The gastrointestinal tract (GIT) is an estimated 7 m long organ with a surface area of approximately 300 m2.1 The GIT is composed of intestinal epithelium producing a semipermeable barrier preventing entry of pathogens and blocking contact with constituents of the immune system.1 Ultimately, such a system maintains homeostasis, immune function, and digestion/absorption of nutrients. A central component of digestion (i.e., the breakdown of large food particles into smaller ones) is the timely release of gastric acids and digestive enzymes from the pancreas upon the consumption of food.3 However, certain medications and pathologies can create aberrations of such organs, necessitating the use of oral digestive enzymes (ODEs).4,5 As a means of appreciating the effectiveness of said ODEs, the following will explore the same.
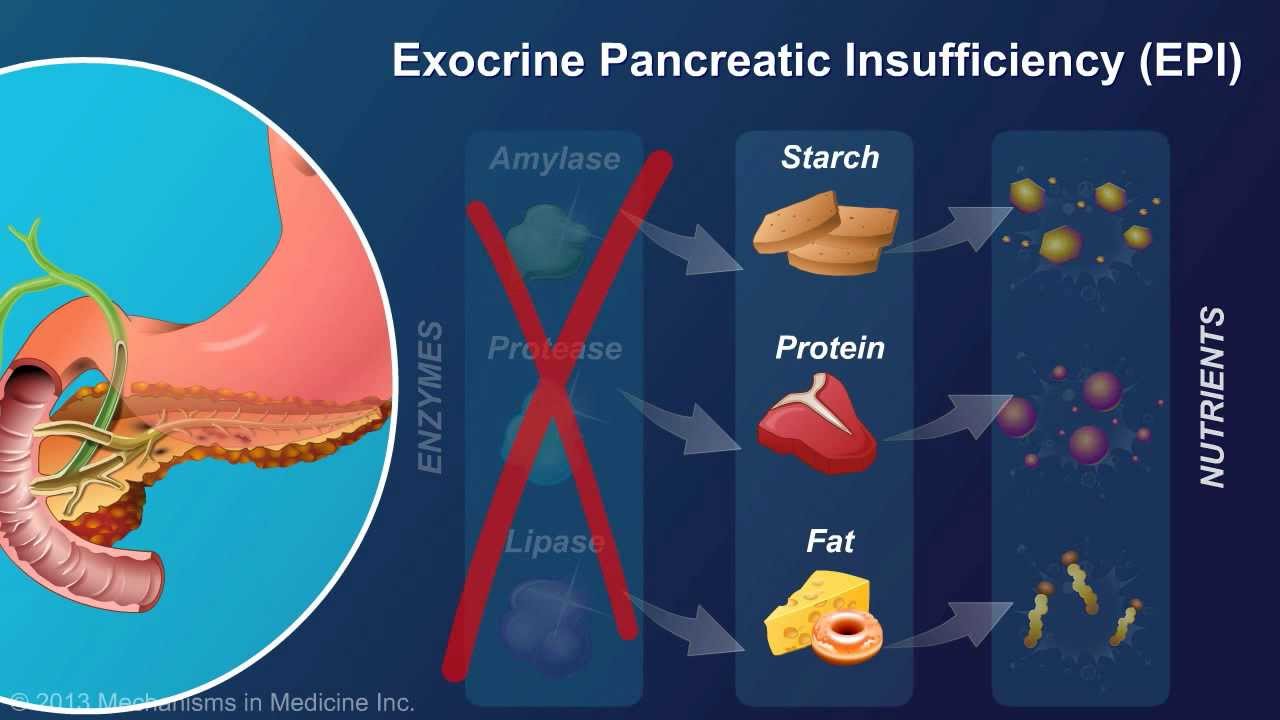
Exocrine pancreatic insufficiency (EPI) is a condition which prevents the pancreas from synthesizing enough pancreatic enzymes to successfully digest food.4 Furthermore, EPI can be difficult to recognize, and diagnose, since many of its symptoms and signs tend to overlap with other gastrointestinal maladies.4(41) EPI can emanate from several sources to include pancreatitis, pancreatic resection, and cystic fibrosis. However, EPI can also be induced by history of pancreatic cancer, pancreatic obstruction, celiac disease, Chron’s disease, gastric surgery, and short bowel syndrome.4(42) Ultimately, many conditions can lead to pancreatic dysfunction. Most relevantly, EPI can produce multiple downstream pathophysiological aberrations which can directly affect an individual’s activities of daily living, health, and overall quality of life. The following will consider such systemic manifestations from EPI.
