Constipation is a condition that falls under a broader term known as irritable bowel syndrome (IBS); a disorder that negatively affects millions of people, globally.1 IBS with constipation (IBS-C) can be caused by multiple factors, ultimately presenting as slowed gut motility, gas, and bloating.1(39),2 Left unmanaged, IBS-C can create psychological burdens, affect relationships, lower physical productivity, and decreases the individual’s quality of life.3 Thus, it is imperative to both diagnose IBS-C and develop interventions to restore and support normal gut function. As such, the following will explore the same.
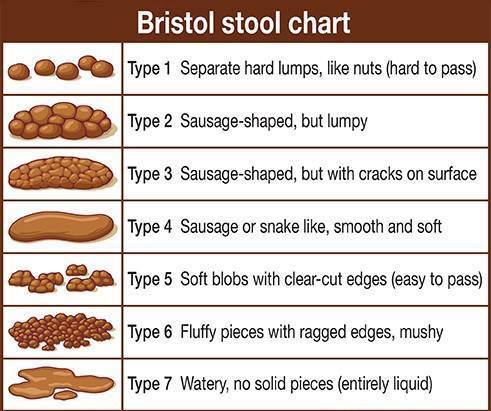
Constipation can be characterized by recurrent abdominal pain for a minimum of 3 days per month within a 12-week period, hard/lumpy stools, incomplete evacuation, less than 3 defecations/week, and straining while defecating.4 Thus, if an individual experiences such outcomes, the presence of IBS-C is likely. Physiologically, normal gut motility is induced by a cyclic pattern known as the major migrating complex; an event characterized by periodic luminal contractions, which drives contents within the small intestine from the stomach towards the large intestine.1(40) However, patients with IBS-C have aberrations in such contractions.
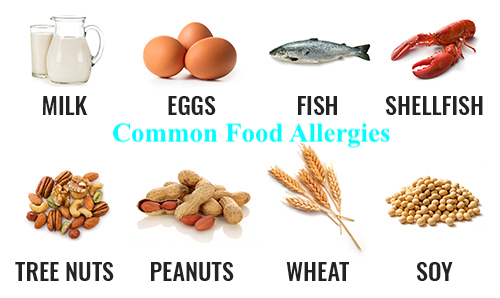
As mentioned previously, IBS-C can originate from multiple factors to include allergic reactions to particular foods.5 Such a submission is supported by studies (300 subjects) in which chronic constipation was tightly associated with protracted colonic transit times, and the presence of IgE-mediated (a measure of allergic activity) food allergies; subjects without food allergies tended to have typical transit times.5(1299) As such, if an individual has IBS-C, food allergy testing can provide the opportunity to elucidate foods, which indicate allergic reactions. If particular foods are determined as problematic, removal of said foods from the diet would be a logical first step intervention.
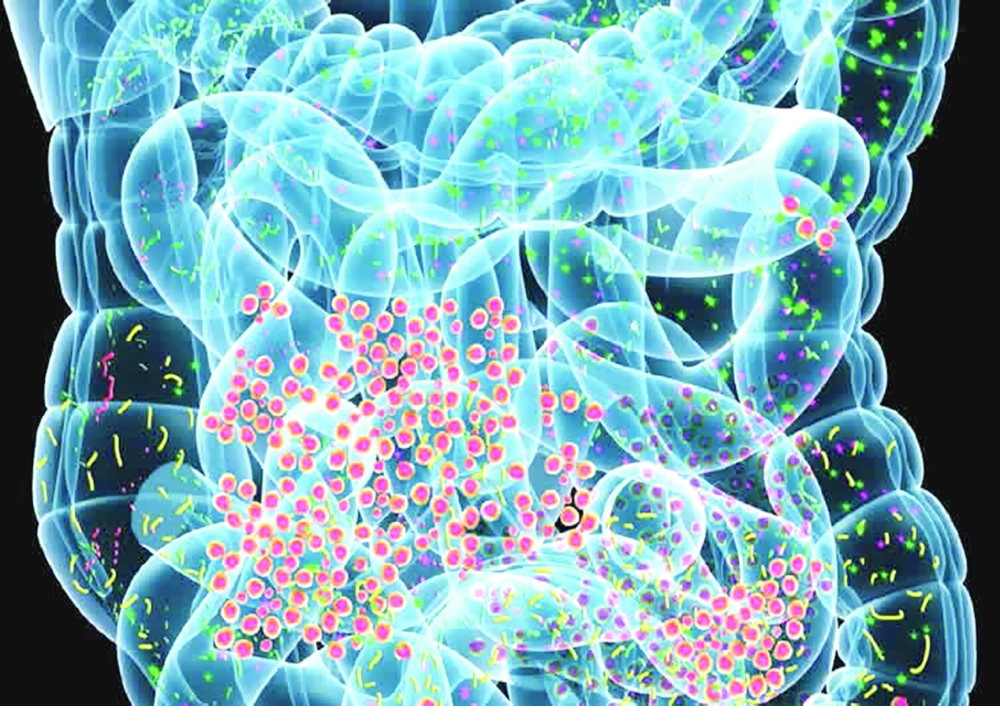
Once food allergies are addressed, another step in managing IBS-C would include analysis of the microbiome. As mentioned in this author’s previous posts, the gastrointestinal tract (GIT) is the home and breeding ground for many microbes. Dysbiosis is a condition defined by a disruption in the number and ratio of microorganisms (known as the microbiome) in the large and small intestine.6 Such microorganisms include parasites/bacteria/fungus/viruses, and imbalances between the same have been linked to reduced immune/barrier function, altered nutrient digestion/absorption.7(447)8

