demyelinating, autoimmune condition which affects more than 2 million people worldwide. As such, it is reasonable to monitor 25-hydroxyvitamin D levels in said population and titrate supplemental vitamin D3 until ≥30ng/ml has been ascertained in the serum. Although such an intervention may not, as a stand-alone modality, significantly change outcomes with the MS population, it may find its place within a larger intervention that considers the underlying impetus behind the autoimmune response, that is central to the disease.
References
Brum, D. G., Comini-Frota, E. R., Vasconcelos, C. C. F., & Dias-Tosta, E. (2014). Supplementation and therapeutic use of vitamin D in patients with multiple sclerosis: Consensus of the scientific department of neuroimmunology of the Brazilian academy of neurology. Arq Neuropsiquiatr, 72(2), 152-156.
Reich, D. S., Lucchinetti, C., & Calabresi, P. A. (2018). Multiple Sclerosis. The New England Journal of Medicine, 378(2), 169-180.
Rosen, C. J. (2011). Vitamin D Insufficiency. The New England Journal of Medicine, 364(3), 248-254.
Rosen, L. N., Livingstone, I. R., & Rosenthal, N. E. (1991). Multiple sclerosis and latitude: A new perspective on an old association. Medical Hypothesis, 36(4), 376-378.
-Michael McIsaac
