Sedentary behavior and a general overconsumption of calories, especially from processed foods, are primary drivers for overweight/obesity.1,2 Such changes can be identified and tracked by implementing a measure known as body mass index (BMI); a metric relating weight (kilograms) divided by height (metres2) to normative values.3 Other biomarkers that provide meaningful insight into an individual’s health status can include high-density lipoprotein cholesterol concentrations (HDL-C), triglycerides, non HDL-C, c-reactive protein (CRP), fasting glucose concentrations, alkaline phosphatase (ALP), and hemoglobin A1C (HBA1C). As a means of appreciating such measures and their relationship to overweight/obesity and general health, the following will explore the same. Furthermore, nutritional recommendations will be provided to help improve said biomarkers.
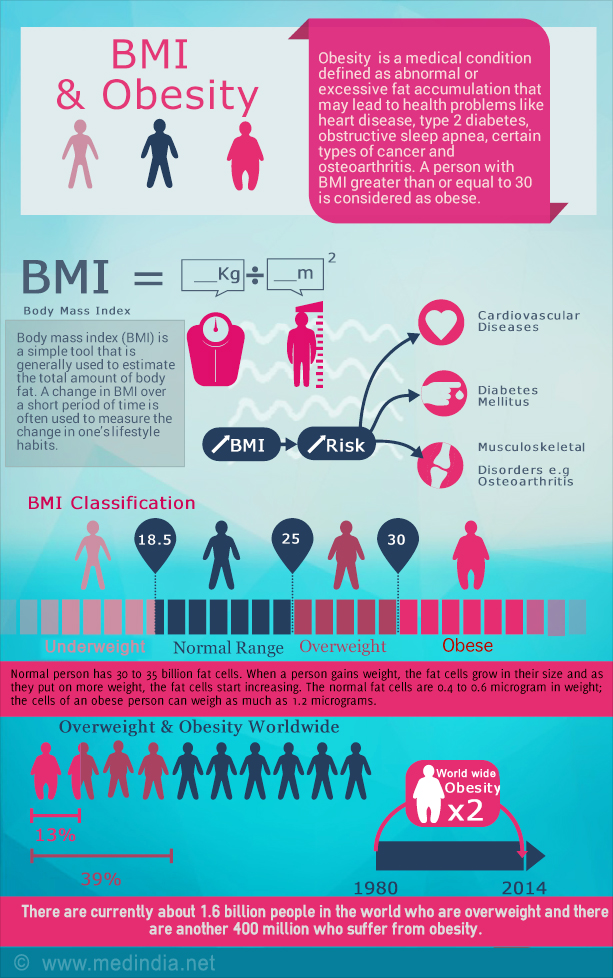
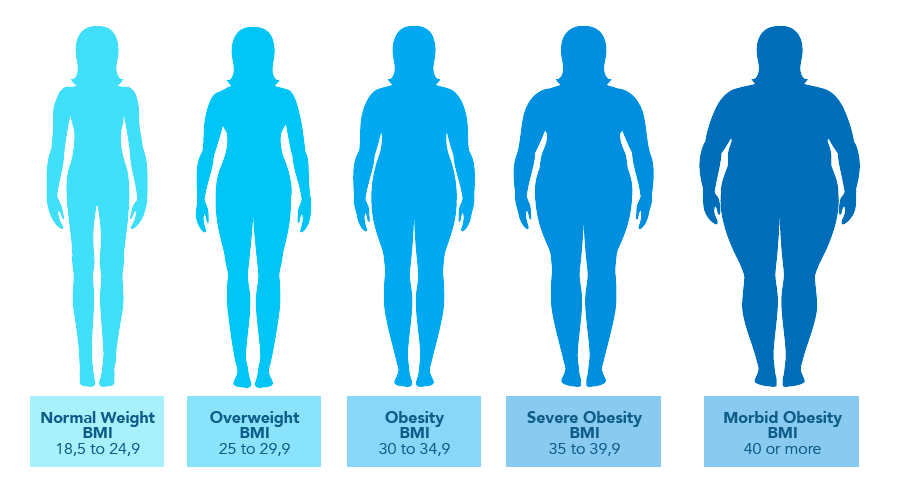
A state of overweight can be defined as ≥ 25 kg m2 and obesity as BMI ≥ 30 kg m2.3(684) If an individual is 200 lbs (91 kg) and 5’11” (1.8 m) the result would be 27.9; such a result suggests the individual is overweight. Essentially, BMI is a convenient and reliable measure of obesity/adiposity, especially when used in conjunction to other markers mentioned in the previous section. For example, if an individual has low HDL-C/high triglycerides/high non HDL-C/high CRP/high fasting glucose/high ALP/high HBA1C, such a combination of above-range values, especially if left unmanaged, are likely to become drivers of deeper health conditions. The following will consider each marker in greater detail.