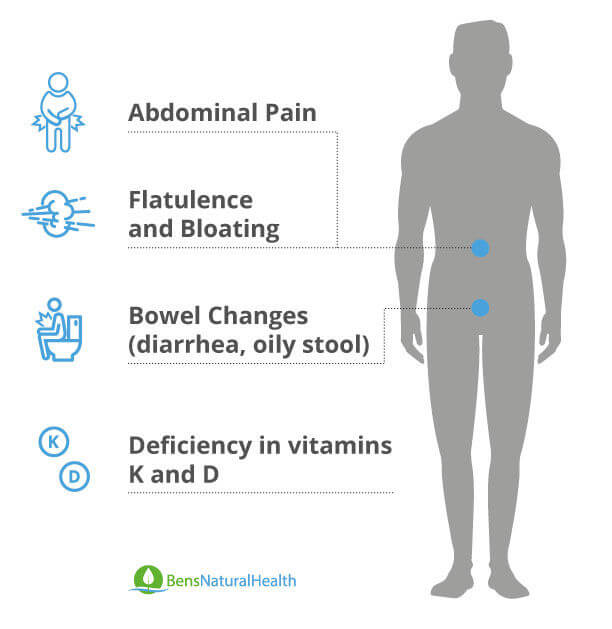
The prevalence of EPI with comorbidities are as follows: pancreatic cancer (50%), advanced cystic pancreatitis (85%), cystic fibrosis (85%), celiac disease (30%), and diabetes mellitus (40%).4(42) Clinical manifestations of EPI can include indigestion, abdominal cramping, bloating, foul smelling feces/flatulence, excess fat in feces (steatorrhea), and weight loss.4(42) Other clinical manifestations of EPI can include malabsorption of fat-soluble vitamins such as K, E, D, and A. Left unmitigated, vitamin deficiencies such as low vitamin A can lead to night blindness while low vitamin D can decrease intestinal absorption of calcium and phosphorus which can lead to bone demineralization/osteopenia/osteoporosis.4(42) Low vitamin E can place individuals with EPI at a higher atherosclerosis, fatigue, and loss of muscle tone while low vitamin K can induce excessive bleeding.4(42) Having considered signs/symptoms of EPI, the following will explore oral supplementation of digestive enzymes as a means pf managing said condition.
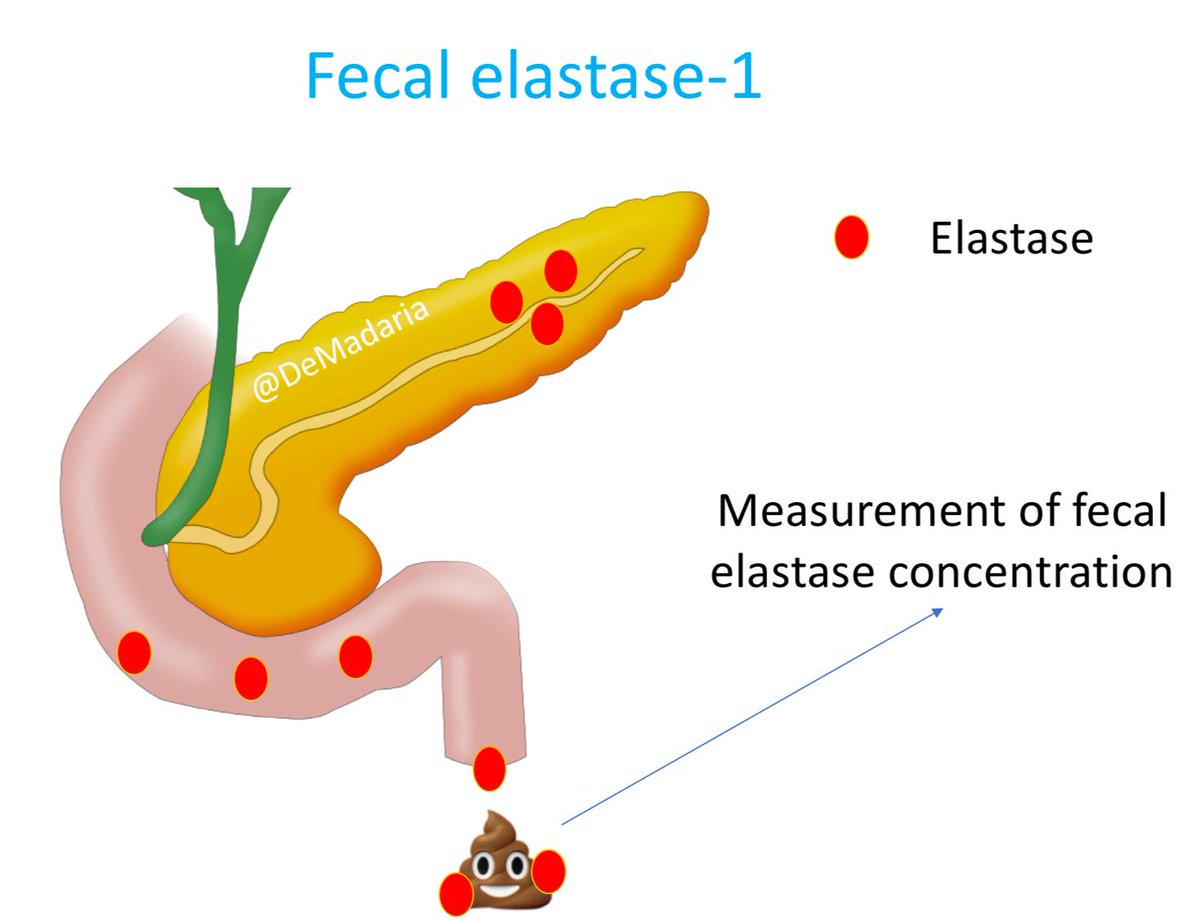
Once EPI has diagnosed using tests outlined in this author’s previous posts (i.e., fecal elastase-1 enzyme, fecal fat tests), it is essential to reintroduce digestive enzymes.3(420-422) Such a process is also known as pancreatic enzyme replacement therapy (PERT) and its implementation is intended to improve nutritional status thereby positively affecting body mass index (BMI), enhance fat soluble vitamin absorption, and improve gastrointestinal symptoms associated with EPI.5 Ultimately, PERT is the sole therapy for treating EPI and works by providing sufficient enzymes that would otherwise emanate from the pancreas such as lipase (breaks down fats), amylase (breaks down sugars), and protease (breaks down proteins).5(22) Ooi et al5(22) noted that there are different formulations and strengths of oral supplements available on the market, and timing of PERT is crucial for maximal enzyme effectiveness. The following will explore dosing and evidence of efficacy of the same in greater detail.

