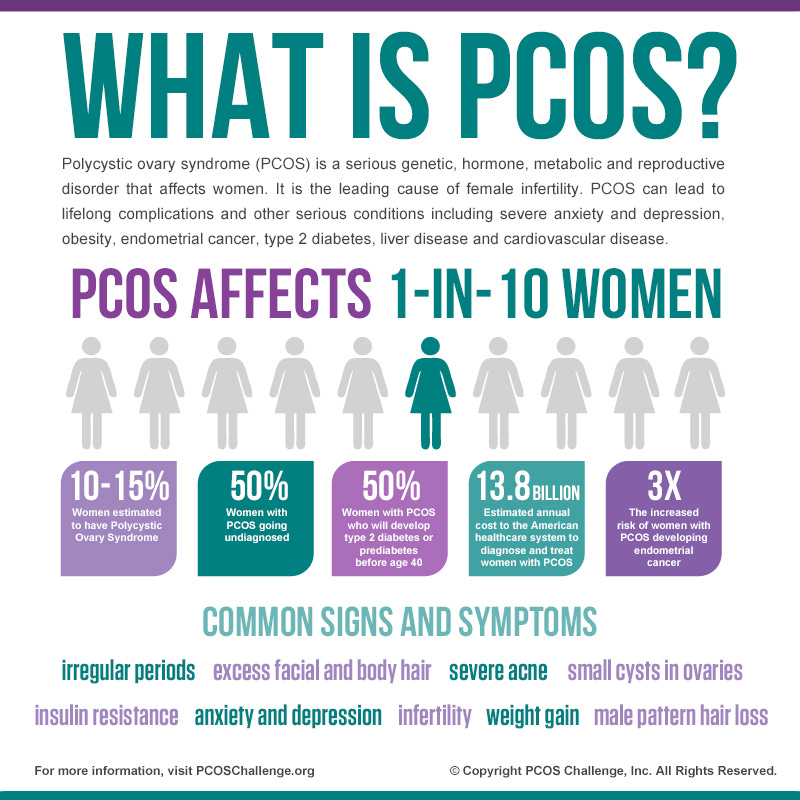
Polycystic ovarian syndrome (PCOS) is an endocrine disorder among women in which 10% of the population is affected within the United States (Reisner & Reisner, 2017). PCOS is often diagnosed among females between 20-40 years of age, and is a prominent cause of anovulatory (no oocytes released during menstruation) infertility. PCOS is characterized by enlarged ovaries containing multiple cysts due to high concentrations of gonadatrophins (regulates normal growth, sexual development, and reproductive function) and is closely associated with obesity, insulin resistance, and diabetes (Reisner & Reisner, 2017). Research indicates that insulin function, or lack thereof, induces the hormonal imbalances, which cause PCOS.
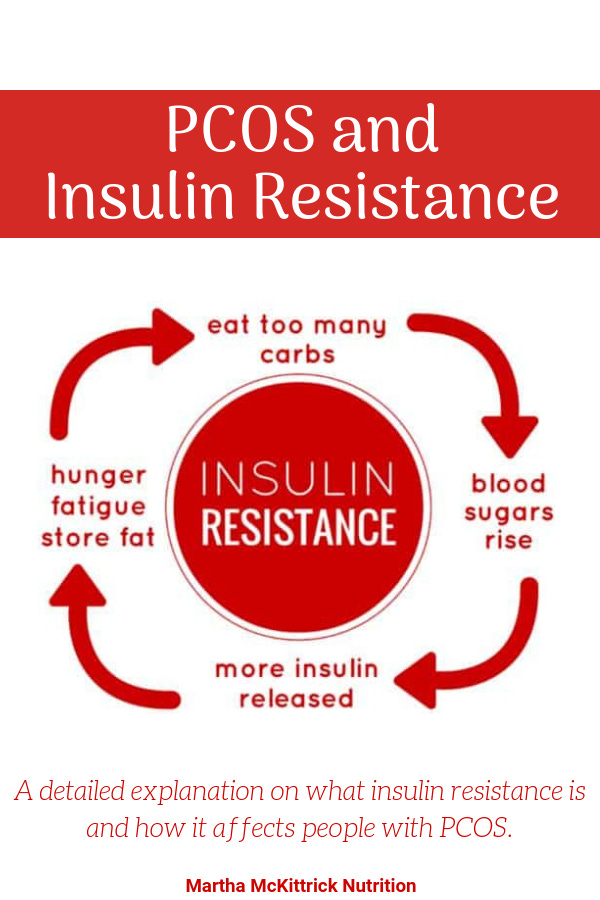
Insulin resistance and the associated hyperinsulinemia affect approximately 65–70% of women with PCOS with 70–80% of obese (BMI > 30) and 20–25% of lean (BMI < 25) women exhibiting said characteristics (Marshall & Dunaif, 2012). Hyperinsulinemia is relevant to PCOS because it appears to cause hyperandrogenemia (excess production of male hormones), inducing excess androgen production; such activities enhance the effect of the increased luteinizing hormone stimulus seen in a majority of women with PCOS (Marshall & Dunaif, 2012).
Additional evidence is also correlating PCOS to other disorders such as glucose intolerance, dyslipidemia, elevated triglycerides, elevated LDL, decreased HDL, and increased chronic systemic inflammation. Colloquially, the aggregate of disorders is known as metabolic syndrome (Marshall & Dunaif, 2012). If excessive insulin production is the cause of PCOS, finding a method to control its production may also provide the answer in controlling the progression of PCOS.

Severity of insulin resistance and hyperinsulinemia can be mitigated and/or eradicated by very low carbohydrate ketogenic diets (VLCKDs). By introducing foods that supply energy (i.e., proteins and fats) but who are also devoid of sugars, insulin response is not required to the same degree, blood sugar concentrations are lowered, and less energy is stored in adipose tissue (Paoli, Rubini, Volek, & Grimaldi, 2013).
Providing lower carbohydrate ingestion induces a change in substrate utilization from one primarily of glucose to fatty acids (ketones-acetoacetate, beta-hydroxybutyrate, acetone) derived from the breakdown of triglycerides (Paoli et al., 2013). Such a process is postulated to help relieve insulin resistance, improve insulin sensitivity, and attenuate hyperinsulinemia (Paoli et al., 2013). Not only can VLCKDs help control insulin resistance, it can also help control several other diseases associated with it (i.e., metabolic syndrome) (Paoli et al., 2013).
References
Marshall, J. C., & Dunaif, A. (2012). Should all women with PCOS be treated for insulin resistance? Fertility and Sterility, 97(1), 18-22.
Paoli, A., Rubini, A., Volek, J. S., & Grimaldi, K. A. (2013). Beyond weight loss: a review of the therapeutic uses of very low-carbohydrate (ketogenic) diets. European Journal of Clinical Nutrition. 67, 789-796.
Reisner, E. G., & Reisner, H. M. (2017). An introduction to human disease: Pathology and pathophysiology correlations (10th ed.). Burlington, MA: Jones & Bartlett Learning.
-Michael McIsaac