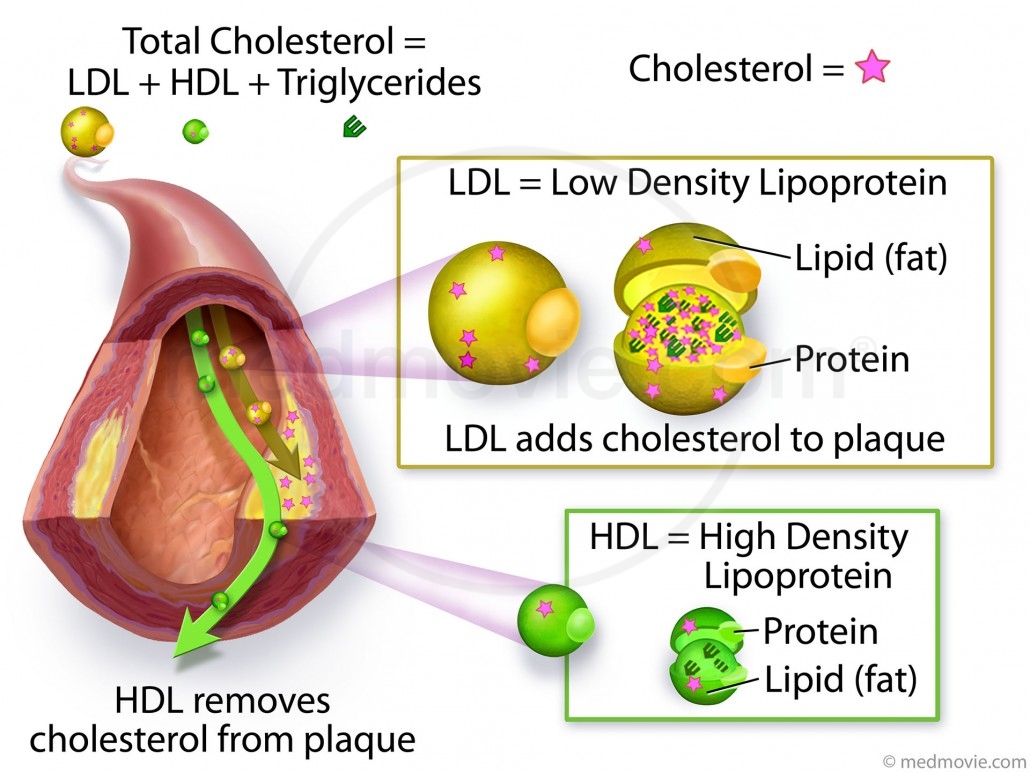
As mentioned in previous posts, HDLs assist in reverse transport of cholesterol moving said molecule from peripheral tissues towards the liver.5 If an individual has a HDL-C of 26 mg/dL, said result would be below the target of 40 mg/dL. Such a result compromises the ability of the body to keep cholesterol levels at normal values along peripheral tissues. Low HDL-C is further complicated by elevated triglycerides; such molecules, especially when in abundance, share a close relationship to low-density lipoproteins (LDLs).6 Specifically, when triglycerides are above normative ranges, they tend to have a strong association with high levels of very low-density lipoproteins (VLDLs) and LDLs.6(1) The following will consider the same in greater detail and the relationship to atherogenic states.