Ingestion of 25000-40000 units of lipase (sometimes as high as 75000-80000 units) is generally recommended for adults during main meals of the day, with half of said dose used for snacks.5(22) If infants/children are suffering from EPI, 500-4000 units of lipase per gram of dietary fat is used, while 500 units/kg bodyweight is used for children between 4 and 17 years of age.5(22) Evidence suggests that PERT can help improve fat absorption, stool consistency, and frequency when compared to a placebo, though said intervention and related studies indicated that patients with EPI might not completely mitigate steatorrhea when present.5(22) Other studies reviewed by Ooi et al5(23) indicated that individuals with chronic pancreatitis and cystic fibrosis found that PERT appeared to improve fat malabsorption, though the delivery system and digestive enzyme brands were not reviewed. Both sets of studies reviewed by Ooi et al5(22) lacked research on optimal timing of digestive enzyme timing indicating a need for future studies to explore the same.
In conclusion, the GIT is an estimated 7 m long organ with a surface area of approximately 300 m2. The GIT is composed of intestinal epithelium producing a semipermeable barrier preventing entry of pathogens and blocking contact with constituents of the immune system. A central component of digestion (i.e., the breakdown of large food particles into smaller ones) is the timely release of gastric acids and digestive enzymes from the pancreas upon the consumption of food. However, individuals with EPI are unable to synthesizine enough pancreatic enzymes to successfully digest food, necessitating the need for PERT. Such interventions have been shown to support and improve digestion/absorption of macronutrients, stool consistency, and stool frequency from PERT, although additional research is required to elucidate optimal dosing times relative to food consumption.
References
1. Pizzorno J, Katzinger J. Clinical Pathophysiology: A Functional Perspective. Coquitlam, BC: Mind Publishing Inc; 2012.
2. Feng Y, Huang Y, Wang Y, et al. Antibiotics induced intestinal tight junction barrier dysfunction is associated with microbiota dysbiosis, activated NLRP3 inflammasome and autophagy.PLOS One. 2019:14(6);1-19. doi:10.1371/journal.pone.0218384.
3. Lord RS, Bralley JA. Laboratory Evaluations for Integrative and Functional Medicine. 2nd ed. Duluth, GA: Genova Diagnostics; 2012.
4. Bellomo TL. Exocrine pancreatic insufficiency: Can this be a cause of your patient’s GI symptoms? Nursing. 2020;50(3): 41-45. doi:10.1097/01.NURSE.0000615080.53435.d5.
5. Ooi YX, Nguyen NQ, Campbell J. Efficacy and safety of pancreatic enzyme replacement therapy in pancreatic exocrine insufficiency: A systematic review. JBI Evidence Synthesis. 2016;14(1):20-30. doi: 10.11124/jbisrir-2016-2507.
-Michael McIsaac