**You will notice some “foods to eat” are considered good options to control fungal overgrowth. However, constipation is multifactorial, and can also be driven by allergies (mentioned previously). This means a low carbohydrate option (i.e., eggs) that starves Candida could still drive an allergic reaction (if present), promoting constipation. This is why allergy tests can help refine low carbohydrate food choices, if Candida is also present**
If an individual has a stool test that indicates an overabundance of fungal species, such as Saccharomyces spp, one step might be reducing nutrients that feed said microbe. Evidence suggests that fungus tends to proliferate in carbohydrate-rich mediums.7(446) Thus, reducing foods high in sugar/starchy carbohydrates would likely slow the growth of fungus. Furthermore, testing levels of other bacterial species, to include Lactobacillus, would be useful; low levels of Lactobacillus can allow the overgrowth of fungal microorganisms.8 Conversely, optimal levels of said bacteria would produce hydrogen peroxide; a substance known to slow fungal proliferation.8(3) If Lactobacillus levels are below range, supplementation of the same can facilitate return to optimal levels.

**Remember that high fibre foods, which facilitate production of SCFAs, must also be considered/selected in the context of other biomarkers (i.e., food allergies and dysbiosis-Candida) that might be present**
Analysis of short chain fatty acids (SCFAs) could be another means of improving gut health and overall digestion. SCFAs are formed from bacterial fermentation of high fiber dietary carbohydrates and amino acids that escape absorption within the small bowel.7(451) SCFAs are generally well absorbed by colonocytes (colon cells) and provide a substantial source of energy for the same.7(451) Thus, changes in the proportion of SCFAs can signify an aberrant state of colonic health. If butyrate is above normal ranges, for example, such outcomes have been associated with obesity and calorie-rich diets.9 Furthermore, higher SCFA levels in general have been associated with indicators of lower gut microbiota diversity, and higher gut permeability.9(11)
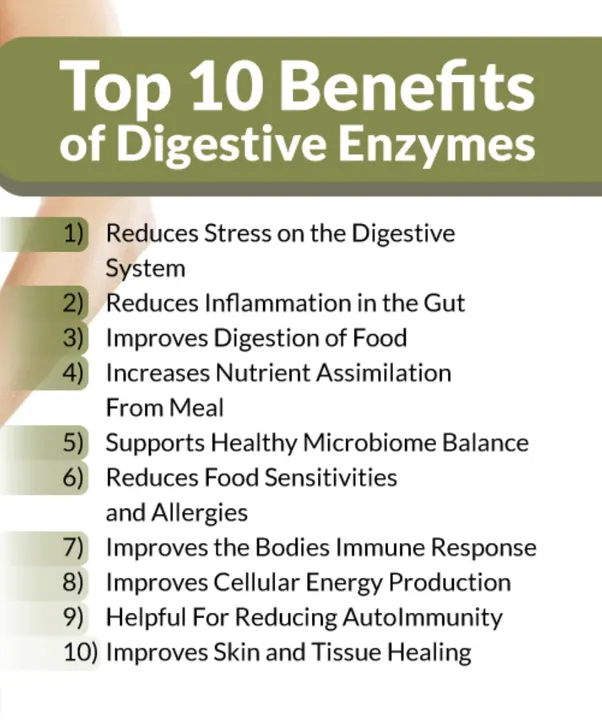
High levels of butyrate can also be a sign of protein maldigestion from pancreatic enzyme insifficiency.7(452) Such a condition could help explain the presence of high butyrate levels. One intervention to consider if butyrate levels are high, might be the introduction of exogenous digestive enzymes rich in chymotrypsin/trypsin (digests proteins), amylase (digests carbohydrates), and lipase (digests fats) which plays an integral role in the breakdown of larger food particles into its constituents.10 Such an intervention would be further supported if stool samples also indicated high levels of putrefactive SCFAs; a process that occurs from undigested protein and subsequent bacterial fermentation of the same.