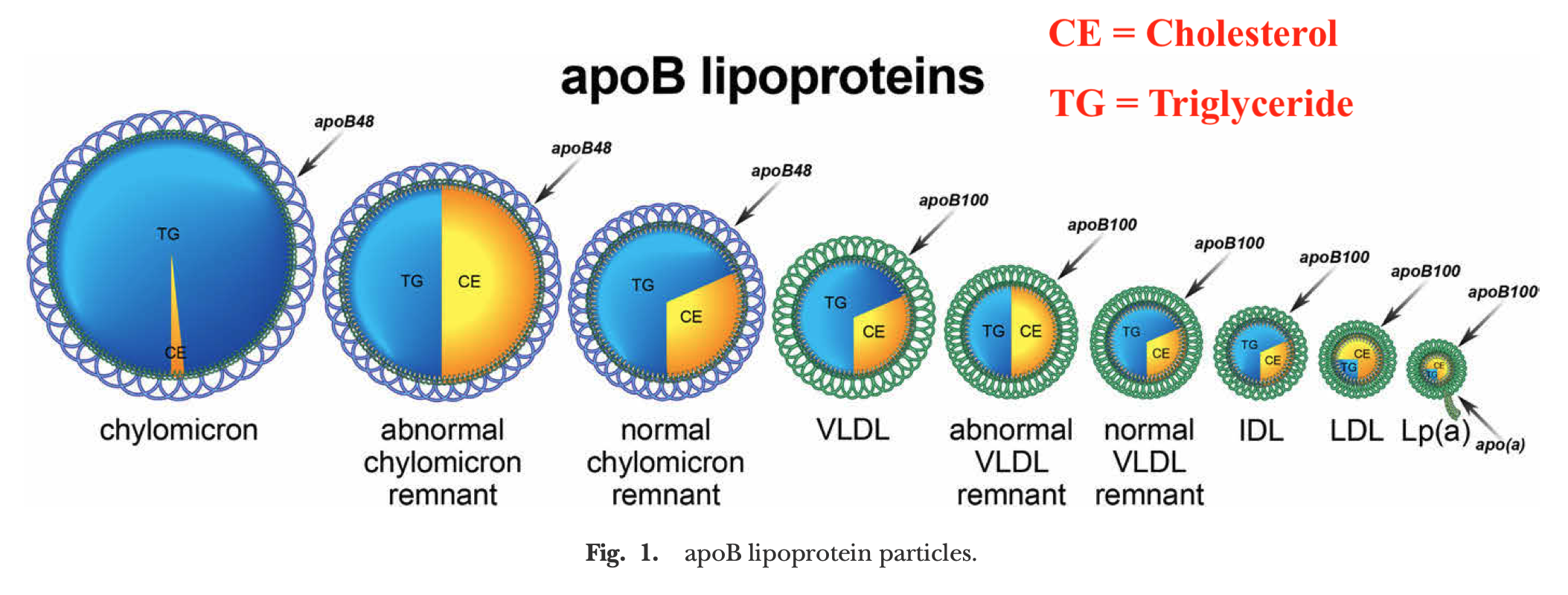
When fatty acids from food are absorbed from the intestine, they are converted to triglycerides that are encapsulated by larger particles known as chylomicrons. Chylomicrons transport dietary triglycerides, and cholesterol, to peripheral tissues and the liver.7 Furthermore, the size of chylomicrons varies depending on the amount of fat ingested.7 After the triglycerides from chylomicrons are metabolized by muscle and adipose tissue, chylomicron remnants (atherogenic), now rich in cholesterol, are formed and absorbed by the liver.7
If individuals consume excessive levels of carbohydrates, the liver will convert said glucose into triglycerides; a process that initiates the endogenous lipoprotein pathway, and emergence, of VLDLs.8 When triglyceride production from the liver is increased, VLDLs are formed to transport said triglycerides to peripheral tissues.7 Once depleted of triglycerides, VLDLs are converted into cholesterol-rich particles known as intermediate low-density lipoproteins (LDLs), also atherogenic in nature. Thus, excessive triglyceride production, especially from carbohydrates, produces chylomicron remnants, VLDLs, and IDLs; all of which are atherogenic, and measured by non HDL-C.7
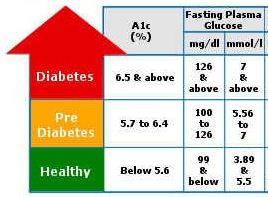
Fasting glucose measures that are high are also telling of the body’s ability to properly manage and store glucose. IR is defined as a decreased biological response to a certain concentration in insulin.9 Said impairment of insulin action comprises both reduced insulin responsiveness, and insulin sensitivity. Several mechanisms can induce IR by interfering with the insulin signalling process such as hyperglycemia, elevated blood lipids , amino acids, and hyperinsulinemia.9(1) IR is also supported by elevated HBA1C, which is an average glucose level concentration within the red blood cell over 3 months.
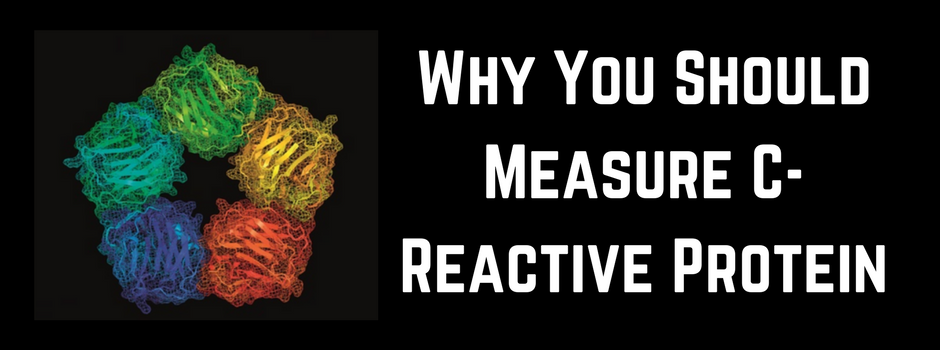
Elevated CRP is an indicator of inflammation resulting from innate or acquired immunity, driven by the presence of external and/or internal changes in the body.10 CRP is synthesized by hepatocytes (liver cells) in a response to acute or chronic inflammation.10(1) Furthermore, CRP is an acute phase protein and inflammatory marker strongly associated with developmental diseases such as cancer, heart disease, and diabetes.10(1) Such an elevation, especially when considering simultaneous elevation in fasting glucose and elevated lipids, places individuals at increased risk for said diseases.
Elevated ALP is an indicator of compromised liver function.11 The most relevant value in measuring serum ALP lies in the diagnosis of cholestatic liver disease (decrease of bile flow from liver), non-alcoholic fatty liver disease, or liver injury.11,12 As such, elevated values should encourage one to consider possible causes of elevated enzymes and further differential diagnosis to elucidate the mechanism behind said rise. Other contributing factors that may tax liver function, according to Bayard et al12(1963) could include disordered lipid metabolism (elevated lipids), IR (suspected from the client’s readings), and potential toxic exposures.

Solutions to mitigate such elevated measures could include decreasing refined/processed carbohydrates; substances known to increase the incidence of elevated fasting glucose levels, elevated lipids, and increased IR.13 Furthermore, this author would suggest increased protein consumption to induce satiety. Protein consumption exerts its satiety-inducing effects by increasing the flow and release of satiety hormones, increasing concentrations of amino acids, increasing energy expenditure, and inducing gluconeogenesis.14

CRP levels could be further reduced by increasing intake of omega-3 rich foods such as fish and omega-3 supplementation at a minimum of 3000 mg/day.15 Reduction of omega-6 rich foods, often seen in processed foods and vegetable oils, would also be advised as they are pro-inflammatory fats.16 Instead, this author would encourage the consumption of a wide array of vegetables as a means of providing polyphenols, antioxidants, and fiber of which could help reduce the client’s dyslipidemic state. Additional use of olive oil with cooking and meals would be encouraged as said oil helps down regulate LDL-C, glucose levels, and inflammatory cascades within the body.17 Avocado oil would also be encouraged as it contains oleic acid (like olive oil) and other fatty acids that help reduce incidence of cardiovascular disease.18
In conclusion, sedentary behavior and a general overconsumption of calories, especially from processed foods, are primary drivers for overweight/obesity and other associated diseases. Slowly removing the consumption of processed foods, rich in sugars/carbohydrates/omega-6 fatty acids, can help modify and improve many biomarkers key to protecting health and longevity. Careful consideration of the client’s signs, symptoms, nutritional habits, and blood chemistry panels can facilitate meaningful changes through diet and lifestyle interventions. Furthermore, when and where indicated, supplementation can help expedite improvements in biomarkers, especially where severe deficiencies are noted.