In conclusion, IBS-C can be caused by multiple factors, ultimately presenting as slowed gut motility, gas, and bloating.Left unmanaged, IBS-C can create psychological burdens, affect relationships, lower physical productivity, and decrease an individual’s quality of life. However, protocols do exist which can identify foods and microorganisms that exacerbate IBS-C. Furthermore, additional tests can help elucidate deficiencies in other microorganisms and digestive enzymes that, when returned to normal ranges, can help improve digestion, absorption, overall gut function, and motility. Ultimately, such holistic approaches can help support digestive homeostasis, health, and overall quality of life.
References
1. Aragon G, Graham DB, Borum M, et al. Probiotic therapy for irritable bowel syndrome. Gastroenterol Hepatol. 2010;6(1):39-44. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2886445/. Accessed February 25, 2020.
2. Ross H. Constipation: Cause and control in an acute hospital setting. Br J Nurs. 1998;7(15):907-913. doi:10.12968/bjon.1998.7.15.5621.
3. Zeng Y, Liu Y, Liu Z. Initial effects of electroacupuncture for chronic severe functional constipation and the potential underlying factors: Secondary analysis of a randomized controlled trial.Evid Based Complement Alternat Med. 2019. doi:https://doi.org/10.1155/2019/7457219.
4. Bahrudin, MF, Rani RA, Tamil AM, et al. Effectiveness of sterilized drink containing lactobacillus helveticus comparable to probiotic alone in patients with constipation-predominant irritable bowel syndrome.Dig Dis Sci. 2019. doi:https://doi-org.libproxy.bridgeport.edu/10.1007/s10620-019-05695-3.
5. Carroccio A, Iacono G. Review article: Chronic constipation and food hypersensitivity-An intriguing relationship. Ailment Pharmacol Ther. 2006;24(9):1295-1304. doi:10.1111/j.1365-2036.2006.03125.x.
6. Huang L, Gao R, Yu N, et al. Dysbiosis of gut microbiota was closely associated with psoriasis. Sci China Life Sci. 2019;62(6):807-815. doi:10.1007/s11427-018-9376-6.
7. Lord RS, Bralley, JA. Laboratory Evaluations for Integrative and Functional Medicine. 2nd ed. Duluth, GA: Genova Diagnostics; 2012.
8. Erdogan A, Rao SSC. Small intestinal fungal overgrowth.Curr Gastroenterol Rep. 2015;17(4):1-7. doi:10.1007/s11894-015-0436-2.9.
9. Cuesta-Zuluaga J, Mueller NT, Alvarez-Quintero R, et al. Obesity, hypertension, and cardiometabolic risk factors. Nutrients. 2019;11(51):1-16. doi:10.3390/nu11010051.
10. Pagana KD, Pagana TJ. Manual of Diagnostic and Laboratory Tests. 5th ed. St. Louis, MO: Mosby; 2014.
-Michael McIsaac