References
1. Ifland JR, Preuss HG, Marcus MT, et al. Refined food addiction: A classic substance use disorder. Med Hypotheses: 2009;72:518-526. doi:10.1016/j.mehy.2008.11.035.
2. Bureau of Labor Statistics (2018). American time use survey-2018 results.http://www.bls.gov/news.release/pdf/atus.pdf. June 19, 2019. Accessed September 24, 2019.
3. He W, Lei Q, Yang M. Lower BMI cut-offs to define overweight and obesity in China.Obes. 2015;23(3):684-691. doi:10.1002/oby.20995.
4. Lee RD, Nieman DC.Nutritional Assessment. 6th ed. New York, NY: McGraw-Hill. 2013.
5. Gropper SS, Smith JL, Carr, TP. Advanced Nutrition and Human Metabolism.7th ed. Boston, MA: Cengage Learning; 2018.
6. Lemanski PE. Beyond Routine Cholesterol Testing: The Role of LDL Particle Size Assessment./courses/1718508/files/100458566/download Accessed January 15, 2020.
7. Feingold KR, Grunfeld C. Introduction to lipids and lipoproteins. Endotext. https://www.ncbi.nlm.nih.gov/books/NBK305896/. Updated February 2, 2018. Accessed January 20, 2020.
8. Freeman MW, Walford GA. Very low-density lipoproteins. Science Direct website. https://www.sciencedirect.com/topics/neuroscience/very-low-density-lipoprotein. Accessed January 30, 2020.
9. Moscoso-Vasquez M, Colmegna P, Sanchez-Pena RS. Control-oriented model including hyperinsulinemia induced resistance in type 1 diabetes. IEEE. 2019;1-6. doi: 10.1109/CCAC.2019.8920846.
10. Rosyadi I, Ramadhona E, Wahono ATU. Acute phase c-reactive protein as early detection of type 1 diabetes mellitus. IEEE. 2018;1-4. doi:10.1109/BIOMIC.2018.8610567.
11. Lowe D, John S. Alkaline Phosphatase. NCBI website. https://www.ncbi.nlm.nih.gov/books/NBK459201/. Updated December 21, 2018. Accessed January 30, 2020.
12. Bayard M, Holt J, Boroughs E. Non-alcoholic fatty liver disease. Am Fam Physician. 2006;73(11):1961-1968.
13. Fernando DH, Forbes JM, Angus PW, et al. Development and progression on non-alcoholic fatty liver disease: The role of advanced glycation end products.Int JMol Sci. 2019;20(20):1-19. doi:10.3390/ijms20205037.
14.Morell P, Fiszman S. Revisiting the role of protein-induced satiation and satiety.Food Hydrocoll. 2017;68:199-210. doi:http://dx.doi.org/10.1016/j.foodhyd.2016.08.003.
15. Kohlstadt I. Advancing Medicine with Food and Nutrients. 2nd London, NY: CRC Press; 2012.
16. Ilich JZ, Kelly, OJ, Kim Y, et al. Low-grade chronic inflammation perpetuated by modern diet as a promoter of obesity and osteoporosis. Arh Hig Rada Toksikol. 2014;65(2),139-148. doi: 10.2478/10004-1254-65-2014-2541.
17. Mohsen G, Khaneghah AM, Lorenzo JM, et al. Health benefits of olive oil and its components: Impacts on gut microbiota, antioxidant activities, and prevention of non-communicable diseases.Trends in Food Science and Technology. 2019;88:220-227. doi: 10.1016/j.tifs.2019.03.008.
18. Tan CX. Virgin avocado oil: An emerging source of functional fruit.J Funct Foods. 2019;54:381-392. doi:https://doi.org/10.1016/j.jff.2018.12.031.
-Michael McIsaac
